Back
Poster Session C - Monday Afternoon
C0065 - Management of Young Patients With Recurrent Episodes of Acute Pancreatitis
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
- ET
Elena Toader, MD, PhD
University of Medicine and Pharmacy "Grigore T. Popa", Iasi, Romania; Institute of Gastroenterology and Hepatology, “St. Spiridon” Emergency County Hospital
Iasi, Iasi, Romania
Presenting Author(s)
Elena Toader, MD, PhD1, Madalina-Anca Musteata, MD2, Mirela Piscuc, MD2, Andreea-Luiza Palamaru, MD3, Andreea Decusara, MD1
1University of Medicine and Pharmacy "Grigore T. Popa", Iasi, Romania; Institute of Gastroenterology and Hepatology, “St. Spiridon” Emergency County Hospital, Iasi, Iasi, Romania; 2Institute of Gastroenterology and Hepatology, “St. Spiridon” Emergency County Hospital, Iasi, Iasi, Romania; 3University of Medicine and Pharmacy "Grigore T. Popa", Iasi, Iasi, Romania
Introduction: Hereditary pancreatitis (HP) is a rare genetic condition, the evolution of which is marked by recurrent episodes of acute pancreatitis that begin in childhood or adolescence and lead to the early inception of chronic pancreatitis and a significant increase in the risk of pancreatic cancer in young adults.
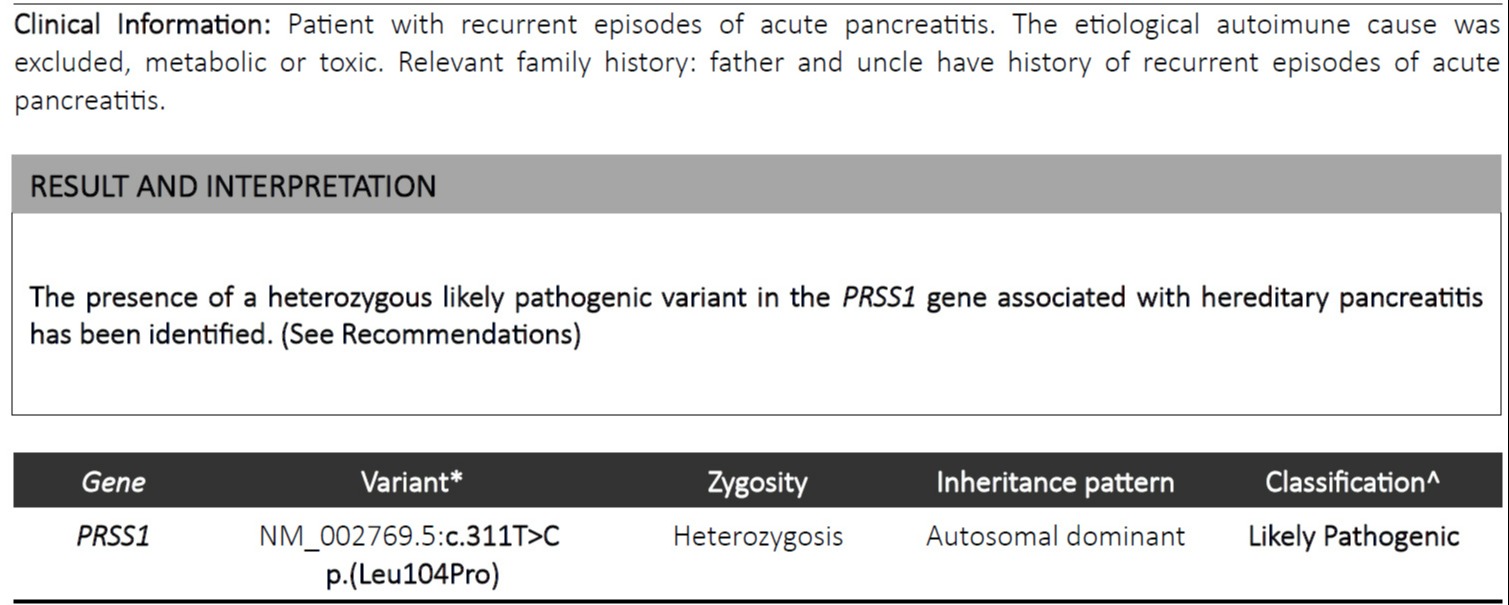
Case Description/Methods: We present the case of a 22-year-old patient, with repeated appearances in the gastroenterology department for episodes of acute pancreatitis (11 episodes), started at the age of 15, for which recent computed tomography scan (2022) showed changes suggestive for chronic pancreatitis. Anamnestic and laboratory tests have ruled out alcohol use, medications, dysmetabolic syndrome, as the most common causative factors involved in triggering episodes of acute pancreatitis. The echo-endoscopic investigation with biopsy was negative for specific markers of autoimmune pancreatitis. Given the positive history of acute pancreatitis (multiple episodes) of relatives (father and uncle), the presence of inherited genetic mutations was taken into account. The result of the genetic panel revealed the presence of a pathogenic variant probably heterozygous in the PRSS1 gene associated with hereditary pancreatitis (Figure 1). The case was included in an individualized management program with multidisciplinary involvement, with a focus on pain management, medical therapy for endocrine and exocrine insufficiency, and surveillance of the sequelae of chronic pancreatitis and pancreatic adenocarcinoma.
