Back
Poster Session C - Monday Afternoon
C0167 - Does Having a Fellow Improve the Quality of Screening Colonoscopy?
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Philip Bouchette, MD
Louisiana State University Health Sciences Center
Shreveport, LA
Presenting Author(s)
Siva Santosh Kumar Gandu, MD1, Philip Bouchette, MD2, Jordan Roussel, MD2, Sudha Pandit, MD3
1LSUHSC-, Shreveport, LA; 2Louisiana State University Health Sciences Center, Shreveport, LA; 3LSUHSC, Shreveport, LA
Introduction: Adenoma detection rate (ADR) is used as a quality metric for physicians performing screening colonoscopies. Many studies use the ADR to assess if different variables affect the quality of colonoscopy. At times, some patients request that a physician in training, a gastroenterology fellow, not be involved in their procedure. This study aims to assess the differences in ADR during screening colonoscopy with and without involvement of the gastroenterology fellow.
Methods: A retrospective review of 243 consecutive screening colonoscopies performed at LSU Health Shreveport over a 3-month period starting in December 2020. The colonoscopies were performed by 10 different attending physicians and 13 different fellows/residents. Procedural sedation was performed by an endoscopy nurse, and a physician. Procedures that were done under minimal anesthesia care, sedation was administered by a certified nurse anesthetist, that included Midazolam, Ketamine, Fentanyl and Propofol. The inclusion criteria for the study were patients presenting for a screening colonoscopy with no prior colonoscopy, etcc..in the last 10 years. Poor prep, incomplete colonoscopy for any reason were excluded from the study. After chart review, various variables were recorded. The data was then used to show the ADR with the different variables.
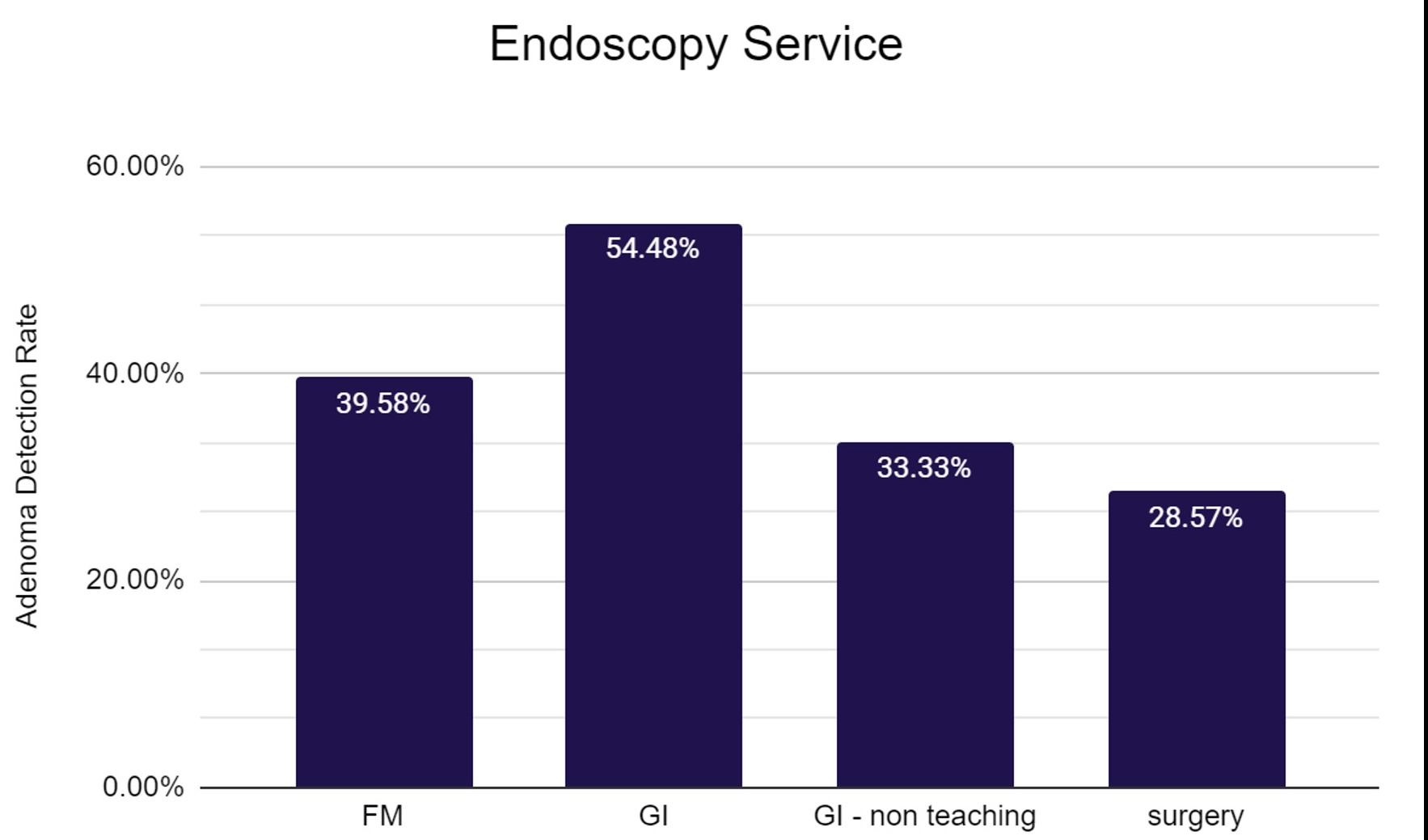
Results: 243 colonoscopies were reviewed. 144 with a gastroenterology fellow, 7 with a surgery resident, and 92 with an attending physician. The fellow's ADR were included vs with an attending alone was 54.3% vs 32.6% (p-value 0.0009). Of colonoscopies done, 59 had MAC sedation, 94 with an endoscopist giving propofol sedation, 89 with versed sedation resulting in ADR of 57.6% vs 53.2% vs 30.3%. When comparing ADR of MAC (57.6%) vs non-MAC (42.1%) was statistically significant with a p-value of 0.04. When comparing ADR to the attending service, endoscopist was part of: GI teaching service 54.5%, GI non-teaching 33.3%, Family medicine 39.6%, and surgery 28.6%.
Discussion: Many people understand the importance of screening colonoscopy and the aim of this study was to find out what variables improve the quality of colonoscopies. It showed that a colonoscopy that involves a fellow, attending teaching service, with MAC anesthesia has the highest rate of detection of precancerous adenomas. Limitations of the study include a low sample size. Other limitations include the different services have varying practice habits such as withdrawal time.
