Back
Poster Session E - Tuesday Afternoon
E0020 - Insulin Therapy vs Plasmapheresis in Patients With Hypertriglyceridemia-Associated Pancreatitis: A Systematic Review and Meta-Analysis
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
.jpg)
Azizullah Beran, MD
University of Toledo
Toledo, OH
Presenting Author(s)
Azizullah Beran, MD1, Hazem Ayesh, MD2, Mohammed Mhanna, MD, MPH1, Wasef Sayeh, MD1, Mouhand F. Mohamed, MD, MSc3, Sami Ghazaleh, MD1, Rami Musallam, MD4, Khaled Elfert, MD, MRCP5, Sehrish Malik, MD1, Mohammad Al-Haddad, MD, MSc6
1University of Toledo, Toledo, OH; 2Vanderbilt University Medical Center, Nashville, TN; 3Warren Alpert Medical School of Brown University, Providence, RI; 4St. Vincent Charity Medical Center, Cleveland, OH; 5SBH Health System, New York, NY; 6Indiana University School of Medicine, Indianapolis, IN
Introduction: Insulin therapy (IT) and plasmapheresis are used to treat hypertriglyceridemia-associated pancreatitis (HTAP). However, the optimal treatment modality for lowering the triglyceride level in patients with HTAP remains unclear. Therefore, we evaluated the efficacy and safety of IT and plasmapheresis in managing HTAP.
Methods: We performed a comprehensive literature search using PubMed, Embase, and Web of Science databases through May 30, 2022, for all studies that compared IT vs. plasmapheresis in patients with HTAP. The primary outcomes were effectiveness (reduction in triglycerides within 24-hours of admission) and clinical outcomes, including hospital length-of-stay (LOS), mortality, acute renal failure (ARF), hypotension, and need for invasive mechanical ventilation (IMV). The secondary outcome was the overall treatment-related adverse events (AEs). Random-effects meta-analysis was conducted, and risk ratio (RR) and mean difference (MD) or standardized mean difference (SMD) for proportional and continuous variables were computed, respectively. For each outcome, forest plot, 95% confidence interval (CI), P-value (< 0.05 considered statistically significant), and I2 statistic ( > 50% considered as significant heterogeneity) were generated.
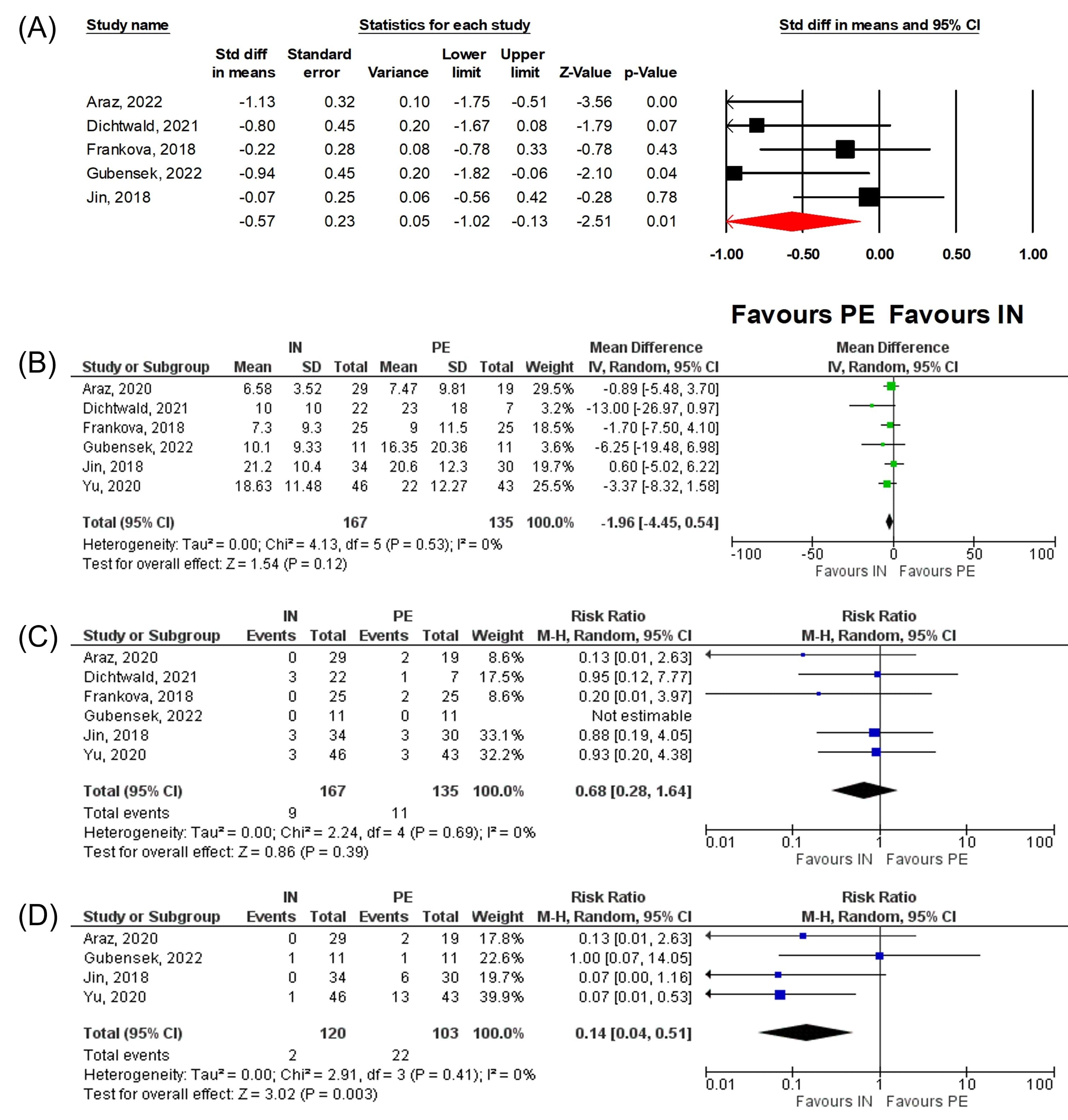
