Back
Poster Session E - Tuesday Afternoon
E0059 - Diabetic Ketoacidosis as a Rare Complication of Alcoholic Pancreatitis in a Previously Euglycemic Patient
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Kameron Tavakolian, MD
Jersey Shore University Medical Center
Neptune, NJ
Presenting Author(s)
Kameron Tavakolian, MD1, Sarah Elmedani, MD1, Andrew Ravin, DO1, Mihir Odak, MD2, Raquel Ong, MD1
1Jersey Shore University Medical Center, Neptune, NJ; 2Jersey Shore University Medical Center, Monroe Township, NJ
Introduction: Acute alcoholic pancreatitis is an acute inflammation of the pancreas secondary to alcohol intake due to autodigestion from an increase in pancreatic enzyme release. Most commonly due to gallstones, alcohol intake, and hypertriglyceridemia, pancreatitis commonly presents with severe epigastric abdominal pain, nausea and vomiting and is managed with aggressive intravenous (IV) fluid resuscitation. Some complications include acute respiratory distress syndrome and compartment syndrome. A very rare complication of acute pancreatitis is diabetic ketoacidosis (DKA), especially in patients without a history of diabetes mellitus.
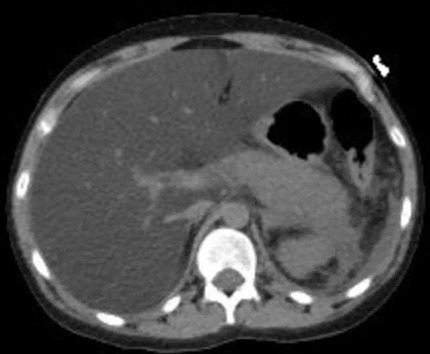
Case Description/Methods: A 25-year-old female with a medical history significant for alcohol abuse presented with nausea, vomiting, and abdominal pain for 2 days. The patient reported drinking one pint of liquor per day. She was tachycardic with a heart rate of 115 and other vitals were normal. Significant laboratory studies showed a lipase of 1715, aspartate transaminase of 292, alanine transaminase of 155, glucose of 540, venous pH of 7.277, bicarbonate of 9, anion gap of 21, and beta-hydroxybutyrate of 5.1. A computed tomography scan of her abdomen and pelvis without IV contrast showed edematous and inflammatory changes in the tail of the pancreas and severe hepatic steatosis. The patient was managed with aggressive IV fluids and IV insulin infusion. Her abdominal pain and anion gap resolved on day 2 of admission and she was able to tolerate a diet. Glycated hemoglobin (HbA1c) returned a value of 4.7 and C-peptide was low at < 0.10; the subsequent pancreatic antibody panel was negative. The patient was seen in the clinic 6 months later and HbA1c at that time was 4.8.
Discussion: This case illustrates DKA as a rare complication of acute pancreatitis. It provides an example of why a high level of suspicion for DKA should be present in patients presenting with alcoholic pancreatitis even in the absence of any diabetic history. Though there is no definitive mechanism of action for this presentation, it is likely from a combination of pancreatic beta-cell destruction and counter-regulatory hormone effects. Pancreatic beta-cell destruction causes impaired insulin production, leading to acute hyperglycemia. Furthermore, as acute pancreatitis can lead to severe intravascular depletion, increased secretion of counter-regulatory hormones such as cortisol and glucagon, in combination with impaired insulin secretion, can precipitate DKA in such a scenario.
Disclosures:
Kameron Tavakolian, MD1, Sarah Elmedani, MD1, Andrew Ravin, DO1, Mihir Odak, MD2, Raquel Ong, MD1. E0059 - Diabetic Ketoacidosis as a Rare Complication of Alcoholic Pancreatitis in a Previously Euglycemic Patient, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Jersey Shore University Medical Center, Neptune, NJ; 2Jersey Shore University Medical Center, Monroe Township, NJ
Introduction: Acute alcoholic pancreatitis is an acute inflammation of the pancreas secondary to alcohol intake due to autodigestion from an increase in pancreatic enzyme release. Most commonly due to gallstones, alcohol intake, and hypertriglyceridemia, pancreatitis commonly presents with severe epigastric abdominal pain, nausea and vomiting and is managed with aggressive intravenous (IV) fluid resuscitation. Some complications include acute respiratory distress syndrome and compartment syndrome. A very rare complication of acute pancreatitis is diabetic ketoacidosis (DKA), especially in patients without a history of diabetes mellitus.
Case Description/Methods: A 25-year-old female with a medical history significant for alcohol abuse presented with nausea, vomiting, and abdominal pain for 2 days. The patient reported drinking one pint of liquor per day. She was tachycardic with a heart rate of 115 and other vitals were normal. Significant laboratory studies showed a lipase of 1715, aspartate transaminase of 292, alanine transaminase of 155, glucose of 540, venous pH of 7.277, bicarbonate of 9, anion gap of 21, and beta-hydroxybutyrate of 5.1. A computed tomography scan of her abdomen and pelvis without IV contrast showed edematous and inflammatory changes in the tail of the pancreas and severe hepatic steatosis. The patient was managed with aggressive IV fluids and IV insulin infusion. Her abdominal pain and anion gap resolved on day 2 of admission and she was able to tolerate a diet. Glycated hemoglobin (HbA1c) returned a value of 4.7 and C-peptide was low at < 0.10; the subsequent pancreatic antibody panel was negative. The patient was seen in the clinic 6 months later and HbA1c at that time was 4.8.
Discussion: This case illustrates DKA as a rare complication of acute pancreatitis. It provides an example of why a high level of suspicion for DKA should be present in patients presenting with alcoholic pancreatitis even in the absence of any diabetic history. Though there is no definitive mechanism of action for this presentation, it is likely from a combination of pancreatic beta-cell destruction and counter-regulatory hormone effects. Pancreatic beta-cell destruction causes impaired insulin production, leading to acute hyperglycemia. Furthermore, as acute pancreatitis can lead to severe intravascular depletion, increased secretion of counter-regulatory hormones such as cortisol and glucagon, in combination with impaired insulin secretion, can precipitate DKA in such a scenario.
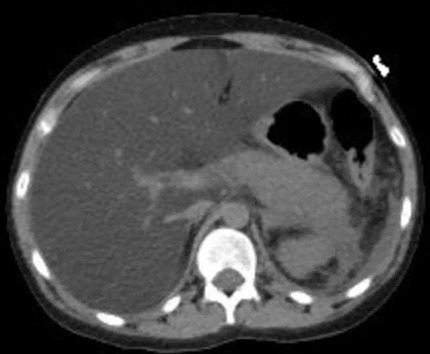
Figure: CT abdomen without contrast demonstrating edematous and inflammatory changes in the tail of the pancreas.
Disclosures:
Kameron Tavakolian indicated no relevant financial relationships.
Sarah Elmedani indicated no relevant financial relationships.
Andrew Ravin indicated no relevant financial relationships.
Mihir Odak indicated no relevant financial relationships.
Raquel Ong indicated no relevant financial relationships.
Kameron Tavakolian, MD1, Sarah Elmedani, MD1, Andrew Ravin, DO1, Mihir Odak, MD2, Raquel Ong, MD1. E0059 - Diabetic Ketoacidosis as a Rare Complication of Alcoholic Pancreatitis in a Previously Euglycemic Patient, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