Disclosures:
Siva Santosh Kumar Gandu, MD1, Philip Bouchette, MD2, Jordan Roussel, MD2, Sudha Pandit, MD3. C0167 - Does Having a Fellow Improve the Quality of Screening Colonoscopy?, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1LSUHSC-, Shreveport, LA; 2Louisiana State University Health Sciences Center, Shreveport, LA; 3LSUHSC, Shreveport, LA
Introduction: Adenoma detection rate (ADR) is used as a quality metric for physicians performing screening colonoscopies. Many studies use the ADR to assess if different variables affect the quality of colonoscopy. At times, some patients request that a physician in training, a gastroenterology fellow, not be involved in their procedure. This study aims to assess the differences in ADR during screening colonoscopy with and without involvement of the gastroenterology fellow.
Methods: A retrospective review of 243 consecutive screening colonoscopies performed at LSU Health Shreveport over a 3-month period starting in December 2020. The colonoscopies were performed by 10 different attending physicians and 13 different fellows/residents. Procedural sedation was performed by an endoscopy nurse, and a physician. Procedures that were done under minimal anesthesia care, sedation was administered by a certified nurse anesthetist, that included Midazolam, Ketamine, Fentanyl and Propofol. The inclusion criteria for the study were patients presenting for a screening colonoscopy with no prior colonoscopy, etcc..in the last 10 years. Poor prep, incomplete colonoscopy for any reason were excluded from the study. After chart review, various variables were recorded. The data was then used to show the ADR with the different variables.
Results: 243 colonoscopies were reviewed. 144 with a gastroenterology fellow, 7 with a surgery resident, and 92 with an attending physician. The fellow's ADR were included vs with an attending alone was 54.3% vs 32.6% (p-value 0.0009). Of colonoscopies done, 59 had MAC sedation, 94 with an endoscopist giving propofol sedation, 89 with versed sedation resulting in ADR of 57.6% vs 53.2% vs 30.3%. When comparing ADR of MAC (57.6%) vs non-MAC (42.1%) was statistically significant with a p-value of 0.04. When comparing ADR to the attending service, endoscopist was part of: GI teaching service 54.5%, GI non-teaching 33.3%, Family medicine 39.6%, and surgery 28.6%.
Discussion: Many people understand the importance of screening colonoscopy and the aim of this study was to find out what variables improve the quality of colonoscopies. It showed that a colonoscopy that involves a fellow, attending teaching service, with MAC anesthesia has the highest rate of detection of precancerous adenomas. Limitations of the study include a low sample size. Other limitations include the different services have varying practice habits such as withdrawal time.
