Back
Poster Session C - Monday Afternoon
C0029 - Neurofibromatosis-Related Biliary Obstruction: Is There a Role in Screening for Biliary Malignancy?
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Danielle Joiner, MD
University of Kentucky
Lexington, KY
Presenting Author(s)
Danielle Joiner, MD1, Patrick J. Carey, MD2, Hammad Qureshi, MD1, Samuel Mardini, MD, MBA, MPH, FACG1, Naba Saeed, MD3
1University of Kentucky, Lexington, KY; 2University of Kentucky College of Medcine, Lexington, KY; 3The University of Kentucky, Lexington, KY
Introduction: Neurofibromatosis-1 (NF1) has known associations with numerous malignancies including breast, bone, thyroid, liver, lung, colon, ovary, esophagus, non-Hodgkins lymphoma, rhabdomyosarcoma, leukemia, and CNS tumors. Other than early initiation of breast cancer screening, there are no other specific cancer screening guidelines for these patients compared to the general population, despite the known high-prevalence of concomitant tumors in these patients. Up to 25% of NF1 patients can have GI tract involvement, but only 5% are symptomatic. Biliary involvement has been seen from periampullary neuroendocrine tumors and gastrointestinal stromal tumors. Biliary obstruction and biliary strictures from ganglioneuromas are rare.
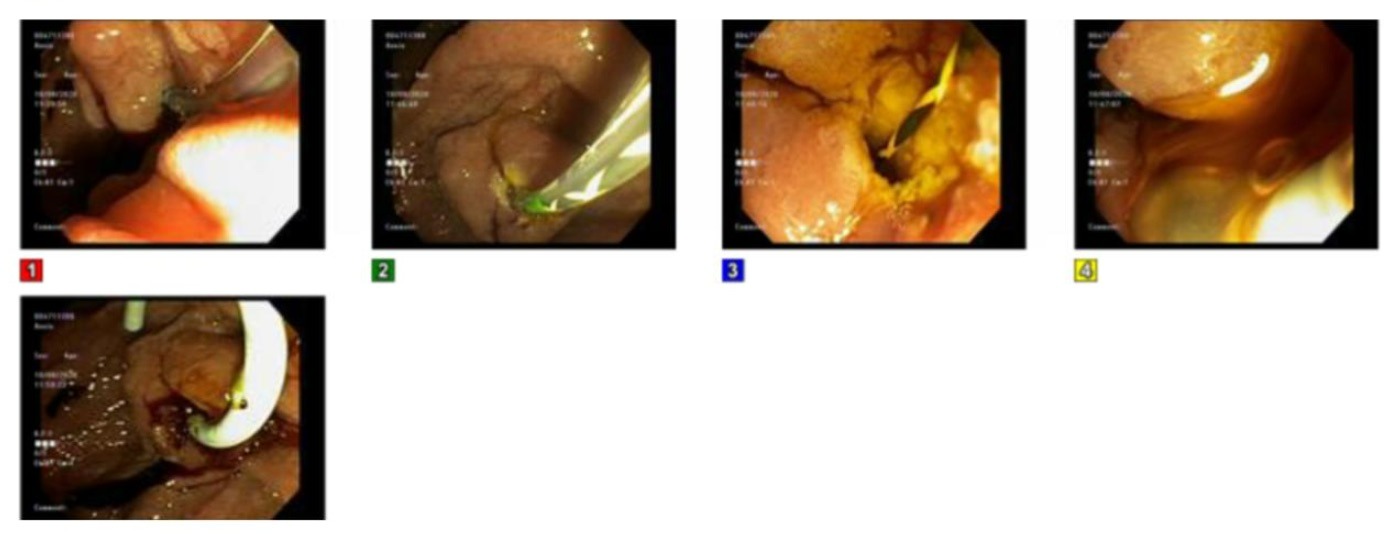
Case Description/Methods: A 63-year-old female with NF-1 who presented with a 5-month history of abdominal pain, nausea, and 40-lb weight loss was found to have ileocecal thickening and intra/extrahepatic biliary dilation on imaging. CEA & CA19-9 were normal. EGD showed multiple large polyps in the second portion of the duodenum. ERCP, as shown in Figure 1, was notable for a periampullary mass causing biliary obstruction and a mid-CBD stricture that was biopsied and stented across. Pathology revealed ganglioneuroma, and was negative for malignancy. After ileocecal thickening was found to be colon adenocarcinoma, she underwent right hemicolectomy and chemotherapy. Subsequently, she has had recurrent episodes of cholangitis related to periampullary obstruction and numerous biliary stents. EGD/ERCP at 1 year showed villous appearance of the ampulla with surrounding congestion. An irregular biliary stricture was again appreciated with pathology showing ganglioneuroma.
Discussion: NF-1 patients with periampullary or biliary tract masses have the potential for malignant transformation. There are no screening guidelines to facilitate early detection of tumor progression in this population. Patients with neurofibromatosis-like findings should also be considered to have other potential underlying genetic mutations, including constitutional mismatch-repair deficiency, which increases the risk of malignant transformation ~80%. Our patient had numerous ERCPs over one year. Although last ERCP had a villous appearance of her periampullary mass, biopsy remained negative for malignancy. She will undergo repeat sampling and stent removal in a few months, where biopsy will be repeated. We suggest the need for biliary imaging/sampling to screen for malignant transformation in similar patients.
