Back

Poster Session A - Sunday Afternoon
Category: IBD
A0362 - Anti-TNFs Are Associated With Lower Prevalence of Cerebrovascular Disease in Patients With Inflammatory Bowel Disease
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio
.jpg)
Khaled Alsabbagh Alchirazi, MD
Cleveland Clinic
Cleveland, OH
Presenting Author(s)
Khaled Alsabbagh Alchirazi, MD1, Abdul Mohammed, MD1, Almaza A. Albakri, MD2, Ashraf Almomani, MD3, Motasem Alkhayyat, MD3, Miguel Regueiro, MD4
1Cleveland Clinic, Cleveland, OH; 2Royal Jordanian Medical Services, Amman, Al Karak, Jordan; 3Cleveland Clinic Foundation, Cleveland, OH; 4Cleveland Clinic Main Campus, Cleveland, OH
Introduction: Inflammatory bowel disease (IBD) patients are at increased risk of cerebrovascular accident (CVA) due to persistent systemic inflammation and hypercoagulability. In rheumatoid arthritis, the anti-inflammatory effects of anti-tumor necrosis factor (anti-TNF) medications are reported to improve atherosclerotic disease burden. Our study describes the effect of anti-TNF therapy on the prevalence of CVA in IBD patients.
Methods: We used a multi-institutional database (Explorys Inc, Cleveland, OH) which includes electronic health record data from 26 major integrated US healthcare systems. Based on Systematized Nomenclature of Medicine – Clinical Terms (SNOMED-CT), we identified all patients (age >18 years) with a concomitant diagnosis of IBD (either Crohn’s disease or Ulcerative colitis) and CVA between 1999 to present. The study population was divided into two groups based on the use or lack of use of anti-TNFs. The intervention group was further categorized into infliximab- and adalimumab- users. A univariate binary logistic model was constructed using anti-TNF as the dependent variable.
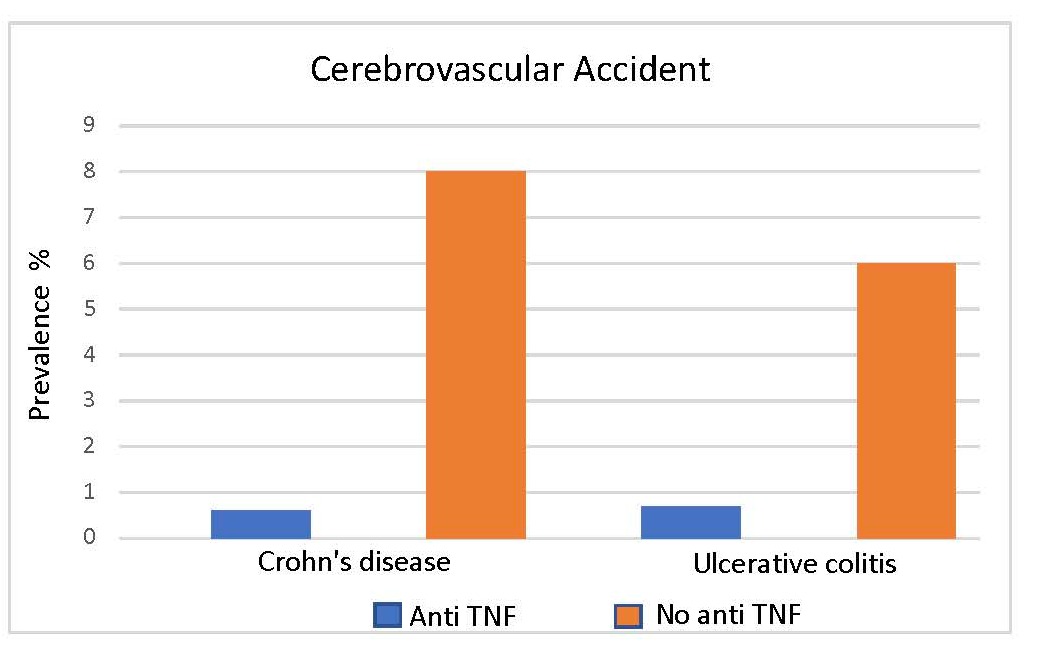
Results: Of the 70, 301,380 individuals in the database, we identified 249,300 (0.35%) patients with CD and 208,880 (0.30%) patients with UC, of whom 40,840 (16.4%) and 20,200 (10%) patients received anti-TNFs, respectively. The prevalence of CVA was 7% and 6% for CD and UC, respectively, compared to 0.3% in individuals without IBD (p< 0.0001). The prevalence of CVA was significantly lower in anti-TNF treated CD patients (0.6%) compared to those who did not receive anti-TNF (8%). Similarly, anti-TNF-treated UC patients were significantly less likely to have CVA (0.7%) compared to UC patients who did not receive anti-TNF therapy (6%) (p< 0.0001).
Discussion: In our large cohort of IBD patients, anti-TNF medications appear to be associated with a decreased prevalence of CVA. Further prospective studies are needed to determine the pathophysiology of ant-TNF medications in improving atherosclerotic disease burden in IBD patients.