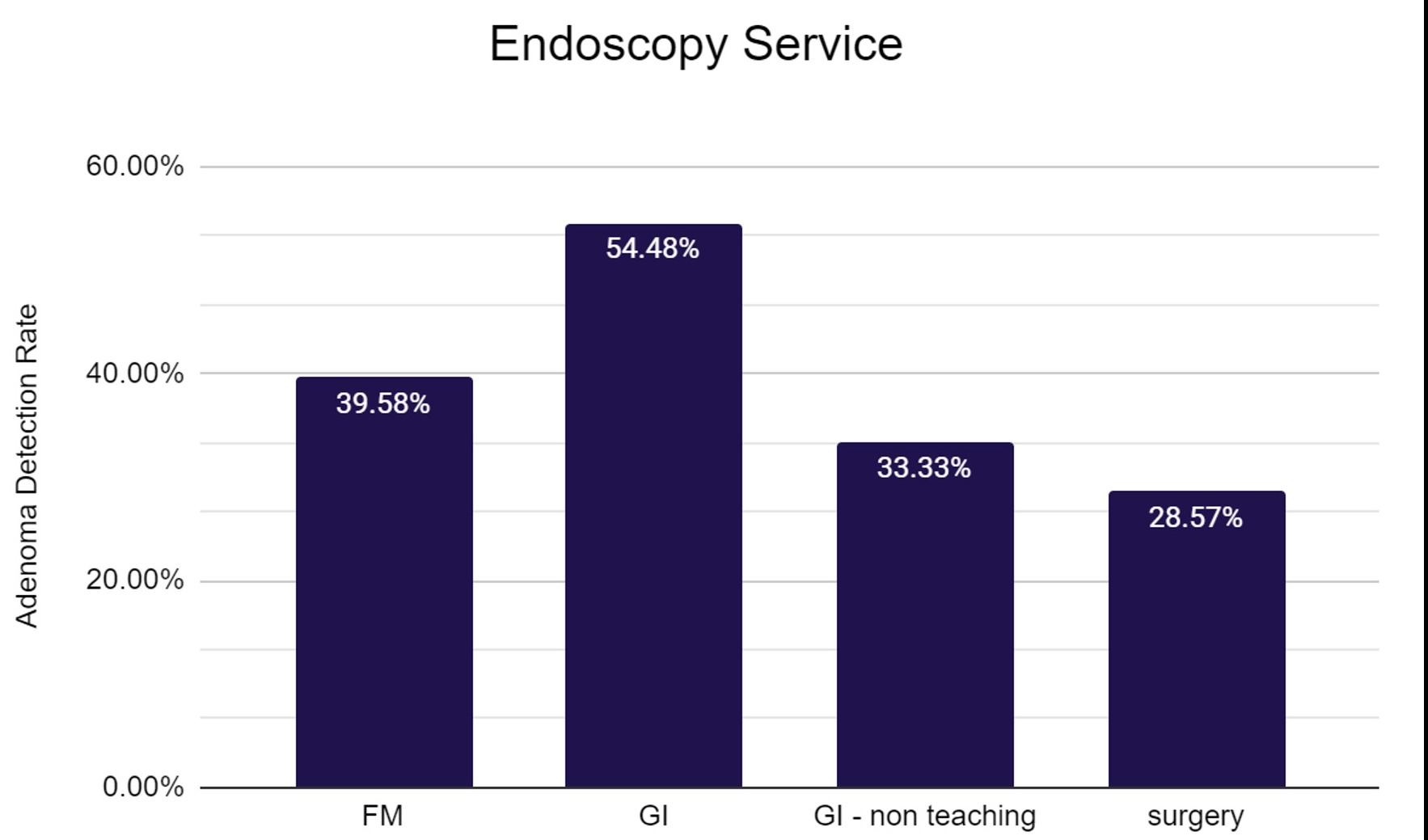
Figure: ADR by service
Disclosures:
Siva Santosh Kumar Gandu indicated no relevant financial relationships.
Philip Bouchette indicated no relevant financial relationships.
Jordan Roussel indicated no relevant financial relationships.
Sudha Pandit indicated no relevant financial relationships.
Siva Santosh Kumar Gandu, MD1, Philip Bouchette, MD2, Jordan Roussel, MD2, Sudha Pandit, MD3. C0167 - Does Having a Fellow Improve the Quality of Screening Colonoscopy?, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
