Back
Poster Session A - Sunday Afternoon
Category: Liver
A0499 - Inpatient Management of Decompensated Cirrhosis - A Quality Improvement Initiative
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
- AK
Ali Khalifa, MD
Rutgers Medical School of Robert Wood Johnson - Saint Peter's University Hospital
New Brunswick, New Jersey
Presenting Author(s)
Ali Khalifa, MD1, Sotirios Doukas, MD2, Yi-Chia Wu, MD3, Chinedum Enete, MD2, Mohamed Abdelbaky, MD2, Arkady Broder, MD, FACG3
1Rutgers Medical School of Robert Wood Johnson - Saint Peter's University Hospital, New Brunswick, NJ; 2Rutgers Robert Wood Johnson Medical School/Saint Peter's University Hospital, New Brunswick, NJ; 3Rutgers Medical School of Robert Wood Johnson, Saint Peter's University Hospital, New Brunswick, NJ
Introduction: Cirrhosis management is centered on the treatment of the causes and management of the complications. The AASLD provides clear recommendations for inpatient management of cirrhosis decompensated by ascites, spontaneous bacterial peritonitis (SBP), hepatic encephalopathy (HE), and hepatorenal syndrome (HRS).
Methods: We evaluated the current hospital practice for 150 consecutively admitted patients with cirrhosis complications in the period between 2017 and 2021. Decompensated cirrhosis was identified using ICD code K70.30/K70.31 (alcoholic cirrhosis) or K74.69/K74.60 (cirrhosis without alcohol), in addition to R18.8 (ascites), plus/minus any of the following: K65.2 (SBP), K72.91 (HE), and K76.7 (HRS).
Results: 21/150 patients had no evidence of clinically decompensated cirrhosis on chart review and thus 129 patients represented the study cohort (decompensated cirrhosis, by at least ascites). The mean age of the cohort was 60±14 years. 83 patients were men, and the majority were White (88 patients, 68%). The most common cause of cirrhosis was alcohol related (72 patients, 56%), most patients had Child Pugh C (64%), and a mean MELD score of 21±7.7 and 20±7.5 on admission and discharge, respectively. Only 49/129 (38%) patients with cirrhotic ascites underwent diagnostic/therapeutic paracentesis. The second most common complication was esophageal varices (52 patients (40%)). SBP was noted in 8 patients, all of whom received appropriate medical treatment. SBP prophylaxis was indicated in 13 patients, and 10 of whom only received prophylaxis on discharge (77%). 41 patients had history of HE, and 21 of whom (51%) were on lactulose treatment. 14 patients developed HRS and were all started on albumin and octreotide therapy. 72 patients (56%) were placed on the appropriate cirrhotic diet, and daily weight was measured in 33/129 patients (26%) undergoing diuresis during the hospital stay. The mean length of stay was 5.9±4.4 days. 54 patients (42%) were re-admitted, and 13 patients (10%) died during the 90-day follow up period.
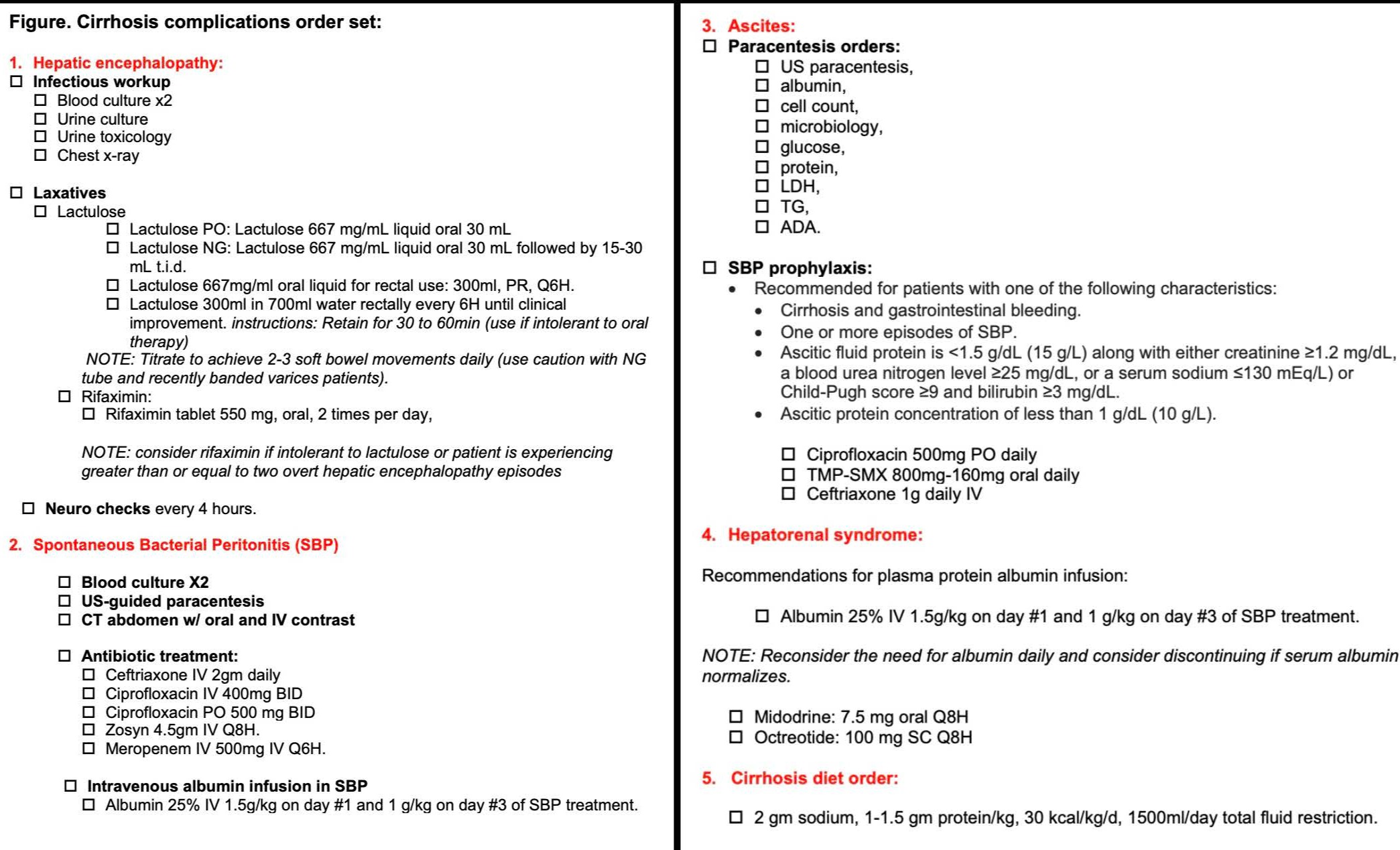
