Back
Poster Session E - Tuesday Afternoon
E0152 - Cocaine-Induced Pseudomembranous Colitis With Negative Clostridium difficile Infection
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
- MC
Mit A. Chauhan, MD
Saint Michael's Medical Center
Newark, NJ
Presenting Author(s)
Mit A. Chauhan, MD1, Rewanth Katamreddy, MD1, Alicia Kovach, MD1, Saraswathi Lakkasani, MD2, Yatinder Bains, MD2, Amol Shah, MD1
1Saint Michael's Medical Center, Newark, NJ; 2Saint Michael's Medical Center, New York Medical College, Newark, NJ
Introduction: Pseudomembranous colitis (PMC) is most commonly caused by Clostridium difficle (C.Diff). The incidence of C.Diff related PMC is 3-8% and increasing. Other than C.Diff, ischemia, infections, medications, and inflammatory conditions can cause PMC. We report a case of pseudomembranous colitis-tested negative PCR for C.Diff
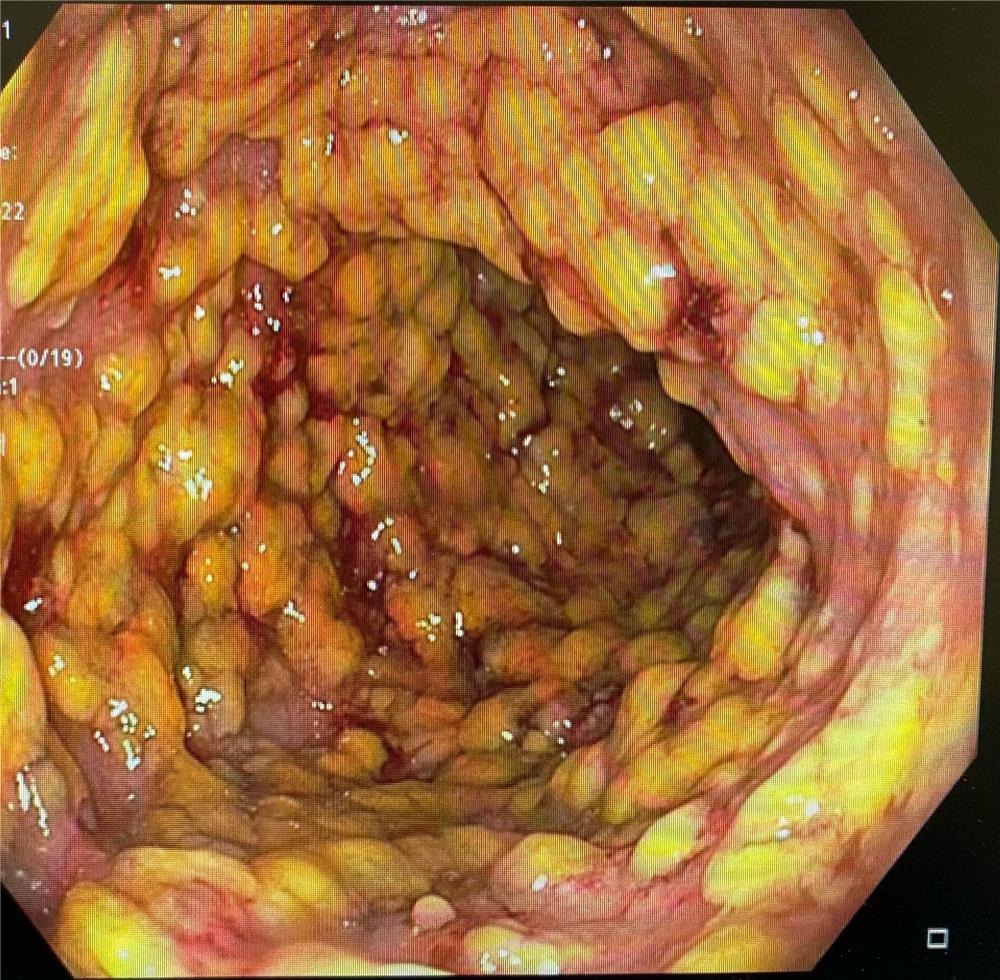
Case Description/Methods: A 52-year-old female with a past medical history of hypothyroidism, asthma, and polysubstance abuse (history of chronic heroin, cocaine, benzodiazepine, alcohol, and cigarette use) with Hx of chronic intermittent diarrhea due to Opioid withdrawal presented to the emergency department with bloody watery diarrhea of 3-4 times in a day for 5 days. On initial evaluation, the patient's vital signs are stable. The abdomen is diffusely tender on physical examination with increased tenderness in the left lower quadrant. Labs showed WBC count of 15,900/μL, 90.2% neutrophils, AST of 80 U/L, ALT of 41 U/L, ALP of 97 U/L, total bilirubin of 0.5 mg/dL, lactic acid of 0.9 mmol/L and c-reactive protein of 11.9 mg/dL. The urine drug screen was positive for benzodiazepine, cocaine, opiate, and methadone. CT scan of the abdomen showed mild diffuse concentric colonic wall thickening representing colitis. The patient was empirically treated with IV ceftriaxone, IV metronidazole, and PO vancomycin. Stool for C. difficile PCR was negative three times on three different days. Stool culture was negative for Salmonella, Shigella, Campylobacter, or E. coli O157:H7. Fecal lactoferrin quantification was 320.72 μg/mL. The patient underwent sigmoidoscopy, which showed discontinuous areas of ulcerated mucosa covered with yellowish punctate membrane with stigmata of recent bleeding in the entire examined colon. Biopsy of the colon showed focal active colitis with superficial crypt erosion and focal adherent mucopurulent material negative for crypt abscesses and granulomas, consistent with pseudomembranous colitis. The patient was continually treated with supportive care including IV fluids and bowel rest. Her diet was advanced, and her diarrhea improved.
