Back
Poster Session C - Monday Afternoon
C0044 - Immunoglobulin G4-Associated Cholangitis Mimicking Cholangiocarcinoma in Elderly
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Anas Mahmoud, MD
Saint Joseph's University Medical Center
Paterson, NJ
Presenting Author(s)
Anas Mahmoud, MD, Mina Fransawy Alkomos, MD, Abdalla Mohamed, MD, Shaker Barham, MD, Yana Cavanagh, MD, Matthew Grossman, MD
Saint Joseph's University Medical Center, Paterson, NJ
Introduction: Sclerosing cholangitis is a diffuse inflammation and fibrosis that progressively leads to stenosis and destruction of the bile ducts. It includes three types: primary sclerosing cholangitis (PSC), secondary cholangitis, and IgG4 sclerosing cholangitis (IgG4-SC). Usually they all present with cholestatic symptoms like pruritus and abdominal pain along with elevated ALP and GGT as well as bilirubin, however IgG4-SC has better outcomes, treatment response to steroids and less recurrence. We hereby presenting a case of IgG4-SC presenting as cholangiocarcinoma.
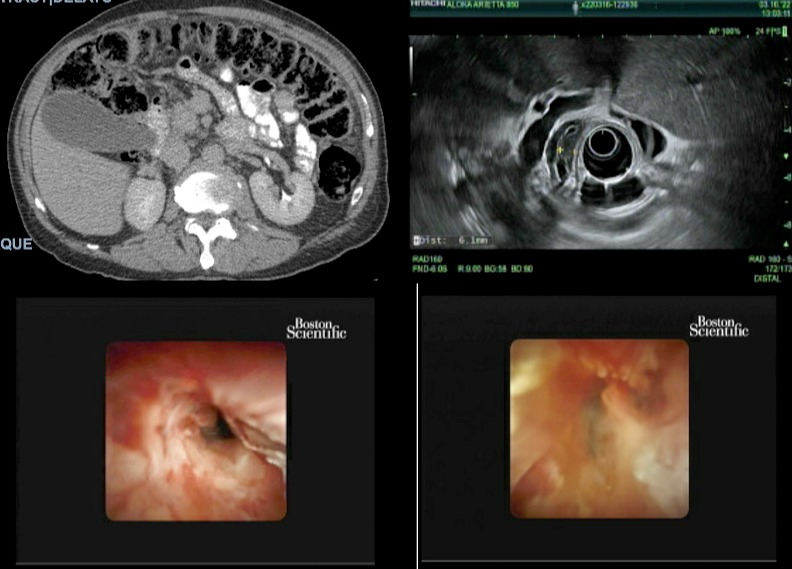
Case Description/Methods: An 80 year-old male with a past medical history of bladder cancer was referred to the gastroenterology for EUS after blood work showed (ALT 320, AST 297, Bilirubin 1.4, GGT 2032), and CT abdomen with IV contrast revealed intra and extrahepatic biliary dilatation with an abrupt cutoff in mid CBD, suspicious for either a primary CBD mass or pancreatic mass (Figure 1). EUS showed an irregular mass in the CBD wall, suspicious for cholangiocarcinoma (Figure 1). The ERCP showed malignant appearing stricture of the extrahepatic bile duct consistent with cholangiocarcinoma, Bismuth 2 vs early 3B (Figure 1). Exploratory laparotomy was done and portal node biopsy came back benign; for which a repeat ERCP/Spyglass with direct visualization cholangioscopy, was done and showed diffusely dilated main bile duct with sludge and pus, single diffuse stenosis in right hepatic duct sludge with lining malignant appearing abnormal mucosa (nodularity and dilated vessels). IgG4 was elevated (931) consistent with IgG4 cholangitis (Figure 1). Biopsy and cytology brush showed no signs of dysplasia or neoplasia. Patient was then started on prednisone for a month and scheduled to repeat ERCP/Spyglass after.
Discussion: IgG4-RD is a fibrous-inflammatory process related to immunomodulation, therefore IgG4-SC often co-presents with auto-immune pancreatitis, dacryoadenitis and sialadenitis. IgG4-SC is extremely challenging, as it’s frequently misdiagnosed on imaging as a pseudotumor, and can progress to liver cirrhosis if left untreated, however it comes with great response to steroids. In 2021, Mendoza criteria (tortuous vessels, irregular nodulations, raised intraductal lesions, irregular surface, and friability) was published and found to be accurate to differentiate malignant and benign causes of biliary stricture, with overall diagnostic accuracy of 77%. Our case didn’t meet the 5 criterias of Mendoza, which is consistent with IgG4-SC.
