Back

Poster Session A - Sunday Afternoon
Category: Esophagus
A0239 - Esophageal Squamous Cell Carcinoma: An Unfavorable Complication of Achalasia
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio
Harsh Patel, MD, MPH
NewYork Presbyterian Brooklyn Methodist Hospital
Brooklyn, NY
Presenting Author(s)
Harsh Patel, MD, MPH1, Dean Rizzi, MD2, Navim Mobin, MD1, Michael Castillo, MD3, Vincent Notar-Francesco, MD1
1NewYork Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY; 2New York Presbyterian Brooklyn Methodist, Brooklyn, NY; 3New York Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY
Introduction: Achalasia is a motility disorder of the esophagus characterized by impaired relaxation of the lower esophageal sphincter and loss of peristalsis in the distal esophagus. It is a rare condition with an annual incidence of 0.5-1.2 per 100,000 individuals. The etiology of primary achalasia is unknown, however secondary achalasia can be attributed to malignancy, infections or systemic diseases such as amyloidosis. An infrequent complication of achalasia is esophageal squamous cell carcinoma which has a prevalence of 26 in every 1,000 cases. We present a case of interval locoregionally advanced esophageal squamous cell carcinoma only two years after a normal upper endoscopy.
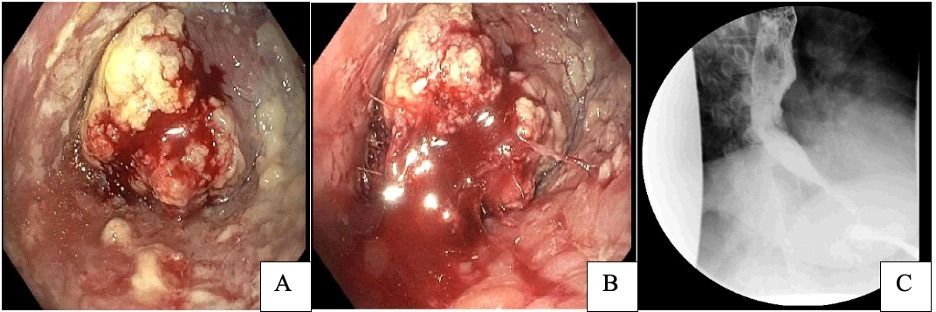
Case Description/Methods: A 67-year-old female with known achalasia and previous pneumatic dilation in her 30s presented to our outpatient clinic in 2019 with complaints of worsening chronic dysphagia. EGD was performed which revealed a significantly dilated esophagus with candida esophagitis. Despite completing antifungal therapy, she continued to experience dysphagia to solids and liquids. Barium swallow demonstrated absent peristalsis with pooling of contrast within the esophagus. High-Resolution Manometry testing demonstrated absent peristalsis. She opted for surgical myotomy, however due to COVID restrictions, the procedure was delayed. Repeat EGD was performed in 2022 for pre-surgical evaluation and showed a large obstructing friable esophageal mass in the lower third of the esophagus. Pathology was consistent with invasive poorly differentiated squamous cell carcinoma. PET scan showed locoregional disease with FDG-avid esophageal and gastrohepatic node lesions. She was started on chemoradiation with Paclitaxel and Carboplatin.
Discussion: The risk of esophageal squamous cell carcinoma in achalasia has significantly increased with incidence of approximately 1 in 300 patients. The presumed mechanism of malignancy in achalasia is poor emptying resulting in food stasis, bacterial overgrowth and inflammation leading to dysplasia and development of carcinoma. Given the relatively low incidence, there are currently no guidelines on routine endoscopic screening to assess for malignancy in patients with achalasia. Survival rates are poor as patients are often diagnosed at advanced stages. This case aims to illustrate the importance and need for interval screening in individuals with long standing achalasia to improve outcomes.
