Back
Poster Session E - Tuesday Afternoon
E0504 - Clostridium difficile Infection Increases In-Hospital Mortality, Length of Stay, and Hospital Cost but Not 30-Day Mortality in Cirrhotic Patients: A Systematic Review and Meta-Analysis
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Aunchalee Jaroenlapnopparat, MBBS
Mount Auburn Hospital
Cambridge, MA
Presenting Author(s)
Aunchalee Jaroenlapnopparat, MD1, Nipith Charoenngam, MD1, Ben Ponvilawan, MD2, Palapun Waitayangkoon, MD3
1Mount Auburn Hospital/Beth Israel Lahey Health, Cambridge, MA; 2Taussig Cancer Institute, Cleveland Clinic, Cleveland, OH; 3Metrowest Medical Center, Framingham, MA
Introduction: Clostridium difficile infection (CDI) is a leading cause of nosocomial infection and is associated with higher morbidity and mortality. Cirrhotic patients are more susceptible to CDI because of impaired gut immune response, frequent hospitalization, and use of proton pump inhibitor and antibiotics. We aim to investigate the impact of CDI on cirrhotic patients in terms of in-hospital and 30-day mortality, length of stay, and hospital cost.
Methods: Potentially eligible studies were identified from Embase, Medline, and Web of Sciences databases from inception to April 2022 using search strategy that comprised of terms for “cirrhosis” and “CDI”. Eligible study must consist of one group of cirrhotic patients with CDI and control group of cirrhotic patients without CDI. The study must provide odds ratio (OR) and 95% confidence interval (95% CI). We extracted such data from each study to calculate mean difference (MD) or OR. Pooled MD/OR were then calculated by combining MD/OR of each study using random-effects model. Funnel plot was used to assess for the presence of publication bias.
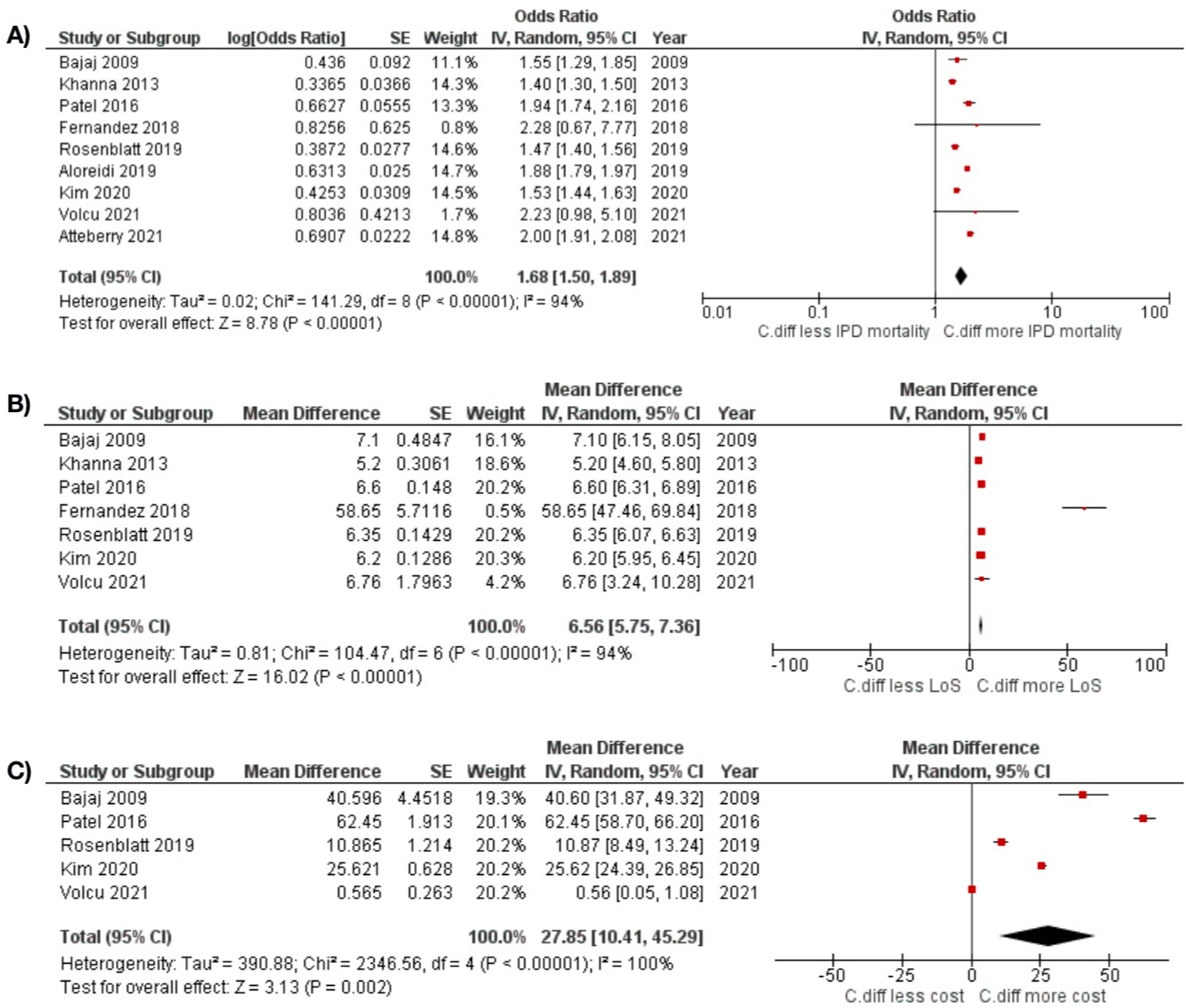
Results: A total of 2,320 articles were identified. After two rounds of independent review by two investigators, nine studies reporting in-hospital mortality and three reporting 30-day mortality of cirrhotic patients with CDI versus those without CDI were included into the meta-analysis. The meta-analysis of nine studies consisting of 7,746,126 patients revealed a significant association between CDI and in-hospital mortality in cirrhotic patients with the pooled OR of 1.68 (95%CI 1.29-1.85, I2 94%, Figure 1A). Length of stay and hospital cost were also higher in the CDI group (pooled MD of 6.56 days [95% CI 5.75-7.36, I2 94%, Figure 1B] and 27.85 (x $1,000) [95% CI 10.41-45.29, I2 100%, Figure 1C] consecutively). The funnel plot for the meta-analysis of the association between CDI and in-hospital mortality was fairly symmetric and was not suggestive of publication bias. From three studies comprising of 3,694 patients, we found that CDI was not associated with 30-day mortality in cirrhotic patients (pooled OR 1.20, 95%CI 0.75-2.24, I2 74%).
