Back

Poster Session A - Sunday Afternoon
Category: Practice Management
A0633 - Optimizing the GI Consult Process: Jointly Bridging the Gap
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Sean Lee, MD
University of Arizona
Tucson, AZ
Presenting Author(s)
Sean Lee, MD, Fortune Unegbu, MD, Cameron Thompson, MD
University of Arizona, Tucson, AZ
Introduction: Many training programs may lack formal teaching regarding proper consults and lead to inefficiency, particularly with heavily utilized services like gastroenterology.
In this study, we focus on bridging the gap and improving communication during the consult process between internal medicine residents and gastroenterology fellows in a teaching hospital.
Methods: We asked residents their training level, formal teaching, and comfort level in calling consults. We asked fellows the average number of consults, “unclear” consults, and those more appropriate for a different service. Working with a chief GI fellow, medicine residents jointly developed a primer of most common questions to aid in framing the question, work-up, and management. After 1 month of dissemination, respondents were re-polled. Responses were anonymous and analyzed via paired, two-tailed t-tests.
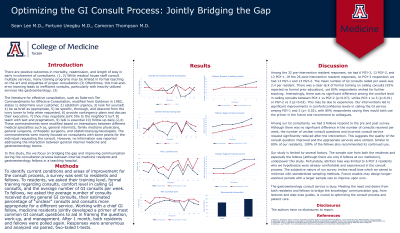
Results: Of the 32 pre-intervention residents, we had 6 PGY-3, 13 PGY-2, and 13 PGY-1. Of the 26 post-intervention residents, no PGY-3 responded. 93% of residents reported no prior training, yet 80% wished for it. There was no significant difference among the comfort level in calling consults between PGY-1 vs PGY-2 (p=0.07); unlike PGY-1 vs 3 (p< 0.01) or PGY-2 vs 3 (p=0.03). This may be due to experience. Our interventions led to significant improvements in confidence levels in calling the GI service among PGY-1 and 2 (p= 0.02), with 80% respondents saying they would use the primer in the future and recommend to colleagues.
5 of our institution’s 8 fellows responded to the pre and post survey. Though there was no significant difference in the number of consults received, the number of unclear questions and incorrect services significantly reduced post-intervention. Similar to 80% of our residents, 100% of the fellows recommended its continued use.
Discussion: Our study is limited by several factors. The sample size from residents and especially the fellows underpower the study. Attrition bias was limited to 6 PGY 3 residents who we hypothesize were experienced with consults. The subjective nature of our survey invites recall bias which we minimized with standardized sampling. Future studies may design longer-washout periods with a larger sample size.
The gastroenterology consult service is busy. Meeting the need and desire from both residents and fellows to bridge the knowledge/ communication gap, is crucial to optimizing the consult process and patient care.

Disclosures:
Sean Lee, MD, Fortune Unegbu, MD, Cameron Thompson, MD. A0633 - Optimizing the GI Consult Process: Jointly Bridging the Gap, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
University of Arizona, Tucson, AZ
Introduction: Many training programs may lack formal teaching regarding proper consults and lead to inefficiency, particularly with heavily utilized services like gastroenterology.
In this study, we focus on bridging the gap and improving communication during the consult process between internal medicine residents and gastroenterology fellows in a teaching hospital.
Methods: We asked residents their training level, formal teaching, and comfort level in calling consults. We asked fellows the average number of consults, “unclear” consults, and those more appropriate for a different service. Working with a chief GI fellow, medicine residents jointly developed a primer of most common questions to aid in framing the question, work-up, and management. After 1 month of dissemination, respondents were re-polled. Responses were anonymous and analyzed via paired, two-tailed t-tests.
Results: Of the 32 pre-intervention residents, we had 6 PGY-3, 13 PGY-2, and 13 PGY-1. Of the 26 post-intervention residents, no PGY-3 responded. 93% of residents reported no prior training, yet 80% wished for it. There was no significant difference among the comfort level in calling consults between PGY-1 vs PGY-2 (p=0.07); unlike PGY-1 vs 3 (p< 0.01) or PGY-2 vs 3 (p=0.03). This may be due to experience. Our interventions led to significant improvements in confidence levels in calling the GI service among PGY-1 and 2 (p= 0.02), with 80% respondents saying they would use the primer in the future and recommend to colleagues.
5 of our institution’s 8 fellows responded to the pre and post survey. Though there was no significant difference in the number of consults received, the number of unclear questions and incorrect services significantly reduced post-intervention. Similar to 80% of our residents, 100% of the fellows recommended its continued use.
Discussion: Our study is limited by several factors. The sample size from residents and especially the fellows underpower the study. Attrition bias was limited to 6 PGY 3 residents who we hypothesize were experienced with consults. The subjective nature of our survey invites recall bias which we minimized with standardized sampling. Future studies may design longer-washout periods with a larger sample size.
The gastroenterology consult service is busy. Meeting the need and desire from both residents and fellows to bridge the knowledge/ communication gap, is crucial to optimizing the consult process and patient care.

Figure: PGY-1 Confidence level in calling GI consults pre vs post intervention
Disclosures:
Sean Lee indicated no relevant financial relationships.
Fortune Unegbu indicated no relevant financial relationships.
Cameron Thompson indicated no relevant financial relationships.
Sean Lee, MD, Fortune Unegbu, MD, Cameron Thompson, MD. A0633 - Optimizing the GI Consult Process: Jointly Bridging the Gap, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
