Back
Poster Session C - Monday Afternoon
C0002 - Overutilization of Amylase and Lipase Testing in Acute Pancreatitis
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Vatsal Khanna, MD
Wayne State University School of Medicine
Rochester Hills, MI
Presenting Author(s)
Vatsal Khanna, MD1, Alaa Taha, MD1, Ranim Chamseddin, MD2, Yashar Eshman, MD1, Vesna Tegeltija, MD1
1Wayne State University School of Medicine, Rochester Hills, MI; 2Wayne State University, Rochester, MI
Introduction: Acute pancreatitis (AP) is a common cause of hospitalization and is a substantial financial burden to the healthcare system. The American College of Gastroenterology (ACG) guidelines recommend using serum lipase over amylase to diagnose AP, as it has superior specificity and sensitivity. However, based on our institution’s observation, patients diagnosed with AP had both amylase and lipase ordered and had follow-up measurements after diagnosis. We aim to decrease co-testing of amylase and lipase during pancreatitis workup by 40% in 6 months at our community hospital.
Methods: The Institute of Healthcare Improvement model was used for this quality improvement project. A multidisciplinary team approach was utilized. The Plan, Do, Study, Act (PDSA) cycle was used to format this project and test change. Root cause analysis was done using the fishbone diagram.
Results: Pre-intervention, 98% of admissions for AP had serum amylase and lipase ordered at the time of diagnosis, and 82% of patients had repeat testing. In PDSA cycle 1, there was no significant decrease in ordering both amylase and lipase during initial diagnosis, but the intervention decreased repeat testing to 73%.
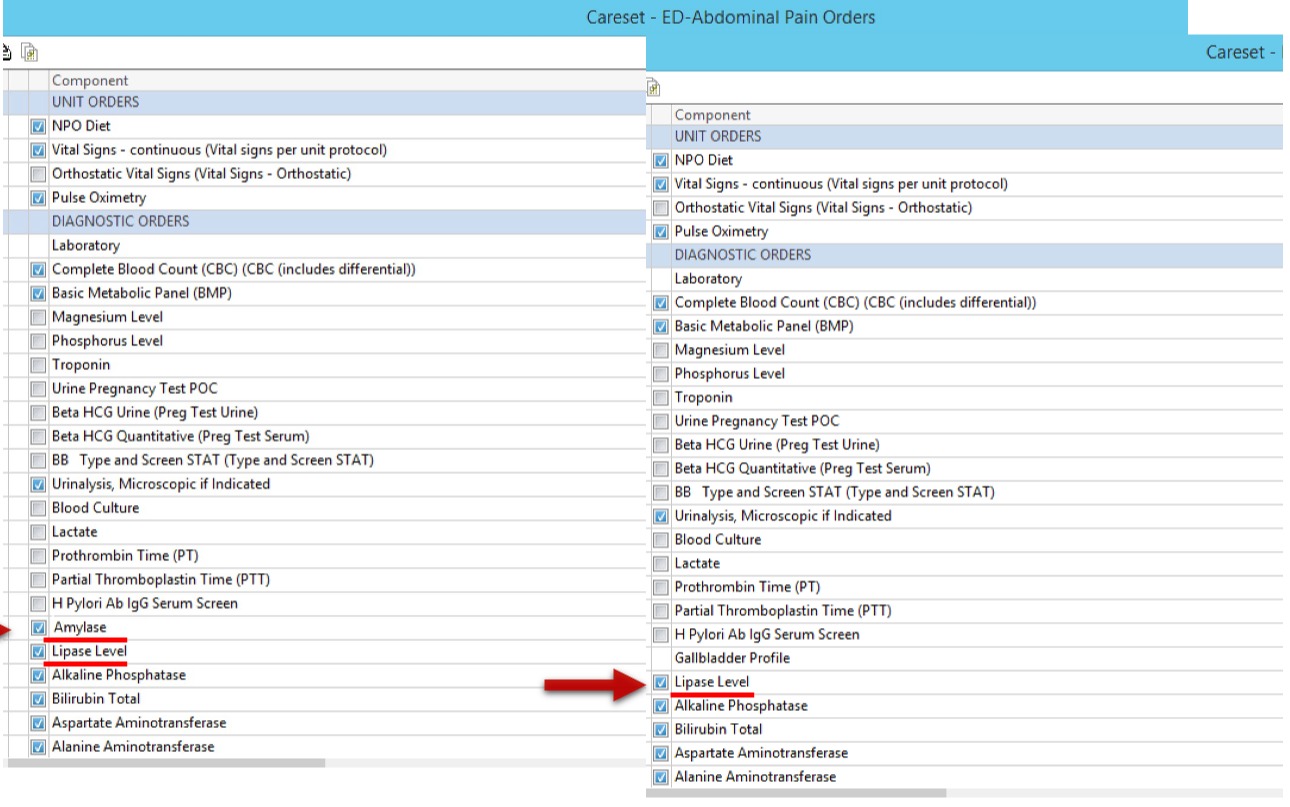
PDSA 2 involved educating residents and the emergency department ( ED ) about the guidelines. After two cycles failed to result in change, a root cause analysis was done and showed an EMR system order set for abdominal pain with pre-selected amylase and lipase. All patients with abdominal pain had both the tests ordered unless the ordering provider de-selects.
