Back

Poster Session A - Sunday Afternoon
Category: Colon
A0161 - TACE-Induced Ischemic Colitis
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Jonathan E. Selzman, DO
University of Texas Health Science Center
San Antonio, TX
Presenting Author(s)
Jonathan E. Selzman, DO1, Mahesh Gajendran, MD, MPH2, Tamneet Basra, MD1, Bara El Kurdi, MD1, Randy Wright, MD3, Chandraprakash Umapathy, MD4, Juan Echavarria, MD1
1University of Texas Health Science Center , San Antonio, TX; 2UTHSCSA, San Antonio, TX; 3UT Health San Antonio, San Antonio, TX; 4University of Texas Health San Antonio, San Antonio, TX
Introduction: Transarterial chemoembolization (TACE) is a locoregional treatment used in patients with hepatocellular carcinoma (HCC). This therapy entails injecting a chemotherapeutic agent into a branch of the hepatic artery supplying blood to the tumor while cutting off blood supply through particle embolization. This procedure may be utilized in a patient who is not a candidate for surgical resection or as a bridge to liver transplantation. Here we present a case of a ischemic colitis in the setting of a recent TACE.
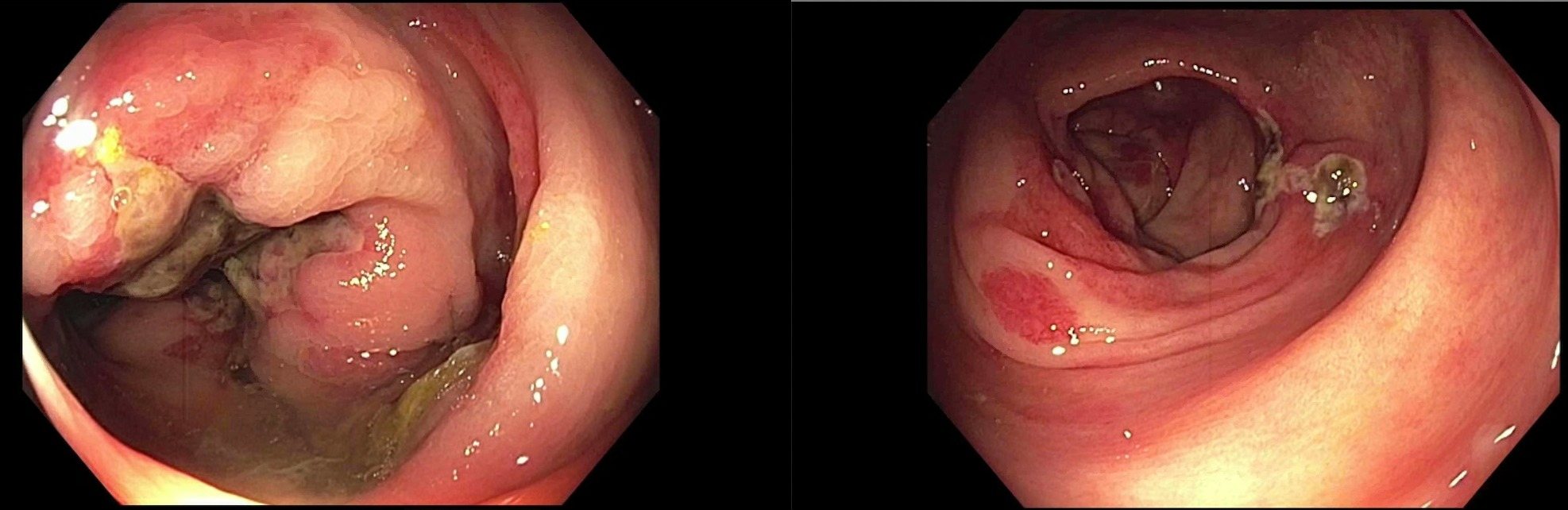
Case Description/Methods: A 65 year-old female with history of HCC underwent an outpatient TACE procedure for a 3.6 cm liver lesion. Soon after the procedure the patient complained of severe abdominal pain and was admitted. On day two of hospitalization, she developed significant bright red blood per rectum. Computed tomography (CT) demonstrated mild wall thickening and pericolonic fat stranding in the ascending colon concerning for acute colitis. Lactic acid was elevated at 5.8 mmol/L (normal < 2). Colonoscopy demonstrated multiple ulcers and erythema stretching from the cecum to descending colon suggestive of ischemic colitis. Biopsies demonstrated superficial mucosal erosion and necrosis, crypt atrophy, and lamina propria hemorrhage with hyalinization, consistent with acute ischemic colitis. CT angiography demonstrated a patent abdominal aorta and all major branches. The patient was treated conservatively without further episodes of hematochezia and was discharged home.
Discussion: Postembolization syndrome is the most common adverse effect of TACE, which occurs in 60 to 80 percent of patients. This has been reported to be related to either tumor necrosis or due to ischemic damage to normal liver parenchyma. One case of gastrointestinal ulceration has been reported after TACE. To date, there has been no reported case of ischemic colitis after TACE. This presentation of ischemic colitis in our patient may be due to regurgitation of embolized particles into superior mesenteric arterial circulation leading to hypoperfusion of the colon, resulting in ischemic colitis. One should consider this presentation on the differential diagnosis in a patient with hematochezia after TACE.
