Back
Poster Session E - Tuesday Afternoon
E0019 - Impact of Frailty on Readmissions and Inpatient Outcomes of Older Adults (≥65 Years) With Acute Pancreatitis
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Muhammad Sheharyar Warraich, MD, MBBS
John H. Stroger Jr. Hospital of Cook County
Chicago, IL
Presenting Author(s)
Muhammad Sheharyar Warraich, MD, MBBS1, Dae Y. Park, MD2, Michelle Ishaya, DO2, Hisham Laswi, MD2, Shazaq Khalid, MBBS3, Bashar Attar, MD2
1John H. Stroger Jr. Hospital of Cook County, Chicago, IL; 2John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 3Punjab Medical College, Chicago, IL
Introduction: Acute pancreatitis (AP) is a major cause of adult hospitalizations in the United States. More than 10 billion US dollars are spent each year on treatment of patients admitted for AP. While data on hospitalizations for AP is widely analyzed, there are limited studies regarding the role that frailty has on this group of patients. The goal of our study is to determine what impact patient frailty has on readmission and on inpatient outcomes.
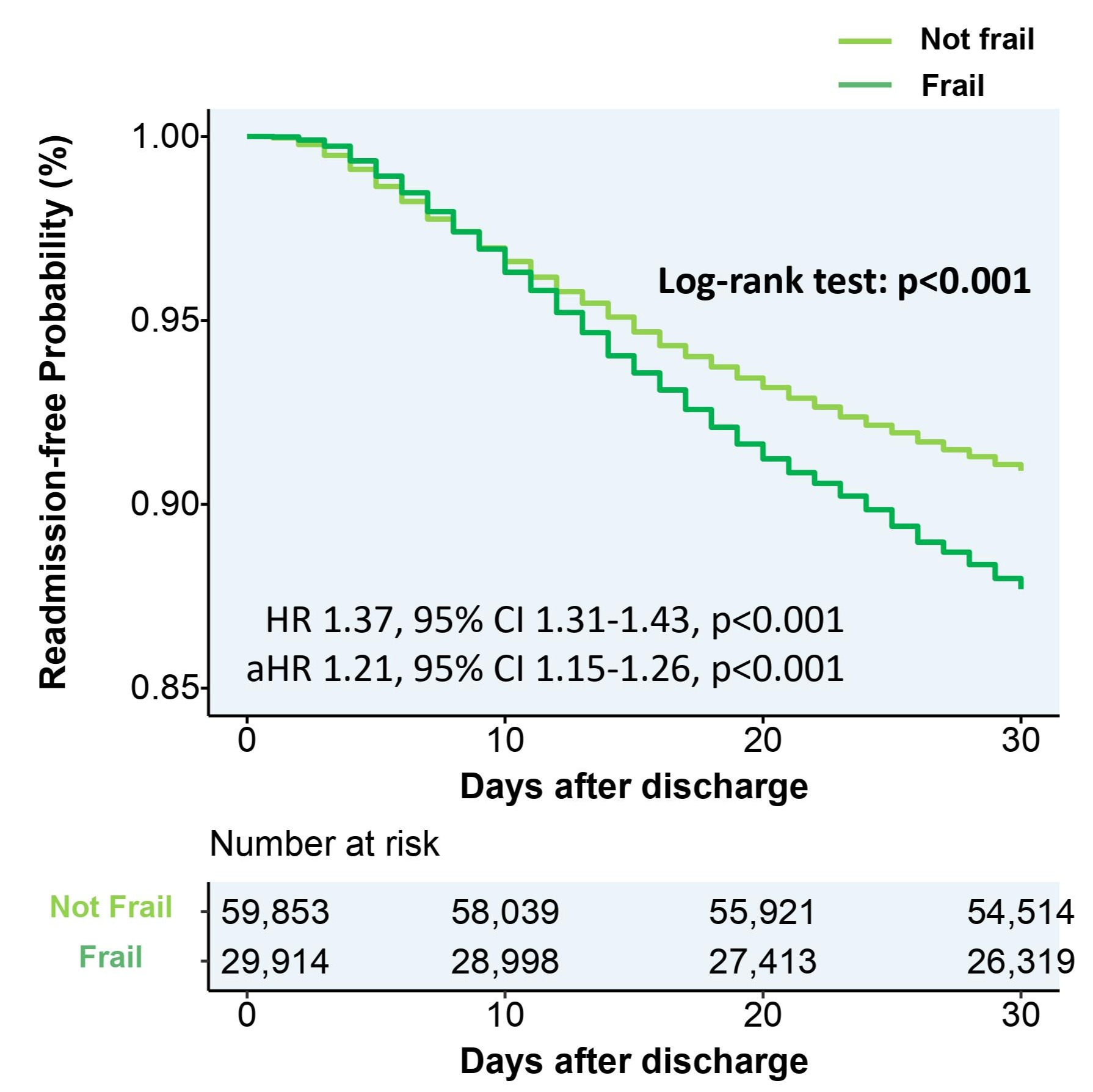
Methods: The National Readmission Database (NRD) 2017-18 was queried. AP patients age >= 65 were selected based on appropriate ICD-10 diagnostic codes. Hospital frailty risk score (HFRS) was calculated for all the AP patients such that patients with HFRS score < 5 were considered to be not frail (NF) and patients with HFRS score >= 5 were considered frail based on the prevalence of comorbidities in each individual. Differences in mean length of stay (LOS) and in-hospital mortality were analyzed using multivariate logistic regression. Cox proportional-hazards regression analysis was used to determine the difference in 30-day readmission between the two groups.
