Back
Poster Session C - Monday Afternoon
C0045 - Unusual Picture of Pancreatic Abscess in a Patient With a Near-Total Distal Pancreatectomy
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Anas Mahmoud, MD
Saint Joseph's University Medical Center
Paterson, NJ
Presenting Author(s)
Anas Mahmoud, MD, Abdalla Mohamed, MD, Matthew Grossman, MD
Saint Joseph's University Medical Center, Paterson, NJ
Introduction: Pancreatic abscess is an infection of the pancreatic pseudocyst which usually occurs 4 weeks after the onset of acute pancreatitis, meanwhile other causes include but are not limited to chronic pancreatitis, iatrogenic intra-abdominal procedures, and seeding from distant sites. We hereby report a case of an unusual occurrence of pancreatic abscess in a patient with a near-total distal pancreatectomy.
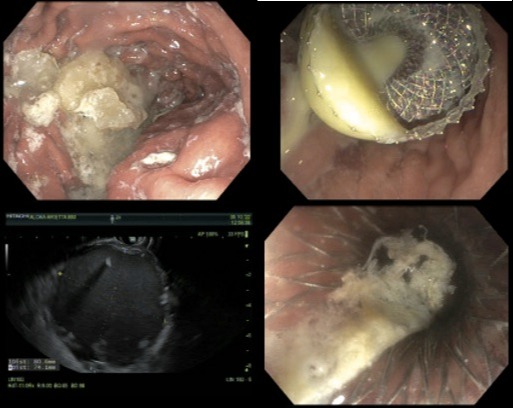
Case Description/Methods: Patient is a 56-year old male with past medical history of diabetes, pancreatic adenocarcinoma, status post near-total distal pancreatectomy 6 months earlier, pancreatic pseudocyst found 3 months ago and splenectomy presented with persistent progressive worsening left upper abdominal non-radiating pain, associated with nausea, eight episodes of bilious vomiting, abdominal distension and chills. Patient denied fever. Vitals and labs were insignificant. CT scan of the abdomen showed significant increase in the size of the pancreatic cyst by the head of the pancreas with gastric outlet obstruction. Patient was started on Unasyn and the GI team proceeded to EGD/EUS and cystogastrostomy on the same day. A stent was placed [with drainage into the stomach], the cyst was aspirated, the collected purulent fluid (Figure1) was sent for culture which came back positive for klebsiella pneumoniae. Patient reported relief after the procedure and was discharged on ciprofloxacin for 2 weeks. After 3 weeks, a follow-up EGD was done for necrosectomy with removal of the stent.
Discussion: Pancreatic abscess is most commonly caused iatrogenically during management of necrotizing pancreatitis, however it can happen in absence of pancreatitis, secondary to biliary tract disease or duodenal disease. A high index of suspicion should be maintained in patients with acute pancreatitis, who don’t improve after initial management especially with high RANSON score, and chronic pancreatitis with persistent pain which can lead to systemic inflammatory response syndrome and death. CT is the gold standard in diagnosis with a higher sensitivity than ultrasonography, however a following fine needle aspiration, has a sensitivity of almost 100%, and is crucial to distinguish sterile inflammation from infection. Gram negative bacteria is most commonly found in aspirated fluids, however gram positive can be seen. Invasive surgical cystogastrostomy or cystoduodenostomy, depending on the location of the abscess, should not be delayed and have better outcomes than solo antibiotic therapy or endoscopic intervention.
Disclosures:
Anas Mahmoud, MD, Abdalla Mohamed, MD, Matthew Grossman, MD. C0045 - Unusual Picture of Pancreatic Abscess in a Patient With a Near-Total Distal Pancreatectomy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Saint Joseph's University Medical Center, Paterson, NJ
Introduction: Pancreatic abscess is an infection of the pancreatic pseudocyst which usually occurs 4 weeks after the onset of acute pancreatitis, meanwhile other causes include but are not limited to chronic pancreatitis, iatrogenic intra-abdominal procedures, and seeding from distant sites. We hereby report a case of an unusual occurrence of pancreatic abscess in a patient with a near-total distal pancreatectomy.
Case Description/Methods: Patient is a 56-year old male with past medical history of diabetes, pancreatic adenocarcinoma, status post near-total distal pancreatectomy 6 months earlier, pancreatic pseudocyst found 3 months ago and splenectomy presented with persistent progressive worsening left upper abdominal non-radiating pain, associated with nausea, eight episodes of bilious vomiting, abdominal distension and chills. Patient denied fever. Vitals and labs were insignificant. CT scan of the abdomen showed significant increase in the size of the pancreatic cyst by the head of the pancreas with gastric outlet obstruction. Patient was started on Unasyn and the GI team proceeded to EGD/EUS and cystogastrostomy on the same day. A stent was placed [with drainage into the stomach], the cyst was aspirated, the collected purulent fluid (Figure1) was sent for culture which came back positive for klebsiella pneumoniae. Patient reported relief after the procedure and was discharged on ciprofloxacin for 2 weeks. After 3 weeks, a follow-up EGD was done for necrosectomy with removal of the stent.
Discussion: Pancreatic abscess is most commonly caused iatrogenically during management of necrotizing pancreatitis, however it can happen in absence of pancreatitis, secondary to biliary tract disease or duodenal disease. A high index of suspicion should be maintained in patients with acute pancreatitis, who don’t improve after initial management especially with high RANSON score, and chronic pancreatitis with persistent pain which can lead to systemic inflammatory response syndrome and death. CT is the gold standard in diagnosis with a higher sensitivity than ultrasonography, however a following fine needle aspiration, has a sensitivity of almost 100%, and is crucial to distinguish sterile inflammation from infection. Gram negative bacteria is most commonly found in aspirated fluids, however gram positive can be seen. Invasive surgical cystogastrostomy or cystoduodenostomy, depending on the location of the abscess, should not be delayed and have better outcomes than solo antibiotic therapy or endoscopic intervention.
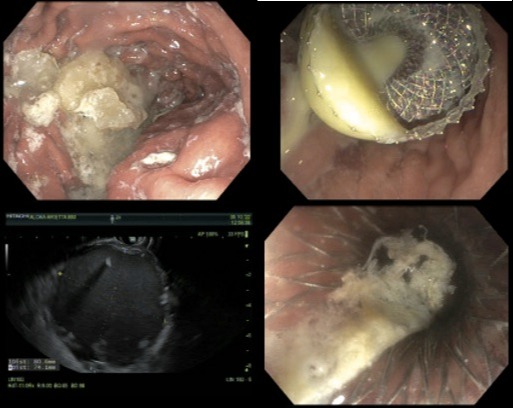
Figure: Figure 1
Disclosures:
Anas Mahmoud indicated no relevant financial relationships.
Abdalla Mohamed indicated no relevant financial relationships.
Matthew Grossman indicated no relevant financial relationships.
Anas Mahmoud, MD, Abdalla Mohamed, MD, Matthew Grossman, MD. C0045 - Unusual Picture of Pancreatic Abscess in a Patient With a Near-Total Distal Pancreatectomy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