Discussion: We here demonstrated that further improvement in the medical care provided to hospitalized cirrhotic patients remains necessary. We recommend further education of the medical staff on the current guidelines to improve the care provided as well as adopting an electronic medical record order set (Figure) topromote consistent evidence-based practice, decrease errors of omission, and support provider efficiency.
Disclosures:
Ali Khalifa, MD1, Sotirios Doukas, MD2, Yi-Chia Wu, MD3, Chinedum Enete, MD2, Mohamed Abdelbaky, MD2, Arkady Broder, MD, FACG3. A0499 - Inpatient Management of Decompensated Cirrhosis - A Quality Improvement Initiative, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Rutgers Medical School of Robert Wood Johnson - Saint Peter's University Hospital, New Brunswick, NJ; 2Rutgers Robert Wood Johnson Medical School/Saint Peter's University Hospital, New Brunswick, NJ; 3Rutgers Medical School of Robert Wood Johnson, Saint Peter's University Hospital, New Brunswick, NJ
Introduction: Cirrhosis management is centered on the treatment of the causes and management of the complications. The AASLD provides clear recommendations for inpatient management of cirrhosis decompensated by ascites, spontaneous bacterial peritonitis (SBP), hepatic encephalopathy (HE), and hepatorenal syndrome (HRS).
Methods: We evaluated the current hospital practice for 150 consecutively admitted patients with cirrhosis complications in the period between 2017 and 2021. Decompensated cirrhosis was identified using ICD code K70.30/K70.31 (alcoholic cirrhosis) or K74.69/K74.60 (cirrhosis without alcohol), in addition to R18.8 (ascites), plus/minus any of the following: K65.2 (SBP), K72.91 (HE), and K76.7 (HRS).
Results: 21/150 patients had no evidence of clinically decompensated cirrhosis on chart review and thus 129 patients represented the study cohort (decompensated cirrhosis, by at least ascites). The mean age of the cohort was 60±14 years. 83 patients were men, and the majority were White (88 patients, 68%). The most common cause of cirrhosis was alcohol related (72 patients, 56%), most patients had Child Pugh C (64%), and a mean MELD score of 21±7.7 and 20±7.5 on admission and discharge, respectively. Only 49/129 (38%) patients with cirrhotic ascites underwent diagnostic/therapeutic paracentesis. The second most common complication was esophageal varices (52 patients (40%)). SBP was noted in 8 patients, all of whom received appropriate medical treatment. SBP prophylaxis was indicated in 13 patients, and 10 of whom only received prophylaxis on discharge (77%). 41 patients had history of HE, and 21 of whom (51%) were on lactulose treatment. 14 patients developed HRS and were all started on albumin and octreotide therapy. 72 patients (56%) were placed on the appropriate cirrhotic diet, and daily weight was measured in 33/129 patients (26%) undergoing diuresis during the hospital stay. The mean length of stay was 5.9±4.4 days. 54 patients (42%) were re-admitted, and 13 patients (10%) died during the 90-day follow up period.
