Back
Poster Session E - Tuesday Afternoon
E0129 - Colonic Ischemia: When a Rare Etiology Leads to an Unusual Presentation
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Mahmoud Bayoumi, MD, MPH
University of Arizona College of Medicine
Phoenix, AZ
Presenting Author(s)
Mahmoud Bayoumi, MD, MPH1, Nael Haddad, MD1, Wendy Z. Lamb, MD2, Sakolwan Suchartlikitwong, MD1, Hugo Pinillos, MD, FACG1
1University of Arizona College of Medicine, Phoenix, AZ; 2University of Arizona College of Medicine, Litchfield Park, AZ
Introduction: Colon ischemia is the most common form of intestinal ischemia. It is acute and transient but can be chronic if the leading cause is not recognized and reversed. We present a challenging case of chronic ischemic colitis for which conventional therapy was ineffective.
Case Description/Methods: A 54-year-old male with a past medical history of chronic kidney disease and anabolic steroid use presented to the GI lab for open access colonoscopy due to progressive severe rectal pain for two months associated with intermittent rectal bleeding.
His vital signs and physical exam were normal.
One day prior to presentation, he had unremarkable CBC, CMP, INR, CRP, ESR, amylase, and lipase.
CT A/P with contrast showed wall thickening and edema involving rectosigmoid region with surrounding stranding suggestive of colitis and proctitis. Splenic enlargement (16.3 cm) and splenic varices without obvious evidence of liver cirrhosis were noted.
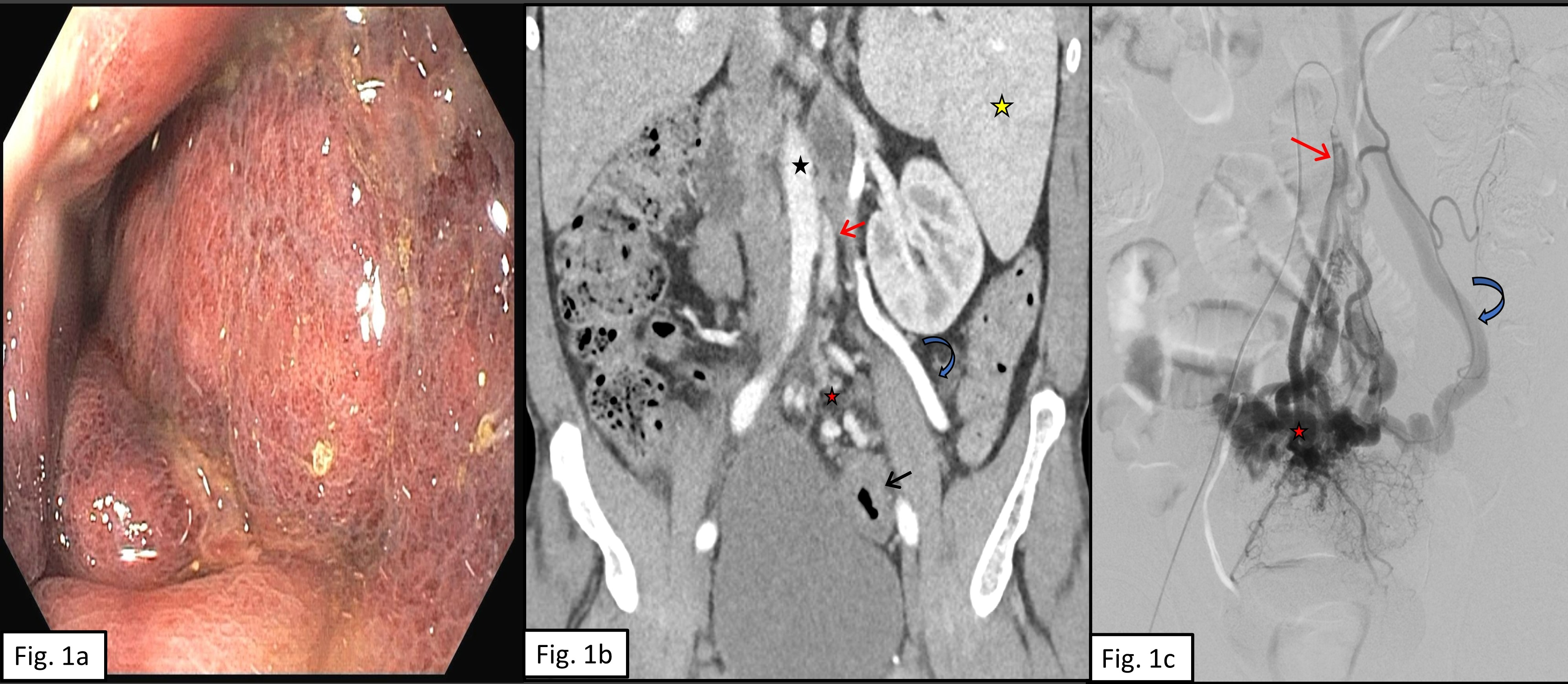
Colonoscopy showed severely inflamed and dark rectosigmoid mucosa with induration and friability (figure 1a), with a normal-appearing mucosa above 30 cm from the anus. Biopsies were obtained.