Disclosures:
Danielle Joiner, MD1, Patrick J. Carey, MD2, Hammad Qureshi, MD1, Samuel Mardini, MD, MBA, MPH, FACG1, Naba Saeed, MD3. C0029 - Neurofibromatosis-Related Biliary Obstruction: Is There a Role in Screening for Biliary Malignancy?, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Kentucky, Lexington, KY; 2University of Kentucky College of Medcine, Lexington, KY; 3The University of Kentucky, Lexington, KY
Introduction: Neurofibromatosis-1 (NF1) has known associations with numerous malignancies including breast, bone, thyroid, liver, lung, colon, ovary, esophagus, non-Hodgkins lymphoma, rhabdomyosarcoma, leukemia, and CNS tumors. Other than early initiation of breast cancer screening, there are no other specific cancer screening guidelines for these patients compared to the general population, despite the known high-prevalence of concomitant tumors in these patients. Up to 25% of NF1 patients can have GI tract involvement, but only 5% are symptomatic. Biliary involvement has been seen from periampullary neuroendocrine tumors and gastrointestinal stromal tumors. Biliary obstruction and biliary strictures from ganglioneuromas are rare.
Case Description/Methods: A 63-year-old female with NF-1 who presented with a 5-month history of abdominal pain, nausea, and 40-lb weight loss was found to have ileocecal thickening and intra/extrahepatic biliary dilation on imaging. CEA & CA19-9 were normal. EGD showed multiple large polyps in the second portion of the duodenum. ERCP, as shown in Figure 1, was notable for a periampullary mass causing biliary obstruction and a mid-CBD stricture that was biopsied and stented across. Pathology revealed ganglioneuroma, and was negative for malignancy. After ileocecal thickening was found to be colon adenocarcinoma, she underwent right hemicolectomy and chemotherapy. Subsequently, she has had recurrent episodes of cholangitis related to periampullary obstruction and numerous biliary stents. EGD/ERCP at 1 year showed villous appearance of the ampulla with surrounding congestion. An irregular biliary stricture was again appreciated with pathology showing ganglioneuroma.
Discussion: NF-1 patients with periampullary or biliary tract masses have the potential for malignant transformation. There are no screening guidelines to facilitate early detection of tumor progression in this population. Patients with neurofibromatosis-like findings should also be considered to have other potential underlying genetic mutations, including constitutional mismatch-repair deficiency, which increases the risk of malignant transformation ~80%. Our patient had numerous ERCPs over one year. Although last ERCP had a villous appearance of her periampullary mass, biopsy remained negative for malignancy. She will undergo repeat sampling and stent removal in a few months, where biopsy will be repeated. We suggest the need for biliary imaging/sampling to screen for malignant transformation in similar patients.
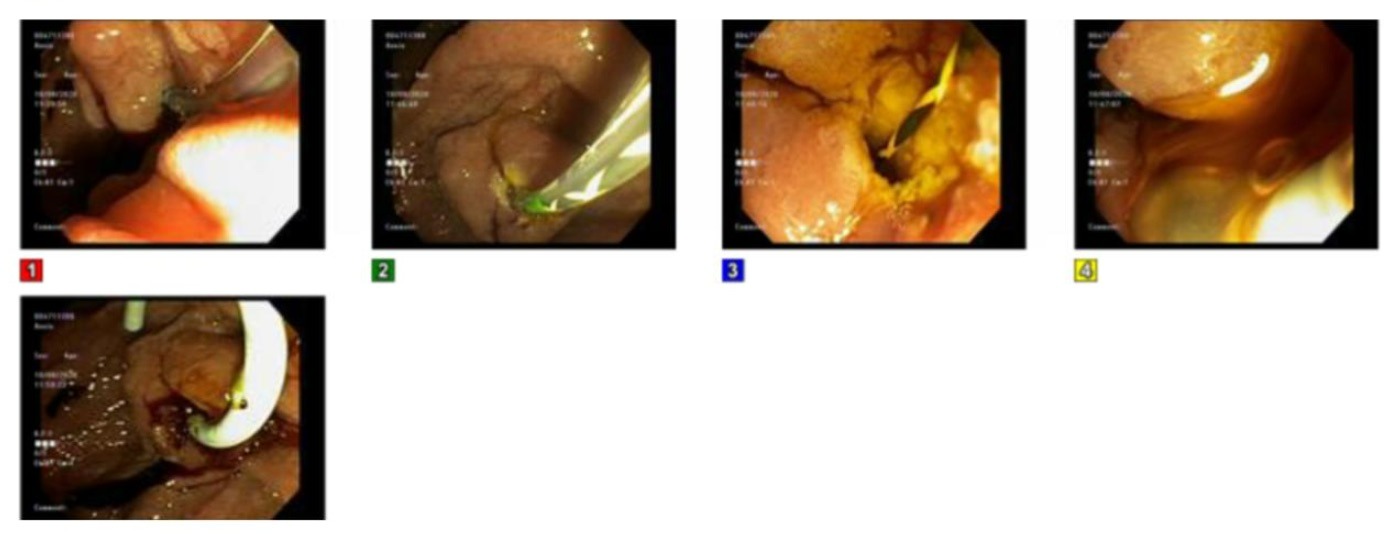
Figure: Figure 1: ERCP images demonstrating periampullary mass, and CBD stricture
Disclosures:
Danielle Joiner indicated no relevant financial relationships.
Patrick Carey indicated no relevant financial relationships.
Hammad Qureshi indicated no relevant financial relationships.
Samuel Mardini indicated no relevant financial relationships.
Naba Saeed indicated no relevant financial relationships.
Danielle Joiner, MD1, Patrick J. Carey, MD2, Hammad Qureshi, MD1, Samuel Mardini, MD, MBA, MPH, FACG1, Naba Saeed, MD3. C0029 - Neurofibromatosis-Related Biliary Obstruction: Is There a Role in Screening for Biliary Malignancy?, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
