Back

Poster Session A - Sunday Afternoon
Category: General Endoscopy
A0265 - Clinical Course and Outcomes Following Dental Foreign Body Ingestion: Adverse Events and Need for Endoscopy
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Lucía Rivera Matos, MD
Rush University Medical Center
Louisville, KY
Presenting Author(s)
Lucía Rivera Matos, MD1, Mohammad El-Saied, MD2, Georgia Lymberopoulos, DMD, MPH3, Jennifer Bereckis, RDH, MS3, Susan A. Rowan, DDS, MS3, Anna M. Lipowska, MD2
1Rush University Medical Center, Chicago, IL; 2University of Illinois at Chicago, Chicago, IL; 3UIC College of Dentistry, Chicago, IL
Introduction: Foreign body ingestion during dental procedures is a rare complication that often requires medical evaluation and consideration for object extraction. There is scarcity of data in existing literature on patient outcomes and need for endoscopy after dental foreign body ingestion (DFBI). Given the uncommon presentation of DFBI, more information would aid gastroenterologists and hospital inpatient teams to help guide treatment plans. We aim to better define patient clinical course after DFBI and identify factors that may influence outcomes.
Methods: We conducted a retrospective review of DFBI cases at a tertiary care center between 2015 and 2021. Patients younger than 18 years old were excluded. Data was collected through electronic medical record review, including patient information, clinical course, imaging, interventions, and timeline.
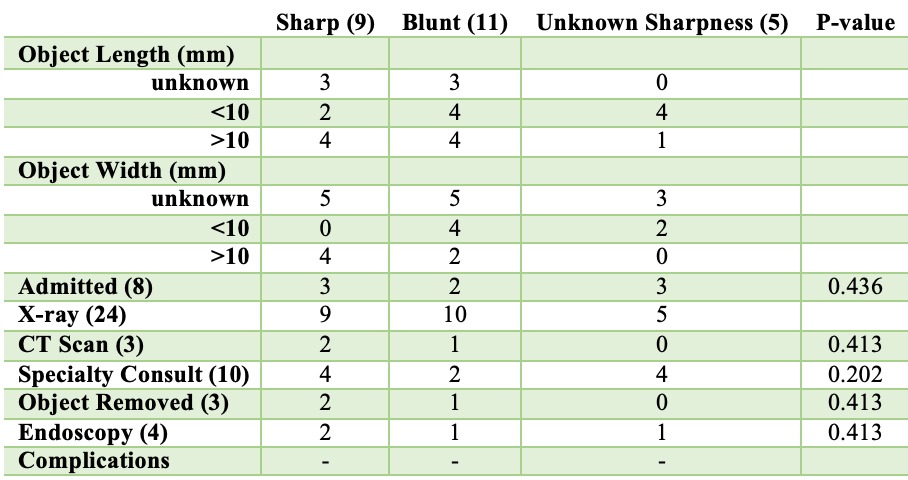
Results: 25 patients were included (56% male) from a diverse cohort (40% Caucasian, 20% African American, 8% Hispanic) and mean age of 64 (SD14.8). 1 patient had an ASA of ≥ 3. 3 individuals were symptomatic, foreign body sensation being most common. Most patients underwent imaging (n=24,96%), with all undergoing x-rays (100%), and 3 CT scans (12.5%). All objects were past the esophagus at time of evaluation and all patients were evaluated within 48hrs of ingestion. Gastroenterology was consulted for 9 (36%) patients and 8 (32%) were admitted to the hospital. 4 patients underwent endoscopy (16%) with object removal in 3 (12%); 0 required surgery. Endoscopy was associated with an increased likelihood of admission (p=0.047). Descriptive data was available on 19 DFB objects; the mean length was 13mm, 9 were sharp, and object sharpness was not found to be associated with requiring endoscopy (p=0.413) (Table 1). Both the complication and mortality rate of DFBI was 0% and all patients managed conservatively did well.
Discussion: This study examines a rare cohort of patients who experienced DFBI and provides better understanding of their clinical course to help guide care decisions. Our findings highlight that DFBI has mostly a benign clinical course and can likely be managed conservatively if the object is distal to the esophagus. While a number of DFBs are sharp, even those that were not retrieved passed uneventfully and without complications, likely due to their small size. No specific patient/object characteristics were associated with need for hospital admission, endoscopy, or increased rate of adverse events.