Discussion: The recurrence of acute pancreatitis episodes at a young age, with negative results for the causes frequently involved in the onset of acute episodes (toxic, metabolic, autoimmune), but with a positive family history of acute pancreatitis, justifies the extension of genetic testing investigations to establish an early diagnosis on hereditary pancreatitis. Given that there are no clearly established methods for preventing the development or progression of the disease in the context of the presence of a genetic mutation associated with HP, the emphasis in case management will focus on avoiding the triggers that can exacerbate and aggravate pancreatitis and monitoring the progression toward adenocarcinoma pancreatic.
Disclosures:
Elena Toader, MD, PhD1, Madalina-Anca Musteata, MD2, Mirela Piscuc, MD2, Andreea-Luiza Palamaru, MD3, Andreea Decusara, MD1. C0065 - Management of Young Patients With Recurrent Episodes of Acute Pancreatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Medicine and Pharmacy "Grigore T. Popa", Iasi, Romania; Institute of Gastroenterology and Hepatology, “St. Spiridon” Emergency County Hospital, Iasi, Iasi, Romania; 2Institute of Gastroenterology and Hepatology, “St. Spiridon” Emergency County Hospital, Iasi, Iasi, Romania; 3University of Medicine and Pharmacy "Grigore T. Popa", Iasi, Iasi, Romania
Introduction: Hereditary pancreatitis (HP) is a rare genetic condition, the evolution of which is marked by recurrent episodes of acute pancreatitis that begin in childhood or adolescence and lead to the early inception of chronic pancreatitis and a significant increase in the risk of pancreatic cancer in young adults.
Case Description/Methods: We present the case of a 22-year-old patient, with repeated appearances in the gastroenterology department for episodes of acute pancreatitis (11 episodes), started at the age of 15, for which recent computed tomography scan (2022) showed changes suggestive for chronic pancreatitis. Anamnestic and laboratory tests have ruled out alcohol use, medications, dysmetabolic syndrome, as the most common causative factors involved in triggering episodes of acute pancreatitis. The echo-endoscopic investigation with biopsy was negative for specific markers of autoimmune pancreatitis. Given the positive history of acute pancreatitis (multiple episodes) of relatives (father and uncle), the presence of inherited genetic mutations was taken into account. The result of the genetic panel revealed the presence of a pathogenic variant probably heterozygous in the PRSS1 gene associated with hereditary pancreatitis (Figure 1). The case was included in an individualized management program with multidisciplinary involvement, with a focus on pain management, medical therapy for endocrine and exocrine insufficiency, and surveillance of the sequelae of chronic pancreatitis and pancreatic adenocarcinoma.