In PDSA 3, we used a multidisciplinary approach and worked to remove the pre-selected amylase from the order set. Post EMR change, we reviewed 98 patients over a six-month period who had abdominal pain and acute pancreatitis workup. Results showed a 48% reduction in amylase orders.
Discussion: PDSA 3 cycle involved removing the pre-selected amylase from the ED order set. The average cost of amylase testing is $35. Post-intervention, six-month data revealed a 48% reduction in amylase co-ordering. This result showed a $1645 direct cost saving. At this pace, yearly cost savings of $3290 would be observed.
Performing a root cause analysis allows discovering key stakeholder and system components contributing to outcomes. We used a process flow map to identify a system problem, including pre-selecting unnecessary labs during patient admission. Targeting a system change and de-selecting amylase from the order set allowed us to reduce unnecessary testing and hospital costs.
Disclosures:
Vatsal Khanna, MD1, Alaa Taha, MD1, Ranim Chamseddin, MD2, Yashar Eshman, MD1, Vesna Tegeltija, MD1. C0002 - Overutilization of Amylase and Lipase Testing in Acute Pancreatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Wayne State University School of Medicine, Rochester Hills, MI; 2Wayne State University, Rochester, MI
Introduction: Acute pancreatitis (AP) is a common cause of hospitalization and is a substantial financial burden to the healthcare system. The American College of Gastroenterology (ACG) guidelines recommend using serum lipase over amylase to diagnose AP, as it has superior specificity and sensitivity. However, based on our institution’s observation, patients diagnosed with AP had both amylase and lipase ordered and had follow-up measurements after diagnosis. We aim to decrease co-testing of amylase and lipase during pancreatitis workup by 40% in 6 months at our community hospital.
Methods: The Institute of Healthcare Improvement model was used for this quality improvement project. A multidisciplinary team approach was utilized. The Plan, Do, Study, Act (PDSA) cycle was used to format this project and test change. Root cause analysis was done using the fishbone diagram.
Results: Pre-intervention, 98% of admissions for AP had serum amylase and lipase ordered at the time of diagnosis, and 82% of patients had repeat testing. In PDSA cycle 1, there was no significant decrease in ordering both amylase and lipase during initial diagnosis, but the intervention decreased repeat testing to 73%.
PDSA 2 involved educating residents and the emergency department ( ED ) about the guidelines. After two cycles failed to result in change, a root cause analysis was done and showed an EMR system order set for abdominal pain with pre-selected amylase and lipase. All patients with abdominal pain had both the tests ordered unless the ordering provider de-selects.
In PDSA 3, we used a multidisciplinary approach and worked to remove the pre-selected amylase from the order set. Post EMR change, we reviewed 98 patients over a six-month period who had abdominal pain and acute pancreatitis workup. Results showed a 48% reduction in amylase orders.
Discussion: PDSA 3 cycle involved removing the pre-selected amylase from the ED order set. The average cost of amylase testing is $35. Post-intervention, six-month data revealed a 48% reduction in amylase co-ordering. This result showed a $1645 direct cost saving. At this pace, yearly cost savings of $3290 would be observed.