Discussion: CDI is associated with increased in-hospital mortality, length of stay, and hospital costs, but not with 30-day mortality in cirrhotic patients. Aggressive monitoring for CDI during admission is needed in this patient population.
Disclosures:
Aunchalee Jaroenlapnopparat, MD1, Nipith Charoenngam, MD1, Ben Ponvilawan, MD2, Palapun Waitayangkoon, MD3. E0504 - Clostridium difficile Infection Increases In-Hospital Mortality, Length of Stay, and Hospital Cost but Not 30-Day Mortality in Cirrhotic Patients: A Systematic Review and Meta-Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Mount Auburn Hospital/Beth Israel Lahey Health, Cambridge, MA; 2Taussig Cancer Institute, Cleveland Clinic, Cleveland, OH; 3Metrowest Medical Center, Framingham, MA
Introduction: Clostridium difficile infection (CDI) is a leading cause of nosocomial infection and is associated with higher morbidity and mortality. Cirrhotic patients are more susceptible to CDI because of impaired gut immune response, frequent hospitalization, and use of proton pump inhibitor and antibiotics. We aim to investigate the impact of CDI on cirrhotic patients in terms of in-hospital and 30-day mortality, length of stay, and hospital cost.
Methods: Potentially eligible studies were identified from Embase, Medline, and Web of Sciences databases from inception to April 2022 using search strategy that comprised of terms for “cirrhosis” and “CDI”. Eligible study must consist of one group of cirrhotic patients with CDI and control group of cirrhotic patients without CDI. The study must provide odds ratio (OR) and 95% confidence interval (95% CI). We extracted such data from each study to calculate mean difference (MD) or OR. Pooled MD/OR were then calculated by combining MD/OR of each study using random-effects model. Funnel plot was used to assess for the presence of publication bias.
Results: A total of 2,320 articles were identified. After two rounds of independent review by two investigators, nine studies reporting in-hospital mortality and three reporting 30-day mortality of cirrhotic patients with CDI versus those without CDI were included into the meta-analysis. The meta-analysis of nine studies consisting of 7,746,126 patients revealed a significant association between CDI and in-hospital mortality in cirrhotic patients with the pooled OR of 1.68 (95%CI 1.29-1.85, I2 94%, Figure 1A). Length of stay and hospital cost were also higher in the CDI group (pooled MD of 6.56 days [95% CI 5.75-7.36, I2 94%, Figure 1B] and 27.85 (x $1,000) [95% CI 10.41-45.29, I2 100%, Figure 1C] consecutively). The funnel plot for the meta-analysis of the association between CDI and in-hospital mortality was fairly symmetric and was not suggestive of publication bias. From three studies comprising of 3,694 patients, we found that CDI was not associated with 30-day mortality in cirrhotic patients (pooled OR 1.20, 95%CI 0.75-2.24, I2 74%).