Results: Six studies (1 randomized controlled trial [RCT] and 5 cohort studies) with 302 patients with HTAP (167 on IT vs. 135 on plasmapheresis) were included. Plasmapheresis was more effective than IT in reduction of triglycerides within 24-hours (SMD -0.57; 95% CI -1.02, -0.13; P=0.01, I2=56.8%, Figure 1A). However, LOS (MD -1.96; 95% CI -4.45, 0.54; P=0.12; I2=0%, Figure 1B), mortality (RR 0.68, 95% CI 0.28-1.64, P=0.39, I2=0%, Figure 1C), ARF (RR 0.44, 95% CI 0.06-3.05, P=0.41, I2=84%), hypotension (RR 0.63, 95% CI 0.16-2.52, P=0.51, I2=79%), and need for IMV (RR 0.52, 95% CI 0.12-12.35, P=0.40, I2=80%) were similar between two groups. The treatment-related AEs were significantly lower in IT than plasmapheresis (RR 0.14, 95% CI 0.04-0.51, P=0.003, I2=0%, Figure 1D).
Discussion: Our meta-analysis demonstrated that despite the greater reduction of triglycerides with plasmapheresis compared to insulin therapy, the clinical outcomes, including LOS, mortality, ARF, hypotension, and need for IMV, were comparable with lower treatment-related adverse events with insulin therapy. Future large-scale RCTs are necessary to validate our findings.
Disclosures:
Azizullah Beran, MD1, Hazem Ayesh, MD2, Mohammed Mhanna, MD, MPH1, Wasef Sayeh, MD1, Mouhand F. Mohamed, MD, MSc3, Sami Ghazaleh, MD1, Rami Musallam, MD4, Khaled Elfert, MD, MRCP5, Sehrish Malik, MD1, Mohammad Al-Haddad, MD, MSc6. E0020 - Insulin Therapy vs Plasmapheresis in Patients With Hypertriglyceridemia-Associated Pancreatitis: A Systematic Review and Meta-Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Toledo, Toledo, OH; 2Vanderbilt University Medical Center, Nashville, TN; 3Warren Alpert Medical School of Brown University, Providence, RI; 4St. Vincent Charity Medical Center, Cleveland, OH; 5SBH Health System, New York, NY; 6Indiana University School of Medicine, Indianapolis, IN
Introduction: Insulin therapy (IT) and plasmapheresis are used to treat hypertriglyceridemia-associated pancreatitis (HTAP). However, the optimal treatment modality for lowering the triglyceride level in patients with HTAP remains unclear. Therefore, we evaluated the efficacy and safety of IT and plasmapheresis in managing HTAP.