Stool culture, ova, parasites, c. difficile, calprotectin, and WBCs were negative. STI testing was negative.
Biopsies revealed changes suggestive of ischemia.
Hospital admission was needed for pain control. Colorectal surgery was consulted, and a repeat flexible sigmoidoscopy revealed unchanged mucosal abnormalities. Extensive coagulopathy workup was nonrevealing.
Despite completing a week of intravenous antibiotics, and multiple sessions of hyperbaric oxygenation therapy, he remained symptomatic and was discharged with pain management.
A repeat CTA A/P revealed worsening circumferential wall thickening of the rectosigmoid colon compatible with ischemia, prominent pelvic varices, and enlarged inferior mesenteric vein (IMV), which were thought to be related to arteriovenous (AV) shunt (figure 1b).
IR performed visceral angiography that showed AV malformation of the inferior mesenteric artery to the IMV (figure 1c).
Both embolization and surgical intervention were offered; however, he opted for conservative management.
Several months after presentation, he has maintained bowel function and continues to be on long-term opioid therapy for pain control.
Discussion: AVM is a rare cause of ischemic colitis, and presentation tends to be insidious. This case highlights the importance of obtaining vascular imaging in atypical cases of colonic ischemia as management would differ significantly.
Disclosures:
Mahmoud Bayoumi, MD, MPH1, Nael Haddad, MD1, Wendy Z. Lamb, MD2, Sakolwan Suchartlikitwong, MD1, Hugo Pinillos, MD, FACG1. E0129 - Colonic Ischemia: When a Rare Etiology Leads to an Unusual Presentation, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Arizona College of Medicine, Phoenix, AZ; 2University of Arizona College of Medicine, Litchfield Park, AZ
Introduction: Colon ischemia is the most common form of intestinal ischemia. It is acute and transient but can be chronic if the leading cause is not recognized and reversed. We present a challenging case of chronic ischemic colitis for which conventional therapy was ineffective.
Case Description/Methods: A 54-year-old male with a past medical history of chronic kidney disease and anabolic steroid use presented to the GI lab for open access colonoscopy due to progressive severe rectal pain for two months associated with intermittent rectal bleeding.
His vital signs and physical exam were normal.
One day prior to presentation, he had unremarkable CBC, CMP, INR, CRP, ESR, amylase, and lipase.
CT A/P with contrast showed wall thickening and edema involving rectosigmoid region with surrounding stranding suggestive of colitis and proctitis. Splenic enlargement (16.3 cm) and splenic varices without obvious evidence of liver cirrhosis were noted.
Colonoscopy showed severely inflamed and dark rectosigmoid mucosa with induration and friability (figure 1a), with a normal-appearing mucosa above 30 cm from the anus. Biopsies were obtained.
Stool culture, ova, parasites, c. difficile, calprotectin, and WBCs were negative. STI testing was negative.
Biopsies revealed changes suggestive of ischemia.
Hospital admission was needed for pain control. Colorectal surgery was consulted, and a repeat flexible sigmoidoscopy revealed unchanged mucosal abnormalities. Extensive coagulopathy workup was nonrevealing.
Despite completing a week of intravenous antibiotics, and multiple sessions of hyperbaric oxygenation therapy, he remained symptomatic and was discharged with pain management.
A repeat CTA A/P revealed worsening circumferential wall thickening of the rectosigmoid colon compatible with ischemia, prominent pelvic varices, and enlarged inferior mesenteric vein (IMV), which were thought to be related to arteriovenous (AV) shunt (figure 1b).
IR performed visceral angiography that showed AV malformation of the inferior mesenteric artery to the IMV (figure 1c).
Both embolization and surgical intervention were offered; however, he opted for conservative management.
Several months after presentation, he has maintained bowel function and continues to be on long-term opioid therapy for pain control.
Discussion: AVM is a rare cause of ischemic colitis, and presentation tends to be insidious. This case highlights the importance of obtaining vascular imaging in atypical cases of colonic ischemia as management would differ significantly.