Disclosures:
Jonathan E. Selzman, DO1, Mahesh Gajendran, MD, MPH2, Tamneet Basra, MD1, Bara El Kurdi, MD1, Randy Wright, MD3, Chandraprakash Umapathy, MD4, Juan Echavarria, MD1. A0161 - TACE-Induced Ischemic Colitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Texas Health Science Center , San Antonio, TX; 2UTHSCSA, San Antonio, TX; 3UT Health San Antonio, San Antonio, TX; 4University of Texas Health San Antonio, San Antonio, TX
Introduction: Transarterial chemoembolization (TACE) is a locoregional treatment used in patients with hepatocellular carcinoma (HCC). This therapy entails injecting a chemotherapeutic agent into a branch of the hepatic artery supplying blood to the tumor while cutting off blood supply through particle embolization. This procedure may be utilized in a patient who is not a candidate for surgical resection or as a bridge to liver transplantation. Here we present a case of a ischemic colitis in the setting of a recent TACE.
Case Description/Methods: A 65 year-old female with history of HCC underwent an outpatient TACE procedure for a 3.6 cm liver lesion. Soon after the procedure the patient complained of severe abdominal pain and was admitted. On day two of hospitalization, she developed significant bright red blood per rectum. Computed tomography (CT) demonstrated mild wall thickening and pericolonic fat stranding in the ascending colon concerning for acute colitis. Lactic acid was elevated at 5.8 mmol/L (normal < 2). Colonoscopy demonstrated multiple ulcers and erythema stretching from the cecum to descending colon suggestive of ischemic colitis. Biopsies demonstrated superficial mucosal erosion and necrosis, crypt atrophy, and lamina propria hemorrhage with hyalinization, consistent with acute ischemic colitis. CT angiography demonstrated a patent abdominal aorta and all major branches. The patient was treated conservatively without further episodes of hematochezia and was discharged home.
Discussion: Postembolization syndrome is the most common adverse effect of TACE, which occurs in 60 to 80 percent of patients. This has been reported to be related to either tumor necrosis or due to ischemic damage to normal liver parenchyma. One case of gastrointestinal ulceration has been reported after TACE. To date, there has been no reported case of ischemic colitis after TACE. This presentation of ischemic colitis in our patient may be due to regurgitation of embolized particles into superior mesenteric arterial circulation leading to hypoperfusion of the colon, resulting in ischemic colitis. One should consider this presentation on the differential diagnosis in a patient with hematochezia after TACE.
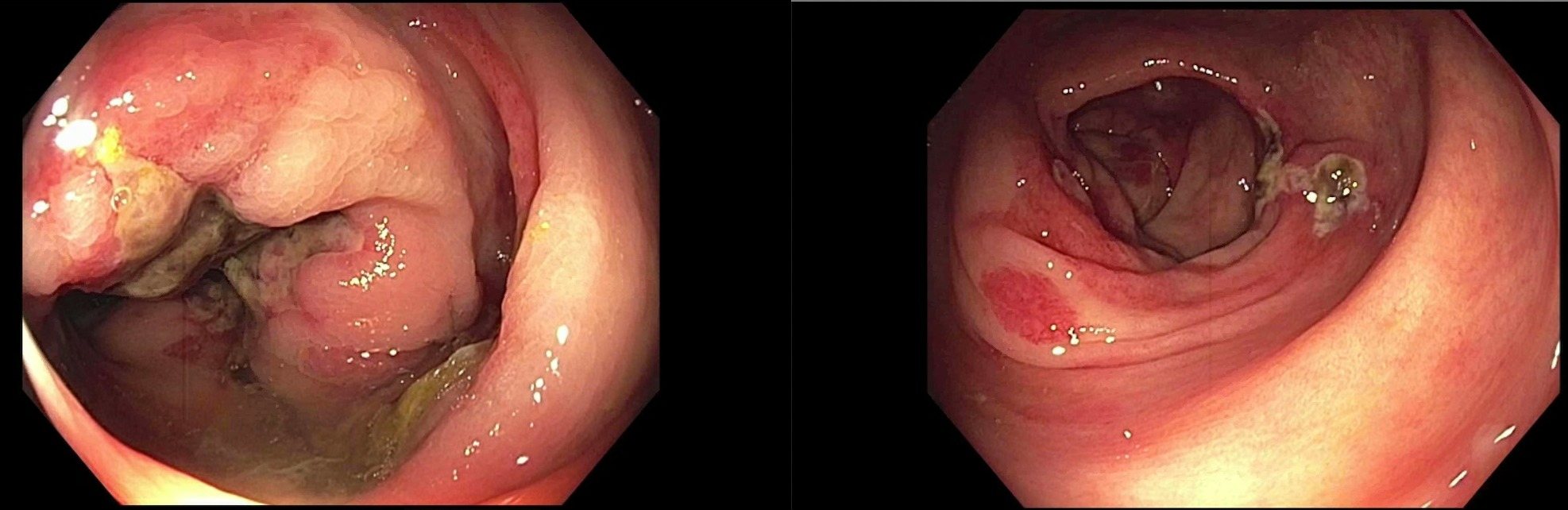
Figure: Ascending and transverse colon demonstrating multiple ulcers and erythema suggestive of ischemic colitis on colonoscopy
Disclosures:
Jonathan Selzman indicated no relevant financial relationships.
Mahesh Gajendran indicated no relevant financial relationships.
Tamneet Basra indicated no relevant financial relationships.
Bara El Kurdi indicated no relevant financial relationships.
Randy Wright indicated no relevant financial relationships.
Chandraprakash Umapathy indicated no relevant financial relationships.
Juan Echavarria indicated no relevant financial relationships.
Jonathan E. Selzman, DO1, Mahesh Gajendran, MD, MPH2, Tamneet Basra, MD1, Bara El Kurdi, MD1, Randy Wright, MD3, Chandraprakash Umapathy, MD4, Juan Echavarria, MD1. A0161 - TACE-Induced Ischemic Colitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
