Back

Poster Session A - Sunday Afternoon
Category: IBD
A0367 - Prevalence of Non-Hodgkin’s Lymphoma Among IBD and Celiac Disease Patients: Results From a Population-Based Study
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio
.jpg)
Khaled Alsabbagh Alchirazi, MD
Cleveland Clinic
Cleveland, OH
Presenting Author(s)
Khaled Alsabbagh Alchirazi, MD1, Abdul Mohammed, MD1, Osama Hamid, MD, MRCPI1, Ashraf Almomani, MD2, Alberto Rubio Tapia, MD1, Miguel Regueiro, MD3
1Cleveland Clinic, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland, OH; 3Cleveland Clinic Main Campus, Cleveland, OH
Introduction: There is an increased risk of non-Hodgkin’s lymphoma (NHL) in chronic inflammatory diseases like rheumatoid arthritis and celiac disease (CD). Although inflammatory bowel disease (IBD) is associated with hematologic manifestations, the association between NHL and IBD remains unclear. Using a large database, we aimed to investigate the epidemiology and risk of NHL in IBD patients.
Methods: We queried a multi-institutional database (Explorys Inc, Cleveland, OH), an aggregate of electronic health record data from 26 US healthcare systems. We identified patients diagnosed with IBD, CD, and NHL based on Systemized Nomenclature of Medicine Clinical Terms, between 1999 and the present. We assessed the prevalence of NHL in patients with IBD without CD and CD without IBD and compared it to patients without IBD or CD.
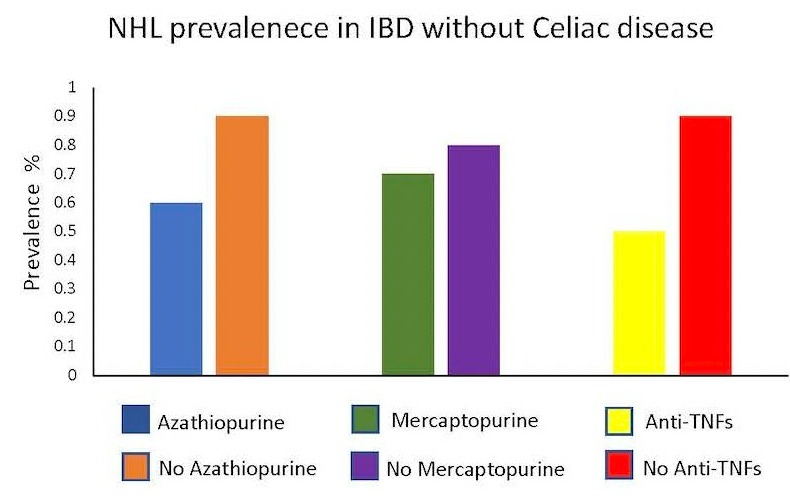
Results: Out of more than 70 million patients in the database, we identified 187,510 with NHL (0.3%), 412,950 with IBD (0.6%), and 136,690 with CD (0.2%). The prevalence of NHL was 0.7% in CD without IBD, 0.8% in IBD without CD and 0.3% among patients without CD or IBD. The risk of NHL was higher in CD without IBD [OR 3.01 95% CI: 2.82–3.21, p < 0.0001] and in IBD without CD [OR 3.22 95% CI: 3.11–3.33, p < 0.0001] than in patients with neither IBD nor CD. In the group with IBD, the risk of NHL was higher in females vs. males (51% vs 49%), in elderly vs. adults aged 18–65 (69% vs 31%) and in Caucasians vs. non-Caucasians (84% vs 16%) (table 1). IBD patients treated with anti-tumor necrosis factors (anti-TNFs) had lower rates of NHL [OR: 0.60; 95% CI: 0.53-0.68, P < 0.0001] vs IBD who were not on anti-TNFs. Similarly, azathioprine had lower rates of NHL [OR: 0.74; 95% CI: 0.64-0.86, P= 0.0001]. 6-mercaptopurine had no significant effect [OR: 0.86; 95% CI: 0.71-1.06, P= 0.1518] (figure 1).
Discussion: Utilizing a large population database, we report a distinct increased association of NHL in IBD and CD. Our findings of lower rates of NHL in immunosuppressed patients contradicts prior studies. These discrepant results could be a sampling error, but also could be that lower inflammatory states are associated with lower NHL rates. More study is needed to evaluate this.
Disclosures:
Khaled Alsabbagh Alchirazi, MD1, Abdul Mohammed, MD1, Osama Hamid, MD, MRCPI1, Ashraf Almomani, MD2, Alberto Rubio Tapia, MD1, Miguel Regueiro, MD3. A0367 - Prevalence of Non-Hodgkin’s Lymphoma Among IBD and Celiac Disease Patients: Results From a Population-Based Study, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Cleveland Clinic, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland, OH; 3Cleveland Clinic Main Campus, Cleveland, OH
Introduction: There is an increased risk of non-Hodgkin’s lymphoma (NHL) in chronic inflammatory diseases like rheumatoid arthritis and celiac disease (CD). Although inflammatory bowel disease (IBD) is associated with hematologic manifestations, the association between NHL and IBD remains unclear. Using a large database, we aimed to investigate the epidemiology and risk of NHL in IBD patients.
Methods: We queried a multi-institutional database (Explorys Inc, Cleveland, OH), an aggregate of electronic health record data from 26 US healthcare systems. We identified patients diagnosed with IBD, CD, and NHL based on Systemized Nomenclature of Medicine Clinical Terms, between 1999 and the present. We assessed the prevalence of NHL in patients with IBD without CD and CD without IBD and compared it to patients without IBD or CD.
