Back

Poster Session A - Sunday Afternoon
Category: Biliary/Pancreas
A0003 - Antibiotics Use in Acute Pancreatitis: An Ongoing Problem
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Spyridon Zouridis, MD
Albany Medical Center
Albany, NY
Presenting Author(s)
Spyridon Zouridis, MD, Daniel Sofia, MD, Sonia Samuel, DO, Omar Merdan, MD, Paul J. Feuster, PhD, Omar Tageldin, MD, Stephen Hasak, MD, MPH
Albany Medical Center, Albany, NY
Introduction: Antibiotics use in acute pancreatitis remains a controversial practice. Antibiotic use in acute pancreatitis is indicated in cases of infected pancreatic necrosis, ideally after a culture is obtained. In clinical practice however, antibiotic use is common even in cases without obvious or documented infection.
Methods: This retrospective cohort study included adult patients diagnosed with acute pancreatitis in our hospital between 01/2016- 12/2019. Pancreatitis was confirmed by using the revised Atlanta criteria. Antibiotic use, pancreatitis type (IEP: Idiopathic Edematous pancreatitis or NP: Necrotizing Pancreatitis), etiology, concerns for pancreatic or extra-pancreatic infection and length of stay (LoS) were also collected. Statistical analysis performed by Minitab.
Results: 810 patients were included. 727 (90%) and 83 (10%) had IEP and NP respectively. The most common etiologies were alcohol (25%) and gallstones (28%). 324 (40%) patients received antibiotics. When cases with extra-pancreatic infection concerns were excluded, antibiotics were used in 25% of patients. When cases with any infection concerns were excluded, the antibiotic utilization rate was 19%.
NP cases were more likely to receive antibiotics. When patients with any infection concerns were excluded, the administration rate was 62% while in IEP cases was 17%(p< 0.001).
Some etiologies were more likely to get antibiotics. Antibiotics were used in 50% of ERCP-induced pancreatitis and 39% of gallstone-induced pancreatitis.
NP cases had a significant LoS increase relative to IEP of 5.5 days. An LoS increase of 3 and 6 days was noted with extra-pancreatic and pancreatic infection concerns respectively. The etiology did not affect LoS.
The median LoS, with no antibiotic use was 4 days while with antibiotic use, was 6 days. The LoS was significantly shorter in those who received no antibiotics, even when cases with infection concerns were excluded. (Table 1)
Discussion: Despite clear guidelines, antibiotics are inappropriately used in acute pancreatitis management. Our study indicated antibiotic use in up to 40% of acute pancreatitis cases, while in 19% no clear indication was observed. Antibiotic use was much more common in NP cases. LoS was significantly longer when antibiotics were used, even when no infection suspected. To improve this problem, an acute pancreatitis order set will be included in our hospital’s electronic health records and the antibiotic utilization rate will be reassessed.
Disclosures:
Spyridon Zouridis, MD, Daniel Sofia, MD, Sonia Samuel, DO, Omar Merdan, MD, Paul J. Feuster, PhD, Omar Tageldin, MD, Stephen Hasak, MD, MPH. A0003 - Antibiotics Use in Acute Pancreatitis: An Ongoing Problem, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Albany Medical Center, Albany, NY
Introduction: Antibiotics use in acute pancreatitis remains a controversial practice. Antibiotic use in acute pancreatitis is indicated in cases of infected pancreatic necrosis, ideally after a culture is obtained. In clinical practice however, antibiotic use is common even in cases without obvious or documented infection.
Methods: This retrospective cohort study included adult patients diagnosed with acute pancreatitis in our hospital between 01/2016- 12/2019. Pancreatitis was confirmed by using the revised Atlanta criteria. Antibiotic use, pancreatitis type (IEP: Idiopathic Edematous pancreatitis or NP: Necrotizing Pancreatitis), etiology, concerns for pancreatic or extra-pancreatic infection and length of stay (LoS) were also collected. Statistical analysis performed by Minitab.
Results: 810 patients were included. 727 (90%) and 83 (10%) had IEP and NP respectively. The most common etiologies were alcohol (25%) and gallstones (28%). 324 (40%) patients received antibiotics. When cases with extra-pancreatic infection concerns were excluded, antibiotics were used in 25% of patients. When cases with any infection concerns were excluded, the antibiotic utilization rate was 19%.
NP cases were more likely to receive antibiotics. When patients with any infection concerns were excluded, the administration rate was 62% while in IEP cases was 17%(p< 0.001).
Some etiologies were more likely to get antibiotics. Antibiotics were used in 50% of ERCP-induced pancreatitis and 39% of gallstone-induced pancreatitis.
NP cases had a significant LoS increase relative to IEP of 5.5 days. An LoS increase of 3 and 6 days was noted with extra-pancreatic and pancreatic infection concerns respectively. The etiology did not affect LoS.
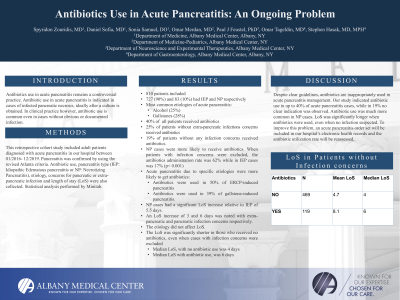
The median LoS, with no antibiotic use was 4 days while with antibiotic use, was 6 days. The LoS was significantly shorter in those who received no antibiotics, even when cases with infection concerns were excluded. (Table 1)
Discussion: Despite clear guidelines, antibiotics are inappropriately used in acute pancreatitis management. Our study indicated antibiotic use in up to 40% of acute pancreatitis cases, while in 19% no clear indication was observed. Antibiotic use was much more common in NP cases. LoS was significantly longer when antibiotics were used, even when no infection suspected. To improve this problem, an acute pancreatitis order set will be included in our hospital’s electronic health records and the antibiotic utilization rate will be reassessed.
Antibiotics | N | Mean LoS | Median LoS |
NO | 469 | 4.7 | 4 |
YES | 119 | 8.1 | 6 |
Table: Table 1: Antibiotics & Length of stay in days (LoS) in patients without infection concerns
Disclosures:
Spyridon Zouridis indicated no relevant financial relationships.
Daniel Sofia indicated no relevant financial relationships.
Sonia Samuel indicated no relevant financial relationships.
Omar Merdan indicated no relevant financial relationships.
Paul Feuster indicated no relevant financial relationships.
Omar Tageldin indicated no relevant financial relationships.
Stephen Hasak indicated no relevant financial relationships.
Spyridon Zouridis, MD, Daniel Sofia, MD, Sonia Samuel, DO, Omar Merdan, MD, Paul J. Feuster, PhD, Omar Tageldin, MD, Stephen Hasak, MD, MPH. A0003 - Antibiotics Use in Acute Pancreatitis: An Ongoing Problem, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
