Back
Poster Session A - Sunday Afternoon
Category: Functional Bowel Disease
A0249 - Nutritional Aspects in Patients With Gastroparesis: Normal BMI Despite Abnormal Intake!
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
- RA
Rawan Aljaras, MD
Indiana University School of Medicine
Indianapolis, Indiana
Presenting Author(s)
Rawan Aljaras, MD1, Noor Abu-Farsakh, MD2, Renato Beas, MD3, Eleazar E. Montalvan-Sanchez, MD1, Maryam Haidar, MD4, Ahmad Karkash, MD3, Mirian Ramirez-Rojas, MLIS3, Gerardo Calderon, MD3
1Indiana University School of Medicine, Indianapolis, IN; 2Jordan University Hospital, Amman, 'Amman, Jordan; 3Indiana University, Indianapolis, IN; 4Detroit Medical Center - Sinai Grace, Indianapolis, IN
Introduction: Patients with gastroparesis have signs and symptoms including nausea, vomiting, and early satiety, thus leading to inadequate food intake and a high risk of malnutrition. The classic clinical picture of gastroparesis is a symptomatic patient losing weight. We performed a systematic review and a meta-analysis to identify average body mass index (BMI) in patients with gastroparesis.
Methods: Medline, Embase, Cochrane, CINAHL, and Scopus were searched for longitudinal studies reporting on nutrition in adult patients with gastroparesis. A search strategy was developed with core terms including “gastroparesis”, “BMI”, “calorie”, and “nutrition”. The main outcome was determined to be the average BMI in patients with gastroparesis. The secondary outcome was average calorie intake in these patients. Data was pooled and I^2 values were calculated to determine heterogeneity. No controls were identified for analysis.
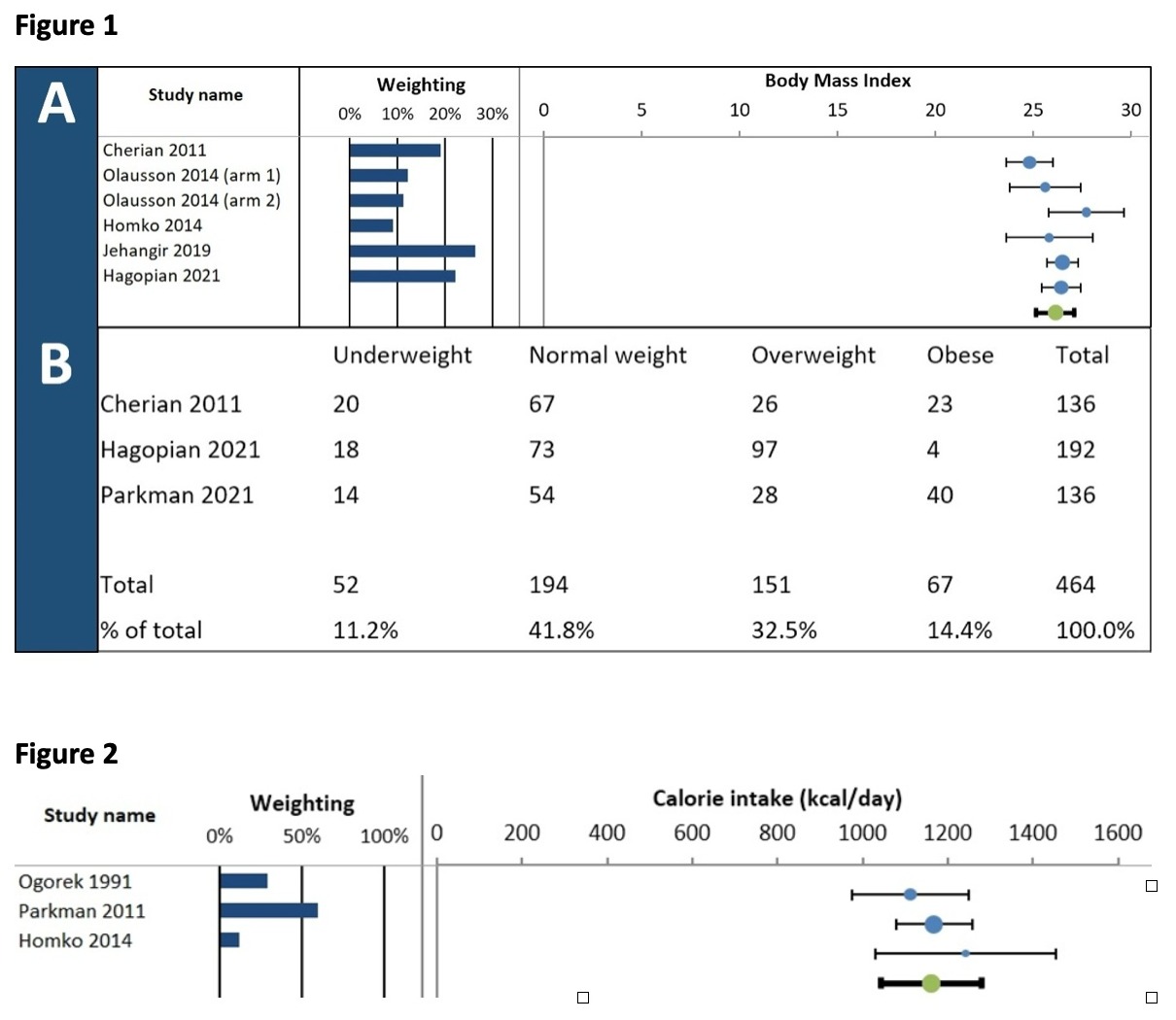
Results: Initial database search resulted in 3999 studies (n=3999). 16 relevant studies were identified for full text review (n=16). 5 studies were identified eligible to be included in the average BMI meta-analysis after applying inclusion and exclusion criteria (n=5). The weighted average BMI in patients with gastroparesis was calculated at (26.1 kg/m^2). Heterogeneity (I^2 value) for these studies was noted to be moderate at 46.7% (Figure 1A). 3 of the initial 16 studies identified for full review reported on distribution of patients with gastroparesis among different BMI categories with details shown in table (Figure 1B). Another 3 studies were identified eligible to be included in the average calorie intake meta-analysis (n=3). Weighted average calorie intake in patients with gastroparesis was calculated at (1161 kcal/day), forest plot is shown in (Figure 2).