Results: A total of 91,031 patients aged 65 years and older with AP were identified in our search. Of these, 31,012 (mean age 76.5) were considered frail (average HFRS score 8.2) and the remaining 60,020 (mean age 74.1) were deemed to be not frail (average HFRS score 2.1). The rate of in-patient mortality was significantly higher in the frail group compared to the not frail group (3.53% vs 0.27%) with an adjusted odds ratio of 10.95 (p < 0.001). Frail AP patients had a significantly longer LOS when compared to NF (6.8 vs 3.6 days; adjusted mean difference 2.6 days, p < 0.001). The difference in 30-day readmission rates between the frail and NF group was also highly statistically significant; (12.0% vs 8.9%, respectively; adjusted hazard ratio 1.2%, 95% CI 1.15-1.26%; p < 0.001).
Discussion: AP patients consume a great deal of healthcare resources and the burden is increasing due to the aging population. Our study finds that the elderly frail group of AP patients is more fragile and has a higher 30-day readmission rate. It would be prudent to risk stratify patients admitted with AP and devise a more customized treatment approach for the more vulnerable frail group, in hopes of reducing inpatient mortality and lessening the burden on our healthcare system that results from longer stays and readmissions.
Disclosures:
Muhammad Sheharyar Warraich, MD, MBBS1, Dae Y. Park, MD2, Michelle Ishaya, DO2, Hisham Laswi, MD2, Shazaq Khalid, MBBS3, Bashar Attar, MD2. E0019 - Impact of Frailty on Readmissions and Inpatient Outcomes of Older Adults (≥65 Years) With Acute Pancreatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1John H. Stroger Jr. Hospital of Cook County, Chicago, IL; 2John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 3Punjab Medical College, Chicago, IL
Introduction: Acute pancreatitis (AP) is a major cause of adult hospitalizations in the United States. More than 10 billion US dollars are spent each year on treatment of patients admitted for AP. While data on hospitalizations for AP is widely analyzed, there are limited studies regarding the role that frailty has on this group of patients. The goal of our study is to determine what impact patient frailty has on readmission and on inpatient outcomes.
Methods: The National Readmission Database (NRD) 2017-18 was queried. AP patients age >= 65 were selected based on appropriate ICD-10 diagnostic codes. Hospital frailty risk score (HFRS) was calculated for all the AP patients such that patients with HFRS score < 5 were considered to be not frail (NF) and patients with HFRS score >= 5 were considered frail based on the prevalence of comorbidities in each individual. Differences in mean length of stay (LOS) and in-hospital mortality were analyzed using multivariate logistic regression. Cox proportional-hazards regression analysis was used to determine the difference in 30-day readmission between the two groups.
Results: A total of 91,031 patients aged 65 years and older with AP were identified in our search. Of these, 31,012 (mean age 76.5) were considered frail (average HFRS score 8.2) and the remaining 60,020 (mean age 74.1) were deemed to be not frail (average HFRS score 2.1). The rate of in-patient mortality was significantly higher in the frail group compared to the not frail group (3.53% vs 0.27%) with an adjusted odds ratio of 10.95 (p < 0.001). Frail AP patients had a significantly longer LOS when compared to NF (6.8 vs 3.6 days; adjusted mean difference 2.6 days, p < 0.001). The difference in 30-day readmission rates between the frail and NF group was also highly statistically significant; (12.0% vs 8.9%, respectively; adjusted hazard ratio 1.2%, 95% CI 1.15-1.26%; p < 0.001).
Discussion: AP patients consume a great deal of healthcare resources and the burden is increasing due to the aging population. Our study finds that the elderly frail group of AP patients is more fragile and has a higher 30-day readmission rate. It would be prudent to risk stratify patients admitted with AP and devise a more customized treatment approach for the more vulnerable frail group, in hopes of reducing inpatient mortality and lessening the burden on our healthcare system that results from longer stays and readmissions.