Results: Out of more than 70 million patients in the database, we identified 187,510 with NHL (0.3%), 412,950 with IBD (0.6%), and 136,690 with CD (0.2%). The prevalence of NHL was 0.7% in CD without IBD, 0.8% in IBD without CD and 0.3% among patients without CD or IBD. The risk of NHL was higher in CD without IBD [OR 3.01 95% CI: 2.82–3.21, p < 0.0001] and in IBD without CD [OR 3.22 95% CI: 3.11–3.33, p < 0.0001] than in patients with neither IBD nor CD. In the group with IBD, the risk of NHL was higher in females vs. males (51% vs 49%), in elderly vs. adults aged 18–65 (69% vs 31%) and in Caucasians vs. non-Caucasians (84% vs 16%) (table 1). IBD patients treated with anti-tumor necrosis factors (anti-TNFs) had lower rates of NHL [OR: 0.60; 95% CI: 0.53-0.68, P < 0.0001] vs IBD who were not on anti-TNFs. Similarly, azathioprine had lower rates of NHL [OR: 0.74; 95% CI: 0.64-0.86, P= 0.0001]. 6-mercaptopurine had no significant effect [OR: 0.86; 95% CI: 0.71-1.06, P= 0.1518] (figure 1).
Discussion: Utilizing a large population database, we report a distinct increased association of NHL in IBD and CD. Our findings of lower rates of NHL in immunosuppressed patients contradicts prior studies. These discrepant results could be a sampling error, but also could be that lower inflammatory states are associated with lower NHL rates. More study is needed to evaluate this.
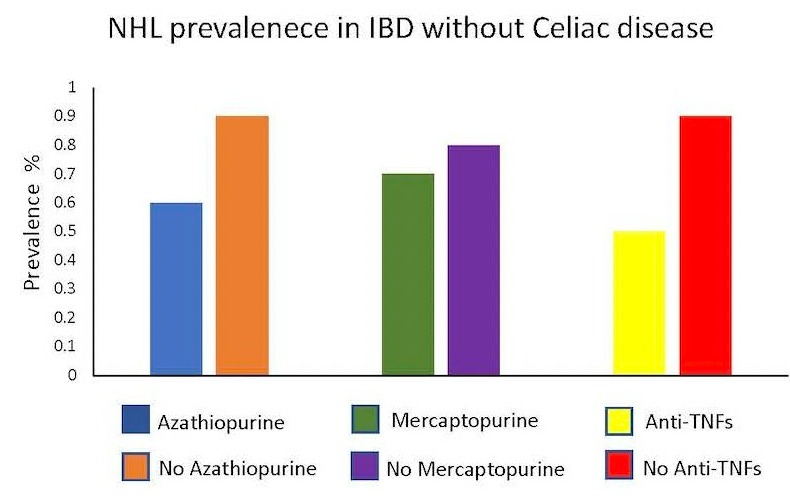
Figure: Figure 1: The prevalence of NHL in patients with inflammatory bowel disease without history of celiac disease based on medication group. IBD; inflammatory bowel disease, NHL; non-hodgkin's lymphoma.
Table: Table 1. Gender-, Age- and Race-Based Prevalence of NHL in individuals with IBD in the United States. Univariate analysis used to calculate OR. OR; odds ratio, CI; confidence interval, IBD; Inflammatory bowel disease, NHL; Non-Hodgkin's Lymphoma.
Disclosures:
Khaled Alsabbagh Alchirazi indicated no relevant financial relationships.
Abdul Mohammed indicated no relevant financial relationships.
Osama Hamid indicated no relevant financial relationships.
Ashraf Almomani indicated no relevant financial relationships.
Alberto Rubio Tapia indicated no relevant financial relationships.
Miguel Regueiro: Abbvie – Advisory Committee/Board Member, Consultant. Abbvie – Grant/Research Support. ALFASIGMA, S.p.A. – Advisory Committee/Board Member. Allergan – Advisory Committee/Board Member. Amgen – Advisory Committee/Board Member. BMS – Grant/Research Support. Bristol Meyer Squibb – Advisory Committee/Board Member, Consultant. CC360 – Royalties. Celgene – Advisory Committee/Board Member. CME Outfitters – CME Companies. Cornerstones – CME Companies. Crohn’s and Colitis Foundation as Editor-in-Chief – Royalties. Genentech – Advisory Committee/Board Member. Genentech – Grant/Research Support. Gilead – Advisory Committee/Board Member. Gilead – Grant/Research Support. HMPGlobal – CME Companies. Imedex, GI Health Foundation (GiHF) – CME Companies. Janssen – Advisory Committee/Board Member, Consultant. Janssen – Grant/Research Support. Lilly – Grant/Research Support. MDEducation – CME Companies. Medscape – CME Companies. Miraca Labs – Advisory Committee/Board Member. MJH life sciences – CME Companies. Pfizer – Advisory Committee/Board Member, Consultant. Prometheus – Advisory Committee/Board Member. Remedy – CME Companies. Salix – Advisory Committee/Board Member. Seres – Advisory Committee/Board Member. Takeda – Advisory Committee/Board Member, Consultant. TARGET Pharma Solutions – Advisory Committee/Board Member. UCB – Grant/Research Support. WebMD – CME Companies. Wolters Kluwer Health as Author/Editor of UpToDate – Royalties.
Khaled Alsabbagh Alchirazi, MD1, Abdul Mohammed, MD1, Osama Hamid, MD, MRCPI1, Ashraf Almomani, MD2, Alberto Rubio Tapia, MD1, Miguel Regueiro, MD3. A0367 - Prevalence of Non-Hodgkin’s Lymphoma Among IBD and Celiac Disease Patients: Results From a Population-Based Study, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