Discussion: Weighted average BMI in patients with gastroparesis laid in the overweight category, with most patients noted of normal weight per distribution of patient’s prevalence per category of BMI (Figure 1B). These results contradict with what is commonly thought of these patients being likely underweight for their inability to meet dietary requirements. Average calorie intake in patients with gastroparesis is found to be less than the recommended daily intake for adult males and females in the US. Reasons why patients are mostly of normal weight to overweight despite less than recommended daily calorie intake are not well understood and more investigations of other factors affecting BMI in these patients is warranted.
Disclosures:
Rawan Aljaras, MD1, Noor Abu-Farsakh, MD2, Renato Beas, MD3, Eleazar E. Montalvan-Sanchez, MD1, Maryam Haidar, MD4, Ahmad Karkash, MD3, Mirian Ramirez-Rojas, MLIS3, Gerardo Calderon, MD3. A0249 - Nutritional Aspects in Patients With Gastroparesis: Normal BMI Despite Abnormal Intake!, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Indiana University School of Medicine, Indianapolis, IN; 2Jordan University Hospital, Amman, 'Amman, Jordan; 3Indiana University, Indianapolis, IN; 4Detroit Medical Center - Sinai Grace, Indianapolis, IN
Introduction: Patients with gastroparesis have signs and symptoms including nausea, vomiting, and early satiety, thus leading to inadequate food intake and a high risk of malnutrition. The classic clinical picture of gastroparesis is a symptomatic patient losing weight. We performed a systematic review and a meta-analysis to identify average body mass index (BMI) in patients with gastroparesis.
Methods: Medline, Embase, Cochrane, CINAHL, and Scopus were searched for longitudinal studies reporting on nutrition in adult patients with gastroparesis. A search strategy was developed with core terms including “gastroparesis”, “BMI”, “calorie”, and “nutrition”. The main outcome was determined to be the average BMI in patients with gastroparesis. The secondary outcome was average calorie intake in these patients. Data was pooled and I^2 values were calculated to determine heterogeneity. No controls were identified for analysis.
Results: Initial database search resulted in 3999 studies (n=3999). 16 relevant studies were identified for full text review (n=16). 5 studies were identified eligible to be included in the average BMI meta-analysis after applying inclusion and exclusion criteria (n=5). The weighted average BMI in patients with gastroparesis was calculated at (26.1 kg/m^2). Heterogeneity (I^2 value) for these studies was noted to be moderate at 46.7% (Figure 1A). 3 of the initial 16 studies identified for full review reported on distribution of patients with gastroparesis among different BMI categories with details shown in table (Figure 1B). Another 3 studies were identified eligible to be included in the average calorie intake meta-analysis (n=3). Weighted average calorie intake in patients with gastroparesis was calculated at (1161 kcal/day), forest plot is shown in (Figure 2).
Discussion: Weighted average BMI in patients with gastroparesis laid in the overweight category, with most patients noted of normal weight per distribution of patient’s prevalence per category of BMI (Figure 1B). These results contradict with what is commonly thought of these patients being likely underweight for their inability to meet dietary requirements. Average calorie intake in patients with gastroparesis is found to be less than the recommended daily intake for adult males and females in the US. Reasons why patients are mostly of normal weight to overweight despite less than recommended daily calorie intake are not well understood and more investigations of other factors affecting BMI in these patients is warranted.