Disclosures:
Khaled Alsabbagh Alchirazi, MD1, Abdul Mohammed, MD1, Almaza A. Albakri, MD2, Ashraf Almomani, MD3, Motasem Alkhayyat, MD3, Miguel Regueiro, MD4. A0362 - Anti-TNFs Are Associated With Lower Prevalence of Cerebrovascular Disease in Patients With Inflammatory Bowel Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Cleveland Clinic, Cleveland, OH; 2Royal Jordanian Medical Services, Amman, Al Karak, Jordan; 3Cleveland Clinic Foundation, Cleveland, OH; 4Cleveland Clinic Main Campus, Cleveland, OH
Introduction: Inflammatory bowel disease (IBD) patients are at increased risk of cerebrovascular accident (CVA) due to persistent systemic inflammation and hypercoagulability. In rheumatoid arthritis, the anti-inflammatory effects of anti-tumor necrosis factor (anti-TNF) medications are reported to improve atherosclerotic disease burden. Our study describes the effect of anti-TNF therapy on the prevalence of CVA in IBD patients.
Methods: We used a multi-institutional database (Explorys Inc, Cleveland, OH) which includes electronic health record data from 26 major integrated US healthcare systems. Based on Systematized Nomenclature of Medicine – Clinical Terms (SNOMED-CT), we identified all patients (age >18 years) with a concomitant diagnosis of IBD (either Crohn’s disease or Ulcerative colitis) and CVA between 1999 to present. The study population was divided into two groups based on the use or lack of use of anti-TNFs. The intervention group was further categorized into infliximab- and adalimumab- users. A univariate binary logistic model was constructed using anti-TNF as the dependent variable.
Results: Of the 70, 301,380 individuals in the database, we identified 249,300 (0.35%) patients with CD and 208,880 (0.30%) patients with UC, of whom 40,840 (16.4%) and 20,200 (10%) patients received anti-TNFs, respectively. The prevalence of CVA was 7% and 6% for CD and UC, respectively, compared to 0.3% in individuals without IBD (p< 0.0001). The prevalence of CVA was significantly lower in anti-TNF treated CD patients (0.6%) compared to those who did not receive anti-TNF (8%). Similarly, anti-TNF-treated UC patients were significantly less likely to have CVA (0.7%) compared to UC patients who did not receive anti-TNF therapy (6%) (p< 0.0001).
Discussion: In our large cohort of IBD patients, anti-TNF medications appear to be associated with a decreased prevalence of CVA. Further prospective studies are needed to determine the pathophysiology of ant-TNF medications in improving atherosclerotic disease burden in IBD patients.
Figure: Figure 1: The prevalence of Cerebrovascular Accident in patients with Inflammatory Bowel Disease with and without anti-TNF therapy.
CVA; cerebrovascular accident. Anti-TNF; Anti-tumor necrosis factor.
CVA; cerebrovascular accident. Anti-TNF; Anti-tumor necrosis factor.
Anti-TNF therapy | CVA | |
Crohn's Disease, 240 (%) | Ulcerative colitis, 140 (%) | |
Infliximab | 100 (42%) | 70 (50%) |
Adalimumab | 80 (33%) | 40 (29%) |
Table: Table 1: Anti-TNF characteristics of inflammatory bowel disease individuals with Cerebrovascular Accident. CVA; Cerebrovascular accident. Anti-TNF; Anti-tumor necrosis factor.
Disclosures:
Khaled Alsabbagh Alchirazi indicated no relevant financial relationships.
Abdul Mohammed indicated no relevant financial relationships.
Almaza Albakri indicated no relevant financial relationships.
Ashraf Almomani indicated no relevant financial relationships.
Motasem Alkhayyat indicated no relevant financial relationships.
Miguel Regueiro: Abbvie – Advisory Committee/Board Member, Consultant. Abbvie – Grant/Research Support. ALFASIGMA, S.p.A. – Advisory Committee/Board Member. Allergan – Advisory Committee/Board Member. Amgen – Advisory Committee/Board Member. BMS – Grant/Research Support. Bristol Meyer Squibb – Advisory Committee/Board Member, Consultant. CC360 – Royalties. Celgene – Advisory Committee/Board Member. CME Outfitters – CME Companies. Cornerstones – CME Companies. Crohn’s and Colitis Foundation as Editor-in-Chief – Royalties. Genentech – Advisory Committee/Board Member. Genentech – Grant/Research Support. Gilead – Advisory Committee/Board Member. Gilead – Grant/Research Support. HMPGlobal – CME Companies. Imedex, GI Health Foundation (GiHF) – CME Companies. Janssen – Advisory Committee/Board Member, Consultant. Janssen – Grant/Research Support. Lilly – Grant/Research Support. MDEducation – CME Companies. Medscape – CME Companies. Miraca Labs – Advisory Committee/Board Member. MJH life sciences – CME Companies. Pfizer – Advisory Committee/Board Member, Consultant. Prometheus – Advisory Committee/Board Member. Remedy – CME Companies. Salix – Advisory Committee/Board Member. Seres – Advisory Committee/Board Member. Takeda – Advisory Committee/Board Member, Consultant. TARGET Pharma Solutions – Advisory Committee/Board Member. UCB – Grant/Research Support. WebMD – CME Companies. Wolters Kluwer Health as Author/Editor of UpToDate – Royalties.
Khaled Alsabbagh Alchirazi, MD1, Abdul Mohammed, MD1, Almaza A. Albakri, MD2, Ashraf Almomani, MD3, Motasem Alkhayyat, MD3, Miguel Regueiro, MD4. A0362 - Anti-TNFs Are Associated With Lower Prevalence of Cerebrovascular Disease in Patients With Inflammatory Bowel Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
