Back

Poster Session A - Sunday Afternoon
Category: IBD
A0351 - Monitoring in Post-Operative Crohn’s Disease: Describing Approaches and the Impact of Guidelines
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio
.jpg)
Terry Li, MD
NYU Langone Health
New York, NY
Presenting Author(s)
Terry Li, MD1, Benjamin Click, MD2, Salam Bachour, MD3, Michael Sachs, PhD4, Jordan Axelrad, MD, MPH5
1NYU Langone Health, New York, NY; 2University of Colorado Anschutz Medical Campus, Aurora, CO; 3Brigham and Women's Hospital, Boston, MA; 4Karolinska Institutet, Solna, Stockholms Lan, Sweden; 5NYU Grossman School of Medicine, New York, NY
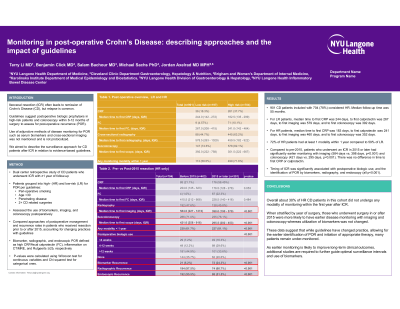
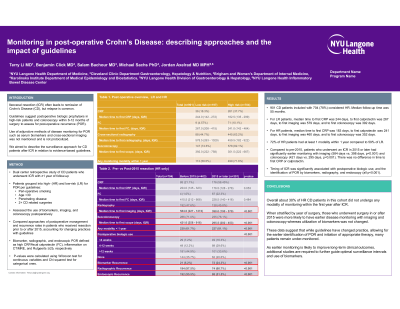
Introduction: Ileocecal resection (ICR) often leads to remission of Crohn’s Disease (CD), but relapse is common. Guidelines suggest postoperative biologic prophylaxis in high-risk patients and colonoscopy within 6-12 months of surgery to assess for post-operative recurrence (POR). Guidance on adjunctive disease monitoring modalities such as biomarkers and cross-sectional imaging is lacking. We aimed to describe the real-world surveillance approach for CD patients after ICR in relation to evidence-based guidelines.
Methods: This was a dual center retrospective study of CD patients who underwent ICR with ≥1 year of follow-up. We grouped patients into high- (HR) and low-risk (LR) for POR per guidelines and assessed the use of biomarkers, imaging, and colonoscopy postoperatively. Approaches and recurrence rates in patients who received resection prior to or after 2015, accounting for changing practices with guidelines, were compared. Biomarker, radiographic, and endoscopic POR were defined as high CRP/fecal calprotectin (FC), active inflammation on CT/MRE, and modified Rutgeerts ≥i2b, respectively. P-values were calculated using Wilcoxon and Chi squared tests.
Results: Of 1026 CD patients who underwent ICR, 798 were HR. For LR patients, median time to first CRP was 244 days (d), FC was 267d, imaging was 579d, and colonoscopy was 392d. For HR patients, median time to first CRP was 183d, FC was 241d, imaging was 460d, and colonoscopy was 352d. 72% of HR patients had at least 1 modality within 1 year compared to 59% of LR. Compared to pre-2015, patients who underwent an ICR in 2015 or later had significantly earlier imaging (543d vs. 379d, p< 0.001) and colonoscopy (404d vs. 292d, p< 0.001). There was no difference in time to first CRP or FC. Timing of ICR was significantly associated with postoperative biologic use and the detection of POR by all methods (p< 0.001).
Discussion: 30% of HR CD patients did not undergo any monitoring within the first year after ICR. Evolving practice patterns suggest earlier disease monitoring with imaging and colonoscopy in more recent years whereas utilization of biomarkers was not changed. These data suggest that while guidelines have changed practice, allowing for the earlier identification of POR and initiation of therapy, many patients remain under-monitored. As earlier monitoring may improve long-term clinical outcomes, additional studies are required to further guide optimal surveillance intervals and use of biomarkers.
Disclosures:
Terry Li, MD1, Benjamin Click, MD2, Salam Bachour, MD3, Michael Sachs, PhD4, Jordan Axelrad, MD, MPH5. A0351 - Monitoring in Post-Operative Crohn’s Disease: Describing Approaches and the Impact of Guidelines, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1NYU Langone Health, New York, NY; 2University of Colorado Anschutz Medical Campus, Aurora, CO; 3Brigham and Women's Hospital, Boston, MA; 4Karolinska Institutet, Solna, Stockholms Lan, Sweden; 5NYU Grossman School of Medicine, New York, NY
Introduction: Ileocecal resection (ICR) often leads to remission of Crohn’s Disease (CD), but relapse is common. Guidelines suggest postoperative biologic prophylaxis in high-risk patients and colonoscopy within 6-12 months of surgery to assess for post-operative recurrence (POR). Guidance on adjunctive disease monitoring modalities such as biomarkers and cross-sectional imaging is lacking. We aimed to describe the real-world surveillance approach for CD patients after ICR in relation to evidence-based guidelines.
Methods: This was a dual center retrospective study of CD patients who underwent ICR with ≥1 year of follow-up. We grouped patients into high- (HR) and low-risk (LR) for POR per guidelines and assessed the use of biomarkers, imaging, and colonoscopy postoperatively. Approaches and recurrence rates in patients who received resection prior to or after 2015, accounting for changing practices with guidelines, were compared. Biomarker, radiographic, and endoscopic POR were defined as high CRP/fecal calprotectin (FC), active inflammation on CT/MRE, and modified Rutgeerts ≥i2b, respectively. P-values were calculated using Wilcoxon and Chi squared tests.
Results: Of 1026 CD patients who underwent ICR, 798 were HR. For LR patients, median time to first CRP was 244 days (d), FC was 267d, imaging was 579d, and colonoscopy was 392d. For HR patients, median time to first CRP was 183d, FC was 241d, imaging was 460d, and colonoscopy was 352d. 72% of HR patients had at least 1 modality within 1 year compared to 59% of LR. Compared to pre-2015, patients who underwent an ICR in 2015 or later had significantly earlier imaging (543d vs. 379d, p< 0.001) and colonoscopy (404d vs. 292d, p< 0.001). There was no difference in time to first CRP or FC. Timing of ICR was significantly associated with postoperative biologic use and the detection of POR by all methods (p< 0.001).
Discussion: 30% of HR CD patients did not undergo any monitoring within the first year after ICR. Evolving practice patterns suggest earlier disease monitoring with imaging and colonoscopy in more recent years whereas utilization of biomarkers was not changed. These data suggest that while guidelines have changed practice, allowing for the earlier identification of POR and initiation of therapy, many patients remain under-monitored. As earlier monitoring may improve long-term clinical outcomes, additional studies are required to further guide optimal surveillance intervals and use of biomarkers.
Disclosures:
Terry Li indicated no relevant financial relationships.
Benjamin Click: Jannsen – Consultant. Takeda – Consultant.
Salam Bachour indicated no relevant financial relationships.
Michael Sachs indicated no relevant financial relationships.
Jordan Axelrad: AbbVie – Consultant. BioFire Diagnostics – Consultant, Grant/Research Support. BMS – Consultant. Janssen – Consultant. Pfizer – Consultant.
Terry Li, MD1, Benjamin Click, MD2, Salam Bachour, MD3, Michael Sachs, PhD4, Jordan Axelrad, MD, MPH5. A0351 - Monitoring in Post-Operative Crohn’s Disease: Describing Approaches and the Impact of Guidelines, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