Disclosures:
Harsh Patel, MD, MPH1, Dean Rizzi, MD2, Navim Mobin, MD1, Michael Castillo, MD3, Vincent Notar-Francesco, MD1. A0239 - Esophageal Squamous Cell Carcinoma: An Unfavorable Complication of Achalasia, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1NewYork Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY; 2New York Presbyterian Brooklyn Methodist, Brooklyn, NY; 3New York Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY
Introduction: Achalasia is a motility disorder of the esophagus characterized by impaired relaxation of the lower esophageal sphincter and loss of peristalsis in the distal esophagus. It is a rare condition with an annual incidence of 0.5-1.2 per 100,000 individuals. The etiology of primary achalasia is unknown, however secondary achalasia can be attributed to malignancy, infections or systemic diseases such as amyloidosis. An infrequent complication of achalasia is esophageal squamous cell carcinoma which has a prevalence of 26 in every 1,000 cases. We present a case of interval locoregionally advanced esophageal squamous cell carcinoma only two years after a normal upper endoscopy.
Case Description/Methods: A 67-year-old female with known achalasia and previous pneumatic dilation in her 30s presented to our outpatient clinic in 2019 with complaints of worsening chronic dysphagia. EGD was performed which revealed a significantly dilated esophagus with candida esophagitis. Despite completing antifungal therapy, she continued to experience dysphagia to solids and liquids. Barium swallow demonstrated absent peristalsis with pooling of contrast within the esophagus. High-Resolution Manometry testing demonstrated absent peristalsis. She opted for surgical myotomy, however due to COVID restrictions, the procedure was delayed. Repeat EGD was performed in 2022 for pre-surgical evaluation and showed a large obstructing friable esophageal mass in the lower third of the esophagus. Pathology was consistent with invasive poorly differentiated squamous cell carcinoma. PET scan showed locoregional disease with FDG-avid esophageal and gastrohepatic node lesions. She was started on chemoradiation with Paclitaxel and Carboplatin.
Discussion: The risk of esophageal squamous cell carcinoma in achalasia has significantly increased with incidence of approximately 1 in 300 patients. The presumed mechanism of malignancy in achalasia is poor emptying resulting in food stasis, bacterial overgrowth and inflammation leading to dysplasia and development of carcinoma. Given the relatively low incidence, there are currently no guidelines on routine endoscopic screening to assess for malignancy in patients with achalasia. Survival rates are poor as patients are often diagnosed at advanced stages. This case aims to illustrate the importance and need for interval screening in individuals with long standing achalasia to improve outcomes.
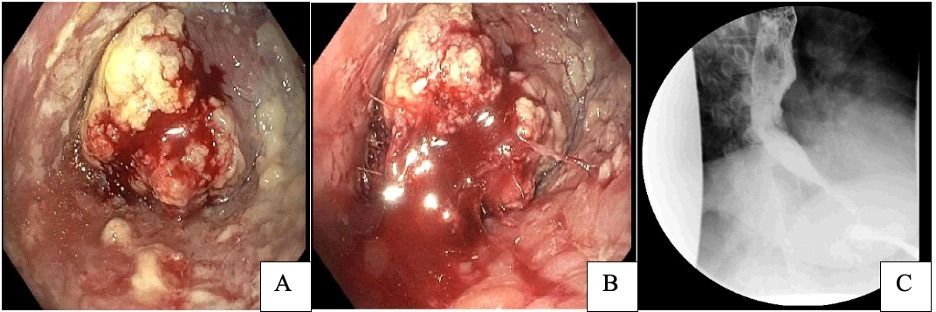
Figure: Figure 1: Image A, B demonstrating almost completely obstructing mass, with retained food products. Lesion appears friable and is oozing blood. Image C with retained contrast and “birds beak” deformity at the gastroesophageal junction.
Disclosures:
Harsh Patel indicated no relevant financial relationships.
Dean Rizzi indicated no relevant financial relationships.
Navim Mobin indicated no relevant financial relationships.
Michael Castillo indicated no relevant financial relationships.
Vincent Notar-Francesco indicated no relevant financial relationships.
Harsh Patel, MD, MPH1, Dean Rizzi, MD2, Navim Mobin, MD1, Michael Castillo, MD3, Vincent Notar-Francesco, MD1. A0239 - Esophageal Squamous Cell Carcinoma: An Unfavorable Complication of Achalasia, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