Discussion: Other than C.Diff, we propose keeping other differentials of pseudomembranous colitis is essential. Other infections from S. aureus, E. coli, Shigella and Strongyloides may also cause PMC. Non-infectious causes of PMC include chemical endoscope cleaning agents, intestinal ischemia, drug abuse from cocaine, inflammatory bowel disease, and microscopic colitis to avoid over-usage of antibiotics and focus on targeted therapy.
Disclosures:
Mit A. Chauhan, MD1, Rewanth Katamreddy, MD1, Alicia Kovach, MD1, Saraswathi Lakkasani, MD2, Yatinder Bains, MD2, Amol Shah, MD1. E0152 - Cocaine-Induced Pseudomembranous Colitis With Negative Clostridium difficile Infection, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Saint Michael's Medical Center, Newark, NJ; 2Saint Michael's Medical Center, New York Medical College, Newark, NJ
Introduction: Pseudomembranous colitis (PMC) is most commonly caused by Clostridium difficle (C.Diff). The incidence of C.Diff related PMC is 3-8% and increasing. Other than C.Diff, ischemia, infections, medications, and inflammatory conditions can cause PMC. We report a case of pseudomembranous colitis-tested negative PCR for C.Diff
Case Description/Methods: A 52-year-old female with a past medical history of hypothyroidism, asthma, and polysubstance abuse (history of chronic heroin, cocaine, benzodiazepine, alcohol, and cigarette use) with Hx of chronic intermittent diarrhea due to Opioid withdrawal presented to the emergency department with bloody watery diarrhea of 3-4 times in a day for 5 days. On initial evaluation, the patient's vital signs are stable. The abdomen is diffusely tender on physical examination with increased tenderness in the left lower quadrant. Labs showed WBC count of 15,900/μL, 90.2% neutrophils, AST of 80 U/L, ALT of 41 U/L, ALP of 97 U/L, total bilirubin of 0.5 mg/dL, lactic acid of 0.9 mmol/L and c-reactive protein of 11.9 mg/dL. The urine drug screen was positive for benzodiazepine, cocaine, opiate, and methadone. CT scan of the abdomen showed mild diffuse concentric colonic wall thickening representing colitis. The patient was empirically treated with IV ceftriaxone, IV metronidazole, and PO vancomycin. Stool for C. difficile PCR was negative three times on three different days. Stool culture was negative for Salmonella, Shigella, Campylobacter, or E. coli O157:H7. Fecal lactoferrin quantification was 320.72 μg/mL. The patient underwent sigmoidoscopy, which showed discontinuous areas of ulcerated mucosa covered with yellowish punctate membrane with stigmata of recent bleeding in the entire examined colon. Biopsy of the colon showed focal active colitis with superficial crypt erosion and focal adherent mucopurulent material negative for crypt abscesses and granulomas, consistent with pseudomembranous colitis. The patient was continually treated with supportive care including IV fluids and bowel rest. Her diet was advanced, and her diarrhea improved.