Discussion: We here demonstrated that further improvement in the medical care provided to hospitalized cirrhotic patients remains necessary. We recommend further education of the medical staff on the current guidelines to improve the care provided as well as adopting an electronic medical record order set (Figure) topromote consistent evidence-based practice, decrease errors of omission, and support provider efficiency.
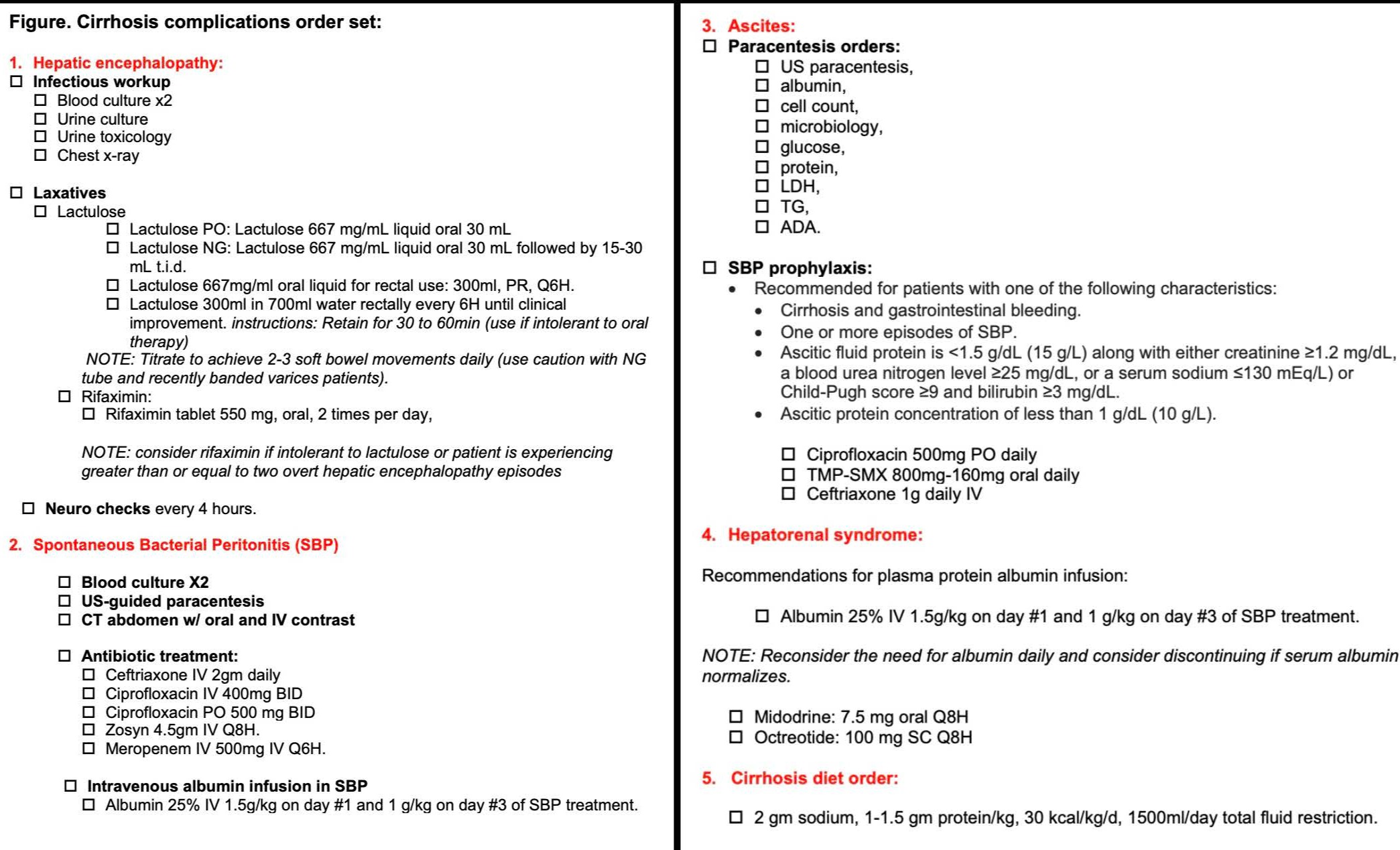
Figure: Figure. Cirrhosis complications order set:
Disclosures:
Ali Khalifa indicated no relevant financial relationships.
Sotirios Doukas indicated no relevant financial relationships.
Yi-Chia Wu indicated no relevant financial relationships.
Chinedum Enete indicated no relevant financial relationships.
Mohamed Abdelbaky indicated no relevant financial relationships.
Arkady Broder: GITrak – Advisory Committee/Board Member.
Ali Khalifa, MD1, Sotirios Doukas, MD2, Yi-Chia Wu, MD3, Chinedum Enete, MD2, Mohamed Abdelbaky, MD2, Arkady Broder, MD, FACG3. A0499 - Inpatient Management of Decompensated Cirrhosis - A Quality Improvement Initiative, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