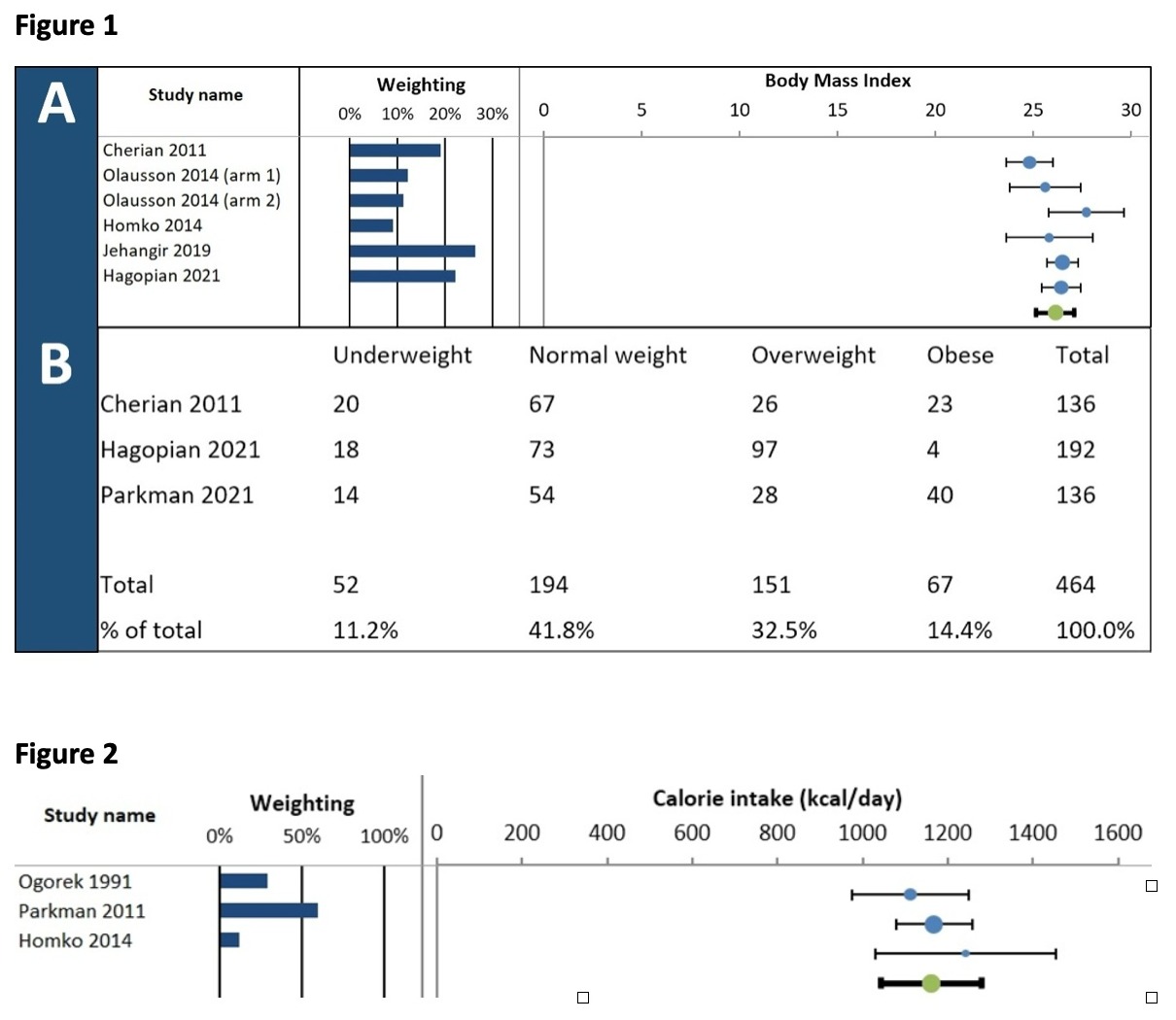
Figure: Figure 1:
A) Forest plot of average BMI in patients with gastroparesis meta-analysis
, B) Distribution of gastroparesis patients' prevalence among BMI categories
Figure 2 : Forest plot of average calorie intake in patients with gastroparesis meta-analysis.
Figure 2 : Forest plot of average calorie intake in patients with gastroparesis meta-analysis.
Disclosures:
Rawan Aljaras indicated no relevant financial relationships.
Noor Abu-Farsakh — NO DISCLOSURE DATA.
Noor Abu-Farsakh indicated no relevant financial relationships.
Renato Beas indicated no relevant financial relationships.
Eleazar Montalvan-Sanchez indicated no relevant financial relationships.
Maryam Haidar indicated no relevant financial relationships.
Ahmad Karkash indicated no relevant financial relationships.
Mirian Ramirez-Rojas indicated no relevant financial relationships.
Gerardo Calderon indicated no relevant financial relationships.
Rawan Aljaras, MD1, Noor Abu-Farsakh, MD2, Renato Beas, MD3, Eleazar E. Montalvan-Sanchez, MD1, Maryam Haidar, MD4, Ahmad Karkash, MD3, Mirian Ramirez-Rojas, MLIS3, Gerardo Calderon, MD3. A0249 - Nutritional Aspects in Patients With Gastroparesis: Normal BMI Despite Abnormal Intake!, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