Discussion: CDI is associated with increased in-hospital mortality, length of stay, and hospital costs, but not with 30-day mortality in cirrhotic patients. Aggressive monitoring for CDI during admission is needed in this patient population.
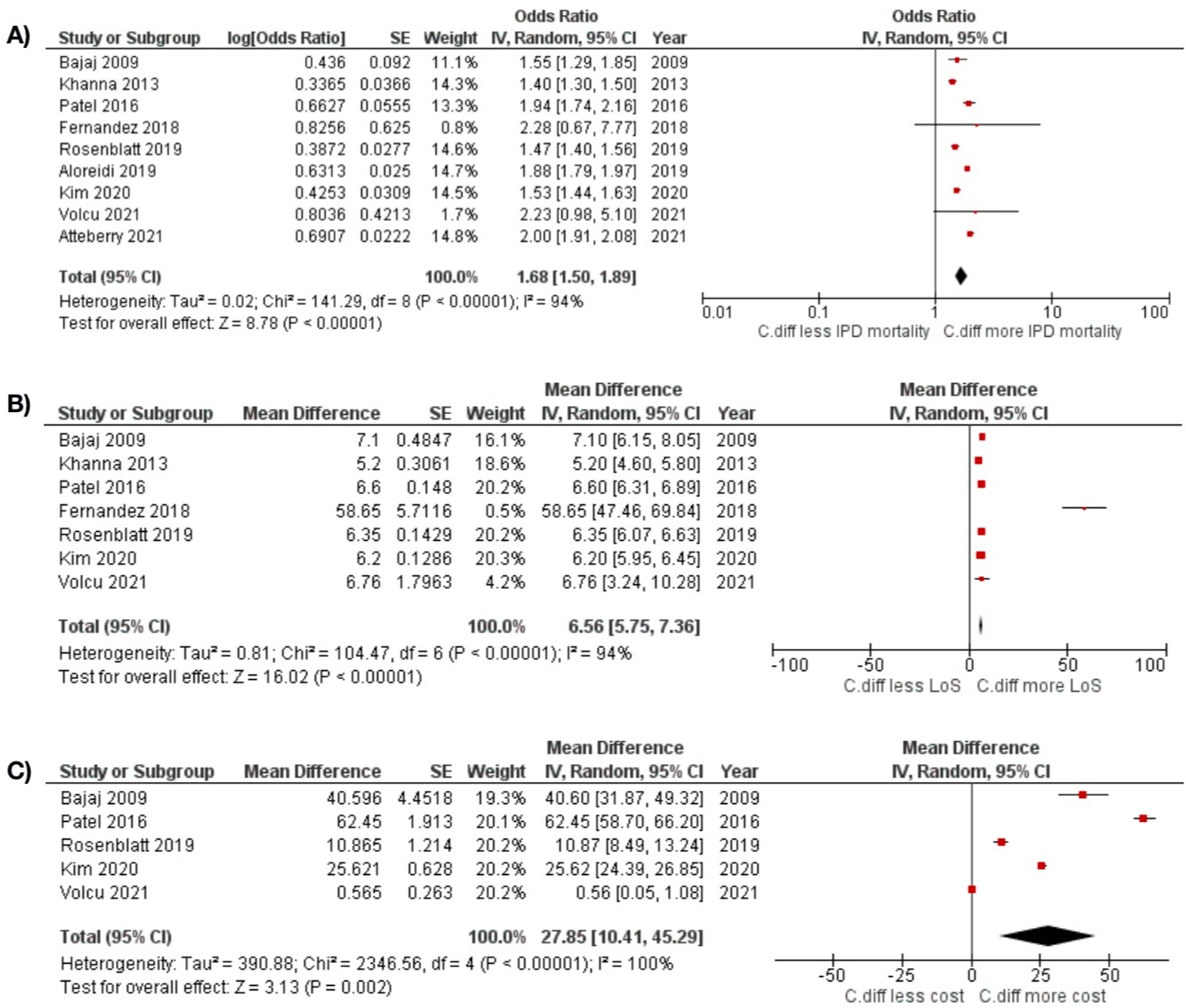
Figure: Figure 1) Forest plot of the associations between CDI in cirrhotic patients and A) in-hospital mortality, B) length of stay, C) hospital cost
Disclosures:
Aunchalee Jaroenlapnopparat indicated no relevant financial relationships.
Nipith Charoenngam indicated no relevant financial relationships.
Ben Ponvilawan indicated no relevant financial relationships.
Palapun Waitayangkoon indicated no relevant financial relationships.
Aunchalee Jaroenlapnopparat, MD1, Nipith Charoenngam, MD1, Ben Ponvilawan, MD2, Palapun Waitayangkoon, MD3. E0504 - Clostridium difficile Infection Increases In-Hospital Mortality, Length of Stay, and Hospital Cost but Not 30-Day Mortality in Cirrhotic Patients: A Systematic Review and Meta-Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