Discussion: Other than C.Diff, we propose keeping other differentials of pseudomembranous colitis is essential. Other infections from S. aureus, E. coli, Shigella and Strongyloides may also cause PMC. Non-infectious causes of PMC include chemical endoscope cleaning agents, intestinal ischemia, drug abuse from cocaine, inflammatory bowel disease, and microscopic colitis to avoid over-usage of antibiotics and focus on targeted therapy.
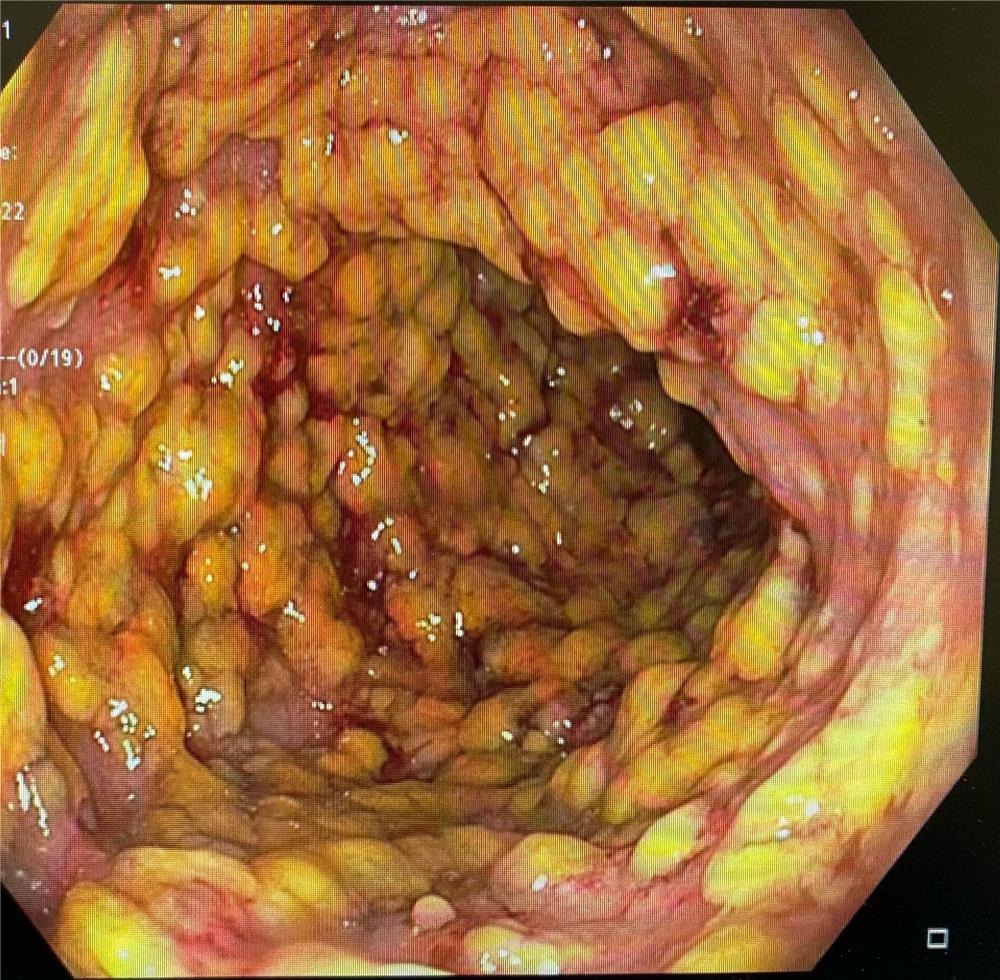
Figure: Image 1 shows discontinuous areas of ulcerated mucosa covered with yellowish punctate membrane with stigmata of recent bleeding in the entire examined colon
Disclosures:
Mit Chauhan indicated no relevant financial relationships.
Rewanth Katamreddy indicated no relevant financial relationships.
Alicia Kovach indicated no relevant financial relationships.
Saraswathi Lakkasani indicated no relevant financial relationships.
Yatinder Bains indicated no relevant financial relationships.
Amol Shah indicated no relevant financial relationships.
Mit A. Chauhan, MD1, Rewanth Katamreddy, MD1, Alicia Kovach, MD1, Saraswathi Lakkasani, MD2, Yatinder Bains, MD2, Amol Shah, MD1. E0152 - Cocaine-Induced Pseudomembranous Colitis With Negative Clostridium difficile Infection, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
