Back
Poster Session E - Tuesday Afternoon
E0080 - When Life Gives You Lemmel's, Call Your Gastroenterologist
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Jeremy Polman, DO, MS, MBA
Baton Rouge General Medical Center
Baton Rouge, LA
Presenting Author(s)
Gabrielle Sanford, MD1, Jeremy Polman, DO, MS, MBA2, Douglas Walsh, MD3
1LSUHSC Baton Rouge Internal Medicine Residency Program at Our Lady of the Lake, Baton Rouge, LA; 2Baton Rouge General Medical Center, Baton Rouge, LA; 3GI Alliance, Baton Rouge, LA
Introduction: Lemmel’s syndrome is defined as obstructive jaundice caused by periampullary duodenal diverticulum (PAD), leading to bile duct compression and dilation. PAD leading to the obstruction of the ampulla of Vater is the most common, with an incidence as high as 27%. Most PAD are found incidentally and are suspected to be found in up to 22% of the population, however, some patients can have life-threatening pathology, necessitating quick intervention. This case outlines a patient with this rare pathology and discusses when to choose specific therapeutic options.
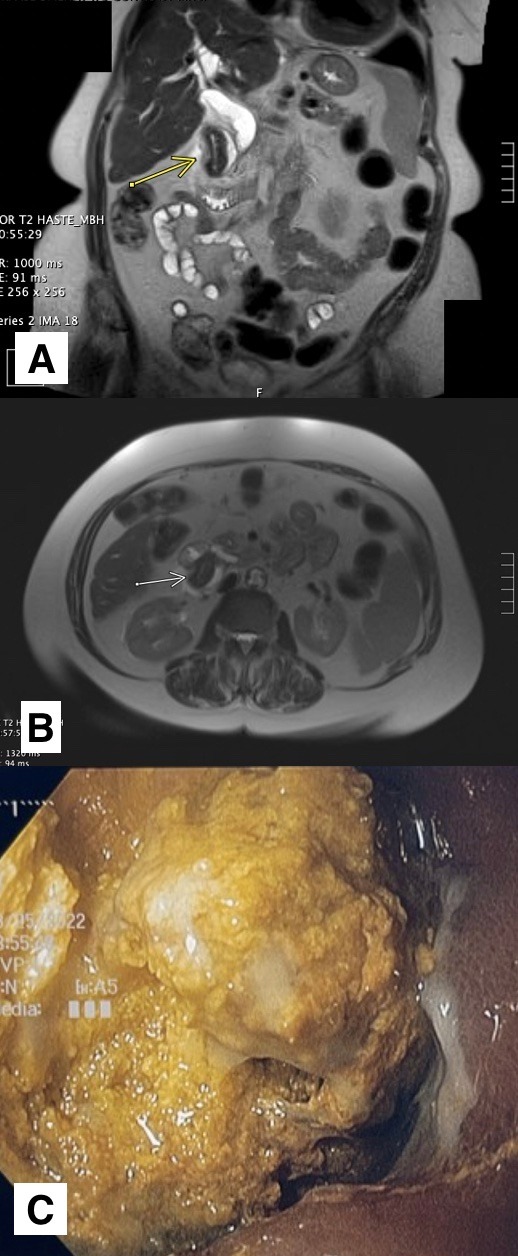
Case Description/Methods: A 77-year-old Caucasian female with a history of cholecystectomy 20 years ago presented to the emergency department with a 1-day history of epigastric abdominal pain, mild fever, jaundice, and non-bloody diarrhea. Laboratory evaluation was notable for a lipase of 3326 U/L and transaminitis with ALP 908 IU/L, AST 234 U/L, ALT 153 U/L, and total bilirubin 7.2 mg/dL. CT abdomen with IV contrast revealed moderate-severe pancreatitis and intra/extrahepatic biliary ductal dilation up to 19 mm in diameter with additional dilation of the pancreatic duct. A subsequent MRCP revealed a large periampullary duodenal diverticulum with obstruction of the common bile duct, consistent with Lemmel’s syndrome, and possible duodenal diverticulitis [A, B]. Piperacillin-tazobactam was initiated due to concern for ascending cholangitis and diverticulitis. ERCP was performed the following morning, which revealed a large duodenal diverticulum in the second portion of the duodenum with fecalized material impacted within the diverticulum [C]. The entire biliary ampulla was obscured by obstructing material and surrounding ulceration was noted. Several attempts to remove the impaction were unsuccessful. A temporary PTC drain was placed with interval improvement in her pain and lab abnormalities. The patient was transferred to another facility for advanced endoscopy, where she had successful removal of obstruction and intra/extrahepatic stenting.
Discussion: Therapeutic options vary, but ERCP is considered the initial treatment of choice because it allows for the placement of a biliary stent and a sphincterotomy. If Lemmel’s is due to chronic papillary fibrosis or sphincter of Oddi dysfunction, then an endoscopic sphincterotomy is the preferred therapy. If the disease is severe or complicated, a diverticulectomy is recommended in patients who are at lower risk for adverse complications.