Performing a root cause analysis allows discovering key stakeholder and system components contributing to outcomes. We used a process flow map to identify a system problem, including pre-selecting unnecessary labs during patient admission. Targeting a system change and de-selecting amylase from the order set allowed us to reduce unnecessary testing and hospital costs.
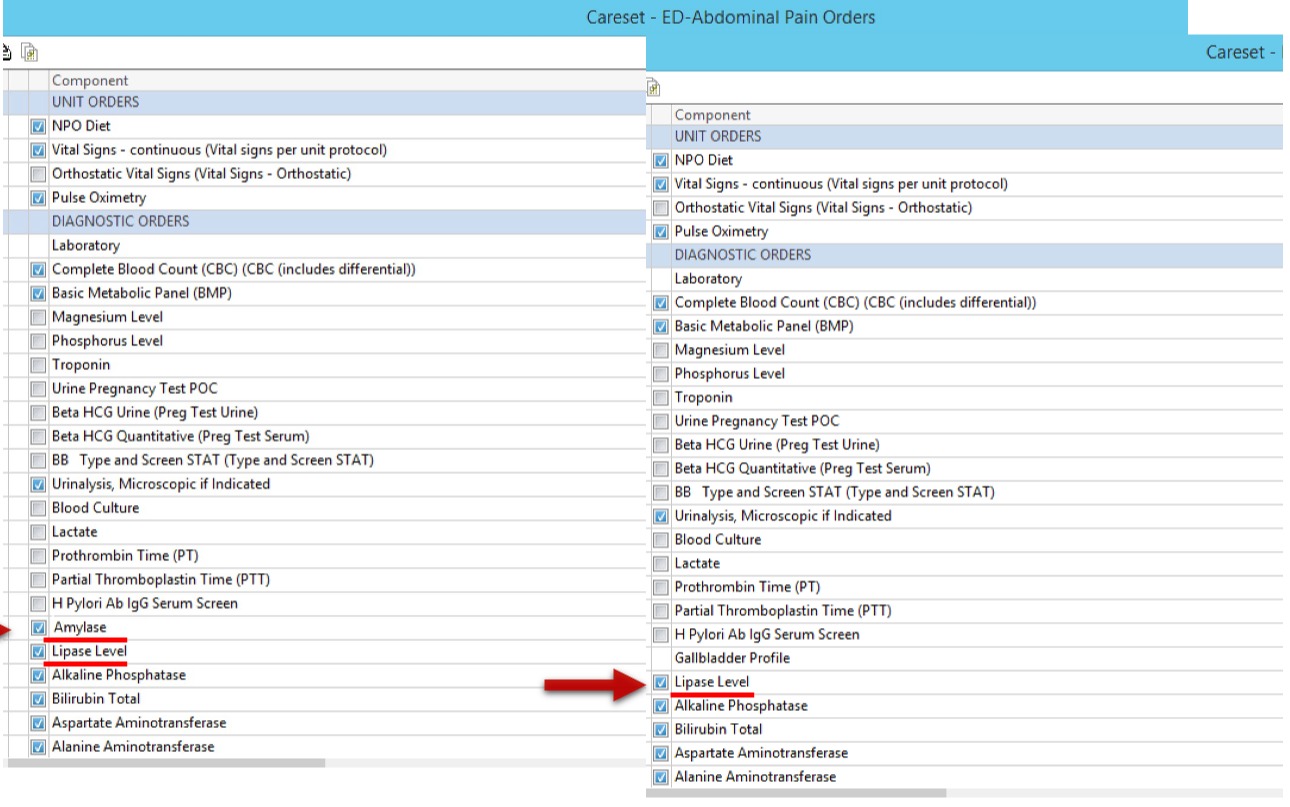
Figure: We were successful in removing amylase from the order set. Providers could still select the test, but with no pre-selection.
Disclosures:
Vatsal Khanna indicated no relevant financial relationships.
Alaa Taha indicated no relevant financial relationships.
Ranim Chamseddin indicated no relevant financial relationships.
Yashar Eshman indicated no relevant financial relationships.
Vesna Tegeltija indicated no relevant financial relationships.
Vatsal Khanna, MD1, Alaa Taha, MD1, Ranim Chamseddin, MD2, Yashar Eshman, MD1, Vesna Tegeltija, MD1. C0002 - Overutilization of Amylase and Lipase Testing in Acute Pancreatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