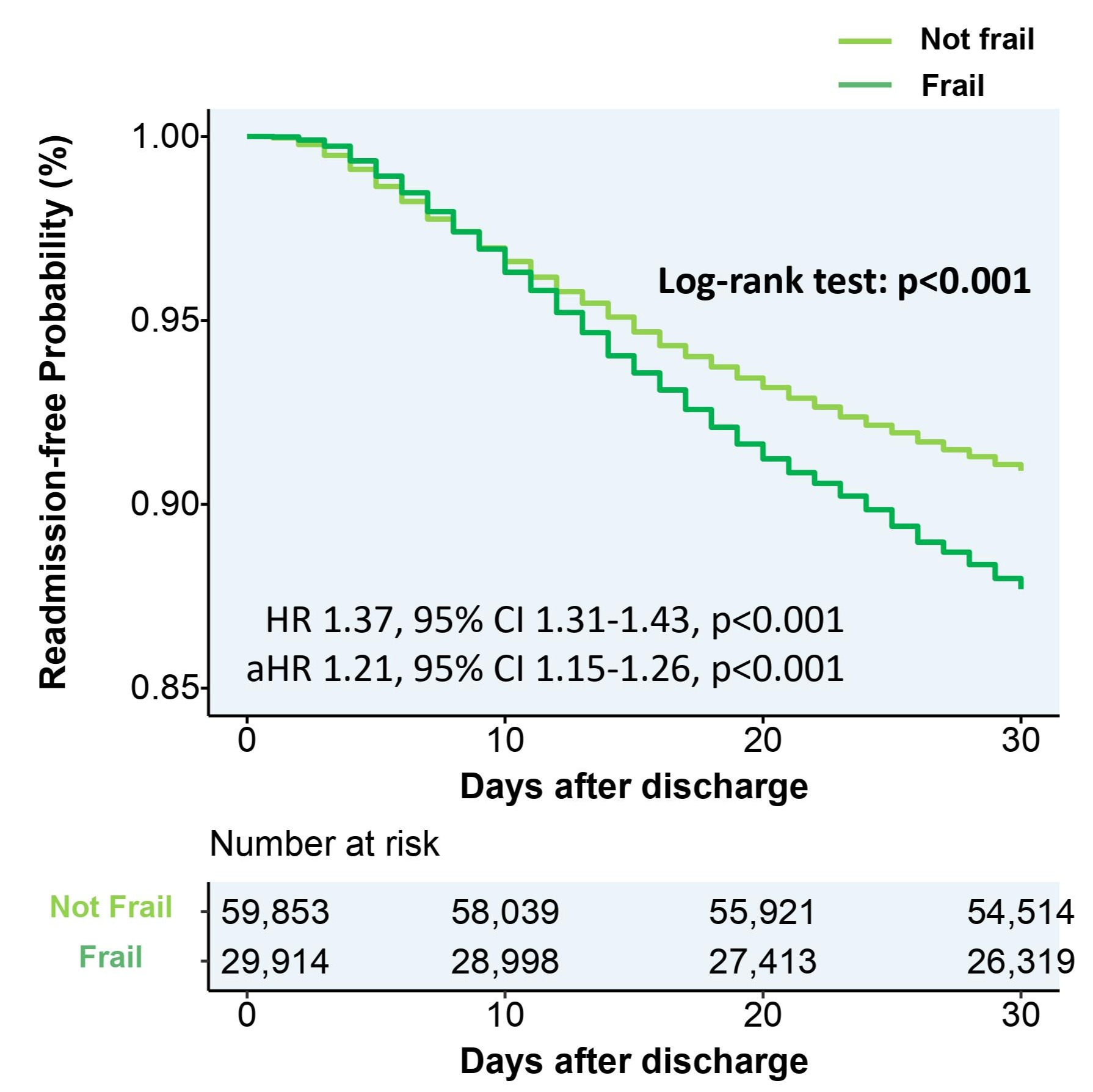
Figure: Kaplan-Meier curves of readmission after acute pancreatitis comparing the frail and not frail (NF) groups
Disclosures:
Muhammad Sheharyar Warraich indicated no relevant financial relationships.
Dae Park indicated no relevant financial relationships.
Michelle Ishaya indicated no relevant financial relationships.
Hisham Laswi indicated no relevant financial relationships.
Shazaq Khalid indicated no relevant financial relationships.
Bashar Attar indicated no relevant financial relationships.
Muhammad Sheharyar Warraich, MD, MBBS1, Dae Y. Park, MD2, Michelle Ishaya, DO2, Hisham Laswi, MD2, Shazaq Khalid, MBBS3, Bashar Attar, MD2. E0019 - Impact of Frailty on Readmissions and Inpatient Outcomes of Older Adults (≥65 Years) With Acute Pancreatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