Methods: We performed a comprehensive literature search using PubMed, Embase, and Web of Science databases through May 30, 2022, for all studies that compared IT vs. plasmapheresis in patients with HTAP. The primary outcomes were effectiveness (reduction in triglycerides within 24-hours of admission) and clinical outcomes, including hospital length-of-stay (LOS), mortality, acute renal failure (ARF), hypotension, and need for invasive mechanical ventilation (IMV). The secondary outcome was the overall treatment-related adverse events (AEs). Random-effects meta-analysis was conducted, and risk ratio (RR) and mean difference (MD) or standardized mean difference (SMD) for proportional and continuous variables were computed, respectively. For each outcome, forest plot, 95% confidence interval (CI), P-value (< 0.05 considered statistically significant), and I2 statistic ( > 50% considered as significant heterogeneity) were generated.
Results: Six studies (1 randomized controlled trial [RCT] and 5 cohort studies) with 302 patients with HTAP (167 on IT vs. 135 on plasmapheresis) were included. Plasmapheresis was more effective than IT in reduction of triglycerides within 24-hours (SMD -0.57; 95% CI -1.02, -0.13; P=0.01, I2=56.8%, Figure 1A). However, LOS (MD -1.96; 95% CI -4.45, 0.54; P=0.12; I2=0%, Figure 1B), mortality (RR 0.68, 95% CI 0.28-1.64, P=0.39, I2=0%, Figure 1C), ARF (RR 0.44, 95% CI 0.06-3.05, P=0.41, I2=84%), hypotension (RR 0.63, 95% CI 0.16-2.52, P=0.51, I2=79%), and need for IMV (RR 0.52, 95% CI 0.12-12.35, P=0.40, I2=80%) were similar between two groups. The treatment-related AEs were significantly lower in IT than plasmapheresis (RR 0.14, 95% CI 0.04-0.51, P=0.003, I2=0%, Figure 1D).