Discussion: The recurrence of acute pancreatitis episodes at a young age, with negative results for the causes frequently involved in the onset of acute episodes (toxic, metabolic, autoimmune), but with a positive family history of acute pancreatitis, justifies the extension of genetic testing investigations to establish an early diagnosis on hereditary pancreatitis. Given that there are no clearly established methods for preventing the development or progression of the disease in the context of the presence of a genetic mutation associated with HP, the emphasis in case management will focus on avoiding the triggers that can exacerbate and aggravate pancreatitis and monitoring the progression toward adenocarcinoma pancreatic.
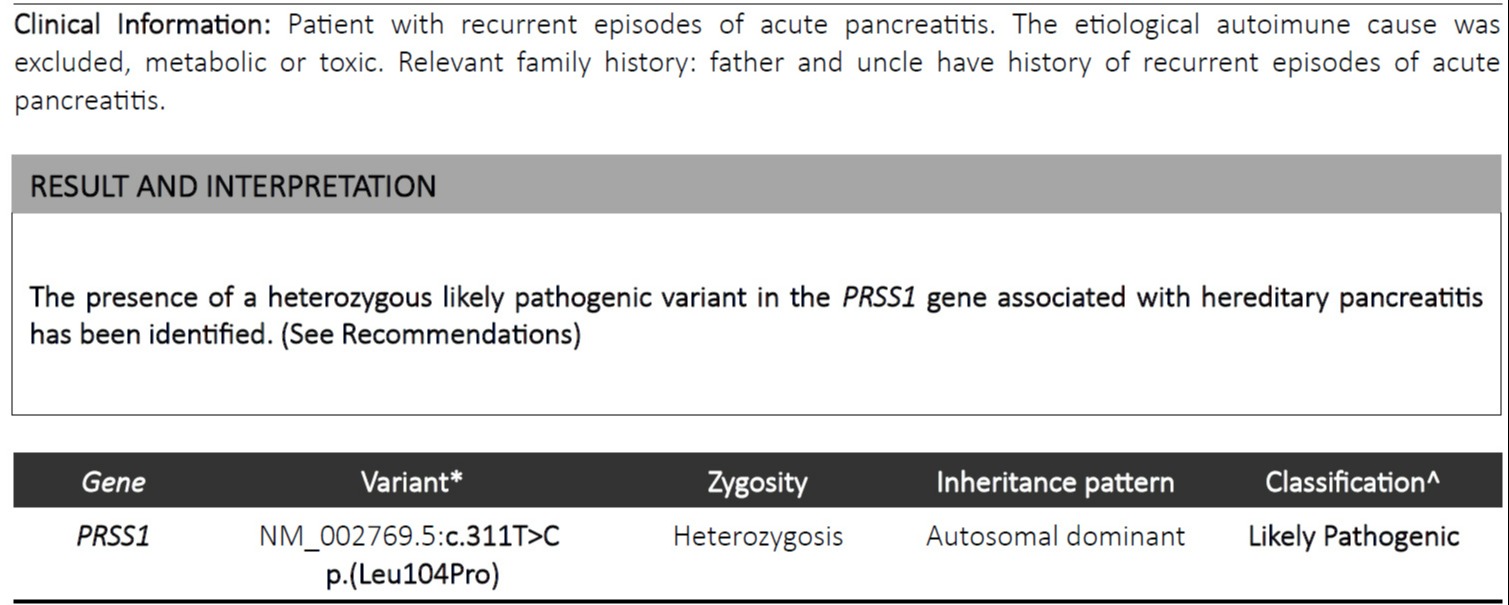
Figure: Figure 1. The result of the genetic panel
Disclosures:
Elena Toader indicated no relevant financial relationships.
Madalina-Anca Musteata indicated no relevant financial relationships.
Mirela Piscuc indicated no relevant financial relationships.
Andreea-Luiza Palamaru indicated no relevant financial relationships.
Andreea Decusara indicated no relevant financial relationships.
Elena Toader, MD, PhD1, Madalina-Anca Musteata, MD2, Mirela Piscuc, MD2, Andreea-Luiza Palamaru, MD3, Andreea Decusara, MD1. C0065 - Management of Young Patients With Recurrent Episodes of Acute Pancreatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