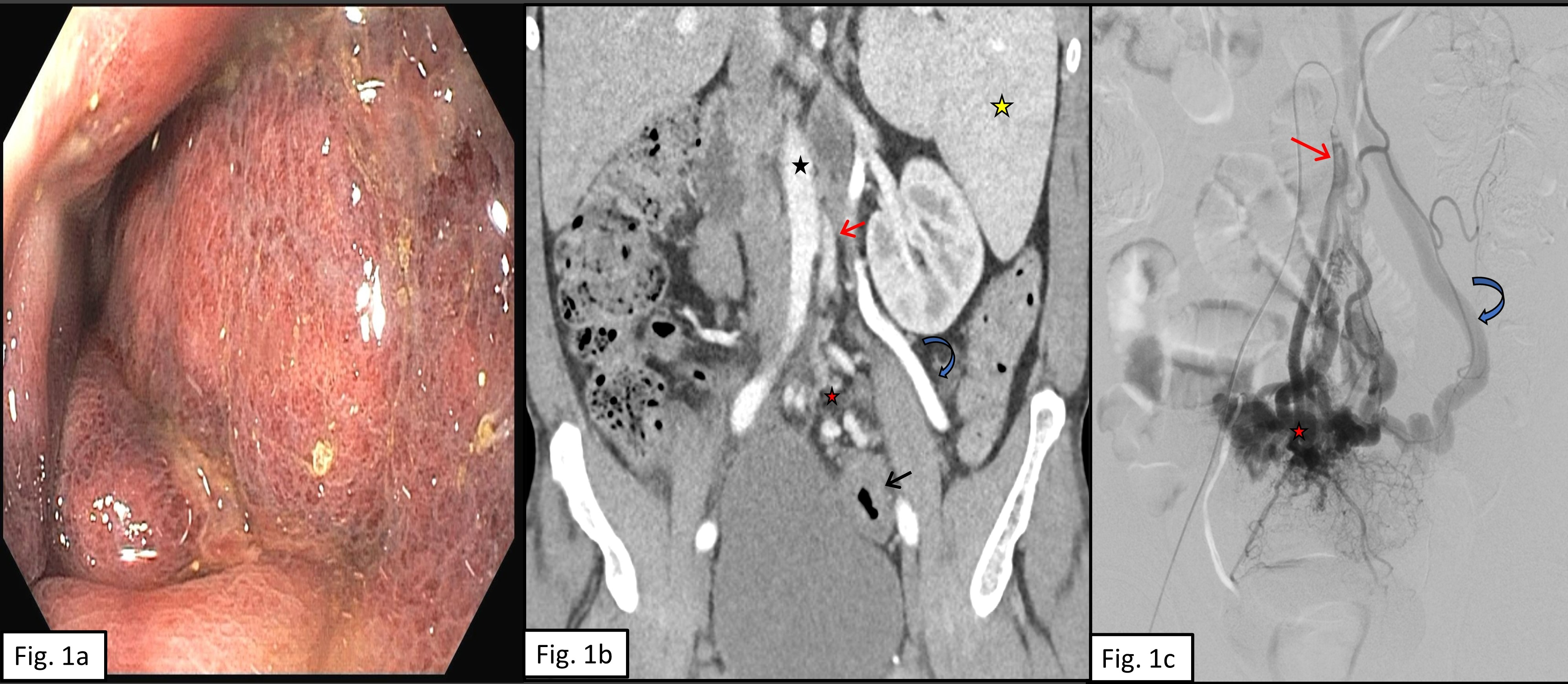
Figure: Figure 1a. A colonoscopy showing severely inflamed and dark rectosigmoid mucosa with induration and friability. Figure 1b. A coronal CT abdomen/pelvis, arterial phase, depicts an increased number of enlarged vessels (red star) superior to a thick-walled rectum (black arrow). These vessels represent the hypertrophied inferior mesenteric artery (red arrow) and its rectal branches. Early filling of an enlarged inferior mesenteric vein (blue curved arrow). Note: enlarged spleen (yellow star) likely related to the high flow state caused by the rectal vascular malformation (AVM), as portal pressures are normal. Aorta (black star). Figure 1c. Selective inferior mesenteric artery (IMA) digital subtraction angiography (DSA), frontal coned down view of the pelvis. The IMA (red arrow) is the main feeder artery to the rectal AVM nidus (red star), which is a complex tangle of enlarged vessels at the rectum. Early filling of an enlarged inferior mesenteric vein (IMV) (blue curved arrow) noted on this conventional angiogram indicating that IMV is the main draining vein.
Disclosures:
Mahmoud Bayoumi indicated no relevant financial relationships.
Nael Haddad indicated no relevant financial relationships.
Wendy Lamb indicated no relevant financial relationships.
Sakolwan Suchartlikitwong indicated no relevant financial relationships.
Hugo Pinillos indicated no relevant financial relationships.
Mahmoud Bayoumi, MD, MPH1, Nael Haddad, MD1, Wendy Z. Lamb, MD2, Sakolwan Suchartlikitwong, MD1, Hugo Pinillos, MD, FACG1. E0129 - Colonic Ischemia: When a Rare Etiology Leads to an Unusual Presentation, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