Discussion: Our meta-analysis demonstrated that despite the greater reduction of triglycerides with plasmapheresis compared to insulin therapy, the clinical outcomes, including LOS, mortality, ARF, hypotension, and need for IMV, were comparable with lower treatment-related adverse events with insulin therapy. Future large-scale RCTs are necessary to validate our findings.
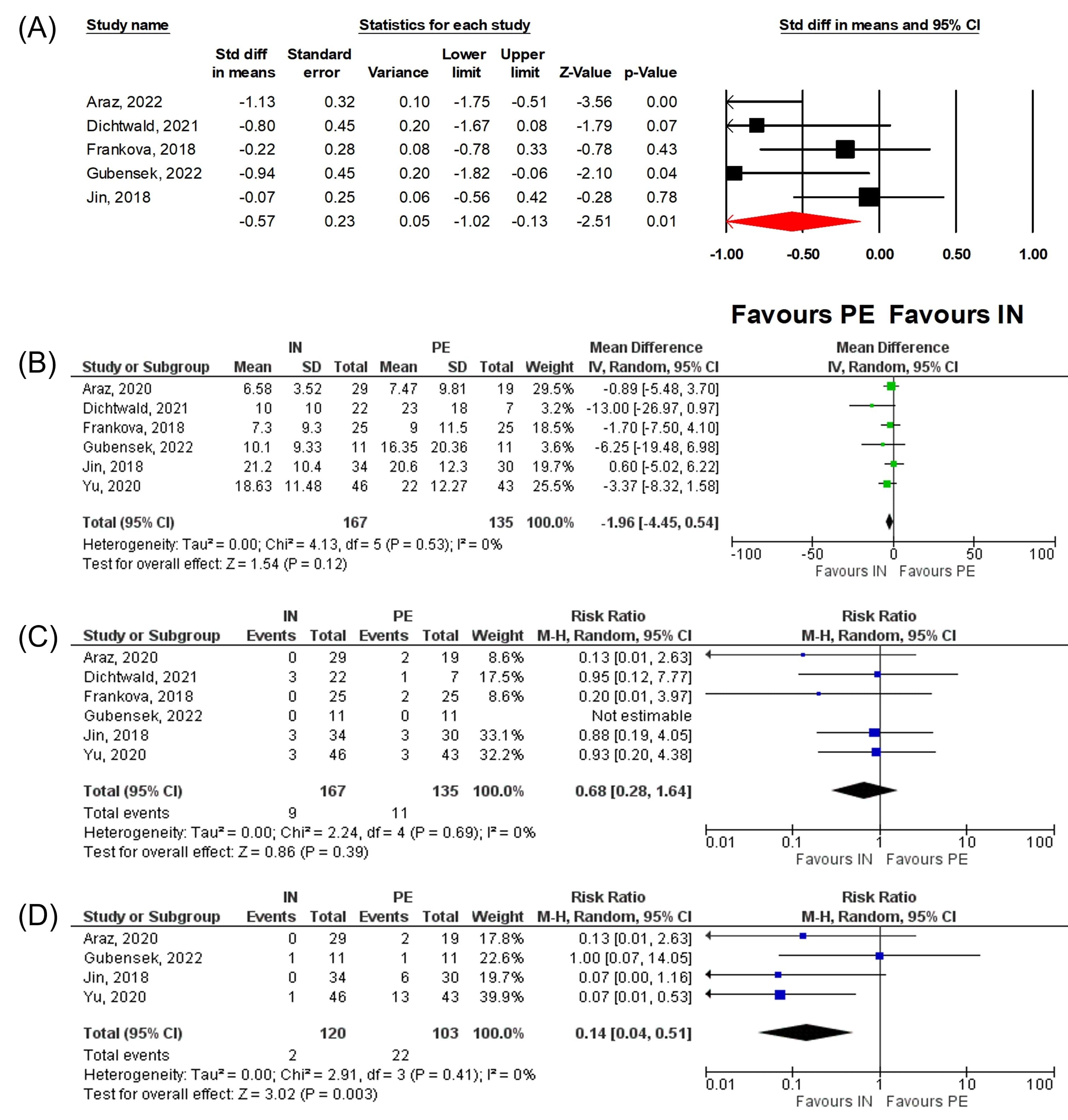
Figure: Figure 1: Forest plots comparing between insulin therapy and plasmapheresis regarding: (A) the reduction of triglyceride within 24 hours, (B) length of hospital stay, (C) mortality, and (D) treatment-related adverse events.
Disclosures:
Azizullah Beran indicated no relevant financial relationships.
Hazem Ayesh indicated no relevant financial relationships.
Mohammed Mhanna indicated no relevant financial relationships.
Wasef Sayeh indicated no relevant financial relationships.
Mouhand Mohamed indicated no relevant financial relationships.
Sami Ghazaleh indicated no relevant financial relationships.
Rami Musallam indicated no relevant financial relationships.
Khaled Elfert indicated no relevant financial relationships.
Sehrish Malik indicated no relevant financial relationships.
Mohammad Al-Haddad: Amplified sciences – Grant/Research Support. Cook endoscopy – Grant/Research Support. Creatics LLC – Grant/Research Support.
Azizullah Beran, MD1, Hazem Ayesh, MD2, Mohammed Mhanna, MD, MPH1, Wasef Sayeh, MD1, Mouhand F. Mohamed, MD, MSc3, Sami Ghazaleh, MD1, Rami Musallam, MD4, Khaled Elfert, MD, MRCP5, Sehrish Malik, MD1, Mohammad Al-Haddad, MD, MSc6. E0020 - Insulin Therapy vs Plasmapheresis in Patients With Hypertriglyceridemia-Associated Pancreatitis: A Systematic Review and Meta-Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