Disclosures:
Gabrielle Sanford, MD1, Jeremy Polman, DO, MS, MBA2, Douglas Walsh, MD3. E0080 - When Life Gives You Lemmel's, Call Your Gastroenterologist, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1LSUHSC Baton Rouge Internal Medicine Residency Program at Our Lady of the Lake, Baton Rouge, LA; 2Baton Rouge General Medical Center, Baton Rouge, LA; 3GI Alliance, Baton Rouge, LA
Introduction: Lemmel’s syndrome is defined as obstructive jaundice caused by periampullary duodenal diverticulum (PAD), leading to bile duct compression and dilation. PAD leading to the obstruction of the ampulla of Vater is the most common, with an incidence as high as 27%. Most PAD are found incidentally and are suspected to be found in up to 22% of the population, however, some patients can have life-threatening pathology, necessitating quick intervention. This case outlines a patient with this rare pathology and discusses when to choose specific therapeutic options.
Case Description/Methods: A 77-year-old Caucasian female with a history of cholecystectomy 20 years ago presented to the emergency department with a 1-day history of epigastric abdominal pain, mild fever, jaundice, and non-bloody diarrhea. Laboratory evaluation was notable for a lipase of 3326 U/L and transaminitis with ALP 908 IU/L, AST 234 U/L, ALT 153 U/L, and total bilirubin 7.2 mg/dL. CT abdomen with IV contrast revealed moderate-severe pancreatitis and intra/extrahepatic biliary ductal dilation up to 19 mm in diameter with additional dilation of the pancreatic duct. A subsequent MRCP revealed a large periampullary duodenal diverticulum with obstruction of the common bile duct, consistent with Lemmel’s syndrome, and possible duodenal diverticulitis [A, B]. Piperacillin-tazobactam was initiated due to concern for ascending cholangitis and diverticulitis. ERCP was performed the following morning, which revealed a large duodenal diverticulum in the second portion of the duodenum with fecalized material impacted within the diverticulum [C]. The entire biliary ampulla was obscured by obstructing material and surrounding ulceration was noted. Several attempts to remove the impaction were unsuccessful. A temporary PTC drain was placed with interval improvement in her pain and lab abnormalities. The patient was transferred to another facility for advanced endoscopy, where she had successful removal of obstruction and intra/extrahepatic stenting.
Discussion: Therapeutic options vary, but ERCP is considered the initial treatment of choice because it allows for the placement of a biliary stent and a sphincterotomy. If Lemmel’s is due to chronic papillary fibrosis or sphincter of Oddi dysfunction, then an endoscopic sphincterotomy is the preferred therapy. If the disease is severe or complicated, a diverticulectomy is recommended in patients who are at lower risk for adverse complications.
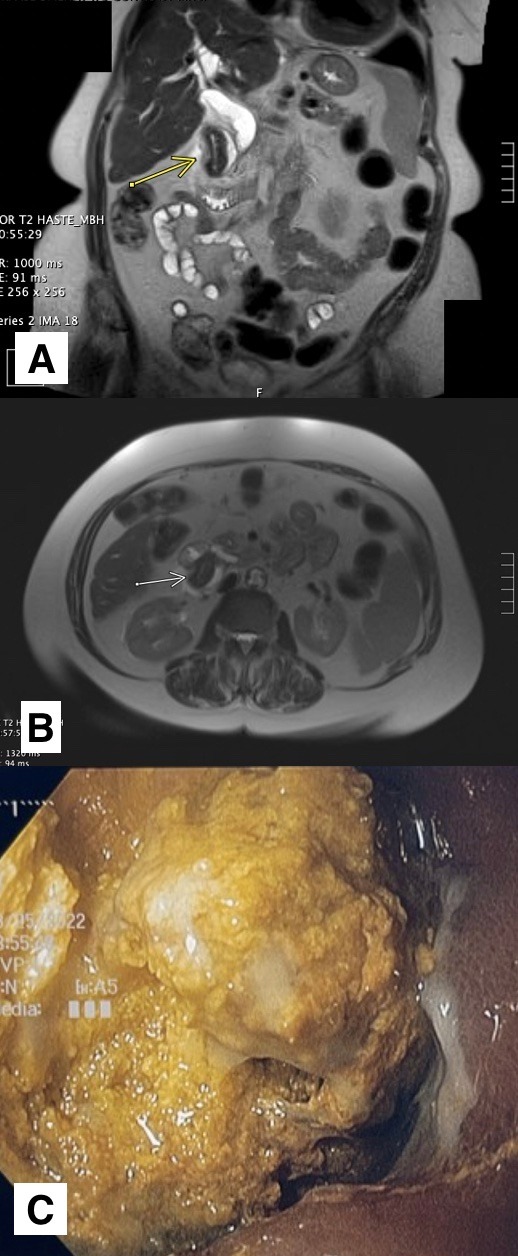
Figure: A) Coronal slice from MRI abdomen and pelvis demonstrating a large periampullary duodenal diverticulum with obstruction of the common bile duct.
B) Transverse slice from MRI abdomen and pelvis demonstrating a large periampullary duodenal diverticulum with obstruction of the common bile duct.
C) Image obtained during ERCP revealing impacted fecalized material within a large duodenal diverticulum in the second portion of the duodenum with surrounding ulceration.
B) Transverse slice from MRI abdomen and pelvis demonstrating a large periampullary duodenal diverticulum with obstruction of the common bile duct.
C) Image obtained during ERCP revealing impacted fecalized material within a large duodenal diverticulum in the second portion of the duodenum with surrounding ulceration.
Disclosures:
Gabrielle Sanford indicated no relevant financial relationships.
Jeremy Polman indicated no relevant financial relationships.
Douglas Walsh indicated no relevant financial relationships.
Gabrielle Sanford, MD1, Jeremy Polman, DO, MS, MBA2, Douglas Walsh, MD3. E0080 - When Life Gives You Lemmel's, Call Your Gastroenterologist, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