Disclosures:
Anas Mahmoud, MD, Mina Fransawy Alkomos, MD, Abdalla Mohamed, MD, Shaker Barham, MD, Yana Cavanagh, MD, Matthew Grossman, MD. C0044 - Immunoglobulin G4-Associated Cholangitis Mimicking Cholangiocarcinoma in Elderly, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Saint Joseph's University Medical Center, Paterson, NJ
Introduction: Sclerosing cholangitis is a diffuse inflammation and fibrosis that progressively leads to stenosis and destruction of the bile ducts. It includes three types: primary sclerosing cholangitis (PSC), secondary cholangitis, and IgG4 sclerosing cholangitis (IgG4-SC). Usually they all present with cholestatic symptoms like pruritus and abdominal pain along with elevated ALP and GGT as well as bilirubin, however IgG4-SC has better outcomes, treatment response to steroids and less recurrence. We hereby presenting a case of IgG4-SC presenting as cholangiocarcinoma.
Case Description/Methods: An 80 year-old male with a past medical history of bladder cancer was referred to the gastroenterology for EUS after blood work showed (ALT 320, AST 297, Bilirubin 1.4, GGT 2032), and CT abdomen with IV contrast revealed intra and extrahepatic biliary dilatation with an abrupt cutoff in mid CBD, suspicious for either a primary CBD mass or pancreatic mass (Figure 1). EUS showed an irregular mass in the CBD wall, suspicious for cholangiocarcinoma (Figure 1). The ERCP showed malignant appearing stricture of the extrahepatic bile duct consistent with cholangiocarcinoma, Bismuth 2 vs early 3B (Figure 1). Exploratory laparotomy was done and portal node biopsy came back benign; for which a repeat ERCP/Spyglass with direct visualization cholangioscopy, was done and showed diffusely dilated main bile duct with sludge and pus, single diffuse stenosis in right hepatic duct sludge with lining malignant appearing abnormal mucosa (nodularity and dilated vessels). IgG4 was elevated (931) consistent with IgG4 cholangitis (Figure 1). Biopsy and cytology brush showed no signs of dysplasia or neoplasia. Patient was then started on prednisone for a month and scheduled to repeat ERCP/Spyglass after.
Discussion: IgG4-RD is a fibrous-inflammatory process related to immunomodulation, therefore IgG4-SC often co-presents with auto-immune pancreatitis, dacryoadenitis and sialadenitis. IgG4-SC is extremely challenging, as it’s frequently misdiagnosed on imaging as a pseudotumor, and can progress to liver cirrhosis if left untreated, however it comes with great response to steroids. In 2021, Mendoza criteria (tortuous vessels, irregular nodulations, raised intraductal lesions, irregular surface, and friability) was published and found to be accurate to differentiate malignant and benign causes of biliary stricture, with overall diagnostic accuracy of 77%. Our case didn’t meet the 5 criterias of Mendoza, which is consistent with IgG4-SC.
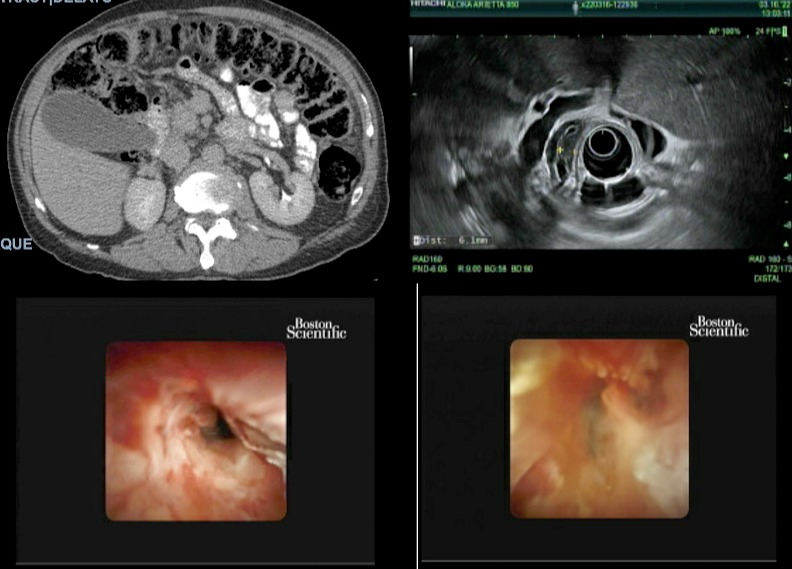
Figure: Figure 1
Disclosures:
Anas Mahmoud indicated no relevant financial relationships.
Mina Fransawy Alkomos indicated no relevant financial relationships.
Abdalla Mohamed indicated no relevant financial relationships.
Shaker Barham indicated no relevant financial relationships.
Yana Cavanagh indicated no relevant financial relationships.
Matthew Grossman indicated no relevant financial relationships.
Anas Mahmoud, MD, Mina Fransawy Alkomos, MD, Abdalla Mohamed, MD, Shaker Barham, MD, Yana Cavanagh, MD, Matthew Grossman, MD. C0044 - Immunoglobulin G4-Associated Cholangitis Mimicking Cholangiocarcinoma in Elderly, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