Disclosures:
Lucía Rivera Matos, MD1, Mohammad El-Saied, MD2, Georgia Lymberopoulos, DMD, MPH3, Jennifer Bereckis, RDH, MS3, Susan A. Rowan, DDS, MS3, Anna M. Lipowska, MD2. A0265 - Clinical Course and Outcomes Following Dental Foreign Body Ingestion: Adverse Events and Need for Endoscopy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Rush University Medical Center, Chicago, IL; 2University of Illinois at Chicago, Chicago, IL; 3UIC College of Dentistry, Chicago, IL
Introduction: Foreign body ingestion during dental procedures is a rare complication that often requires medical evaluation and consideration for object extraction. There is scarcity of data in existing literature on patient outcomes and need for endoscopy after dental foreign body ingestion (DFBI). Given the uncommon presentation of DFBI, more information would aid gastroenterologists and hospital inpatient teams to help guide treatment plans. We aim to better define patient clinical course after DFBI and identify factors that may influence outcomes.
Methods: We conducted a retrospective review of DFBI cases at a tertiary care center between 2015 and 2021. Patients younger than 18 years old were excluded. Data was collected through electronic medical record review, including patient information, clinical course, imaging, interventions, and timeline.
Results: 25 patients were included (56% male) from a diverse cohort (40% Caucasian, 20% African American, 8% Hispanic) and mean age of 64 (SD14.8). 1 patient had an ASA of ≥ 3. 3 individuals were symptomatic, foreign body sensation being most common. Most patients underwent imaging (n=24,96%), with all undergoing x-rays (100%), and 3 CT scans (12.5%). All objects were past the esophagus at time of evaluation and all patients were evaluated within 48hrs of ingestion. Gastroenterology was consulted for 9 (36%) patients and 8 (32%) were admitted to the hospital. 4 patients underwent endoscopy (16%) with object removal in 3 (12%); 0 required surgery. Endoscopy was associated with an increased likelihood of admission (p=0.047). Descriptive data was available on 19 DFB objects; the mean length was 13mm, 9 were sharp, and object sharpness was not found to be associated with requiring endoscopy (p=0.413) (Table 1). Both the complication and mortality rate of DFBI was 0% and all patients managed conservatively did well.
Discussion: This study examines a rare cohort of patients who experienced DFBI and provides better understanding of their clinical course to help guide care decisions. Our findings highlight that DFBI has mostly a benign clinical course and can likely be managed conservatively if the object is distal to the esophagus. While a number of DFBs are sharp, even those that were not retrieved passed uneventfully and without complications, likely due to their small size. No specific patient/object characteristics were associated with need for hospital admission, endoscopy, or increased rate of adverse events.
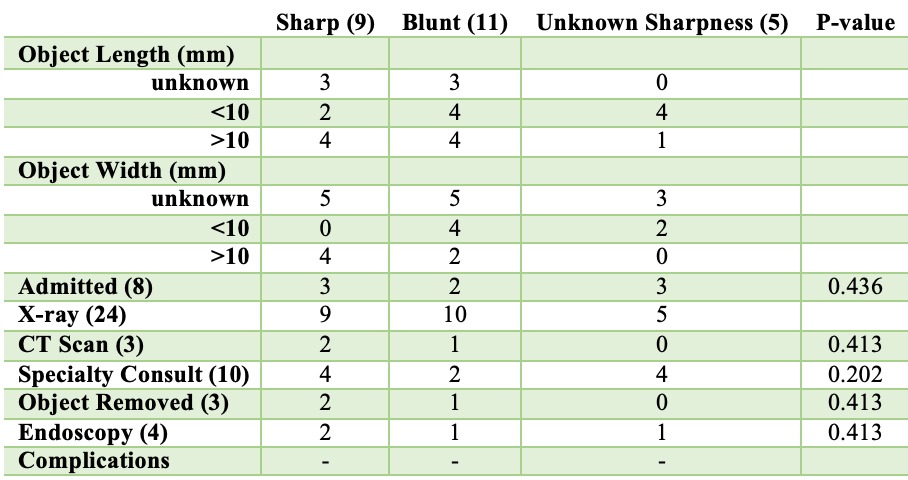
Figure: Table 1. Clinical course of DFBI based on object sharpness.
Disclosures:
Lucía Rivera Matos indicated no relevant financial relationships.
Mohammad El-Saied indicated no relevant financial relationships.
Georgia Lymberopoulos indicated no relevant financial relationships.
Jennifer Bereckis indicated no relevant financial relationships.
Susan Rowan indicated no relevant financial relationships.
Anna Lipowska indicated no relevant financial relationships.
Lucía Rivera Matos, MD1, Mohammad El-Saied, MD2, Georgia Lymberopoulos, DMD, MPH3, Jennifer Bereckis, RDH, MS3, Susan A. Rowan, DDS, MS3, Anna M. Lipowska, MD2. A0265 - Clinical Course and Outcomes Following Dental Foreign Body Ingestion: Adverse Events and Need for Endoscopy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
