Back

Poster Session A - Sunday Afternoon
Category: Small Intestine
A0642 - Device-Assisted Enteroscopy (DAE) in the Surveillance of Intestinal Polyposis in Peutz-Jeghers Syndrome
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Kent A. Broussard, MD
LSU Gastroenterology Fellowship
New Orleans, LA
Presenting Author(s)
Kent A. Broussard, MD1, Daniel Raines, MD2, Omar Wahid Mohamed Elfeky, MD3, Daniel Wild, MD4, David Cave, MD, PhD5
1LSU Gastroenterology Fellowship, New Orleans, LA; 2LSU Health Sciences Center, New Orleans, LA; 3Louisiana State University Health Sciences Center, Metairie, LA; 4Duke University Medical Center, Durham, NC; 5UMass Memorial Health, Worcester, MA
Introduction: Peutz-Jeghers Syndrome (PJS) is an autosomal dominant, genetic disorder characterized by the formation of hamartomatous polyps in the gastrointestinal tract. These polyps are a source of significant morbidity and mortality in this population due to associated complications of intestinal obstruction, bleeding, and malignant transformation. Surveillance of intestinal polyposis in patients with PJS has not been extensively studied, although centers which perform a significant volume of device-assisted enteroscopies (DAEs) encounter multiple cases each year. With the progressive adoption of DAE, examination of the deep small bowel for monitoring and prophylactic polypectomy has the potential to prevent complications of PJS and minimize the need for repeated laparotomy.
Methods: After obtaining IRB approval, electronic health records were used to identify all DAEs performed on patients with PJS at three U.S. referral centers (LSU, Duke, and UMass) between January 1st 2007 and January 1st 2020. Electronic medical records were reviewed to collect and analyze multiple data points. Primary endpoints included the complications associated with DAE performed for removal of intestinal hamartomas and the rate of laparotomy in PJS patients prior to and after index DAE. Secondary data points included patient characteristics, procedural details, and size/location/distribution of small bowel hamartomas.
Results: Twenty-four patients met our inclusion criteria. Of these, 18 (75%) had previously undergone small bowel surgery for complications related to small bowel hamartomas. Between 2007 - 2020, a total of 46 DAEs were performed in these patients with an average of one surveillance exam every 2.5 years. A total of 131 polypectomies were performed during our study period with an observed complication rate of 1.5%, including one bowel perforation requiring surgery. Only one patient underwent surgery related to small bowel hamartomas following initial DAE surveillance exam over a total of 366 years of aggregated follow-up.
Discussion: Endoscopic management of small bowel polyps in patients with PJS using DAE is an effective strategy for prophylactic removal of hamartomas. DAE surveillance and endoscopic polypectomy is safe and may decrease the need for repeated laparotomy due to complications from intestinal hamartomas in patients with PJS.

Disclosures:
Kent A. Broussard, MD1, Daniel Raines, MD2, Omar Wahid Mohamed Elfeky, MD3, Daniel Wild, MD4, David Cave, MD, PhD5. A0642 - Device-Assisted Enteroscopy (DAE) in the Surveillance of Intestinal Polyposis in Peutz-Jeghers Syndrome, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1LSU Gastroenterology Fellowship, New Orleans, LA; 2LSU Health Sciences Center, New Orleans, LA; 3Louisiana State University Health Sciences Center, Metairie, LA; 4Duke University Medical Center, Durham, NC; 5UMass Memorial Health, Worcester, MA
Introduction: Peutz-Jeghers Syndrome (PJS) is an autosomal dominant, genetic disorder characterized by the formation of hamartomatous polyps in the gastrointestinal tract. These polyps are a source of significant morbidity and mortality in this population due to associated complications of intestinal obstruction, bleeding, and malignant transformation. Surveillance of intestinal polyposis in patients with PJS has not been extensively studied, although centers which perform a significant volume of device-assisted enteroscopies (DAEs) encounter multiple cases each year. With the progressive adoption of DAE, examination of the deep small bowel for monitoring and prophylactic polypectomy has the potential to prevent complications of PJS and minimize the need for repeated laparotomy.
Methods: After obtaining IRB approval, electronic health records were used to identify all DAEs performed on patients with PJS at three U.S. referral centers (LSU, Duke, and UMass) between January 1st 2007 and January 1st 2020. Electronic medical records were reviewed to collect and analyze multiple data points. Primary endpoints included the complications associated with DAE performed for removal of intestinal hamartomas and the rate of laparotomy in PJS patients prior to and after index DAE. Secondary data points included patient characteristics, procedural details, and size/location/distribution of small bowel hamartomas.
Results: Twenty-four patients met our inclusion criteria. Of these, 18 (75%) had previously undergone small bowel surgery for complications related to small bowel hamartomas. Between 2007 - 2020, a total of 46 DAEs were performed in these patients with an average of one surveillance exam every 2.5 years. A total of 131 polypectomies were performed during our study period with an observed complication rate of 1.5%, including one bowel perforation requiring surgery. Only one patient underwent surgery related to small bowel hamartomas following initial DAE surveillance exam over a total of 366 years of aggregated follow-up.
Discussion: Endoscopic management of small bowel polyps in patients with PJS using DAE is an effective strategy for prophylactic removal of hamartomas. DAE surveillance and endoscopic polypectomy is safe and may decrease the need for repeated laparotomy due to complications from intestinal hamartomas in patients with PJS.

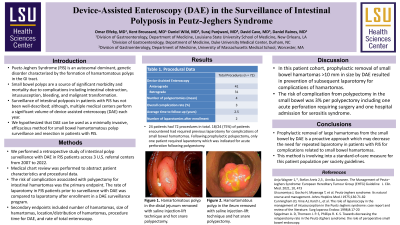
Figure: Hamartomatous polyp in the ileum removed with saline injection-lift technique and hot snare polypectomy.
Disclosures:
Kent Broussard indicated no relevant financial relationships.
Daniel Raines indicated no relevant financial relationships.
Omar Wahid Mohamed Elfeky indicated no relevant financial relationships.
Daniel Wild indicated no relevant financial relationships.
David Cave: Medtronic – Grant/Research Support. Olympus Corp of America – Grant/Research Support.
Kent A. Broussard, MD1, Daniel Raines, MD2, Omar Wahid Mohamed Elfeky, MD3, Daniel Wild, MD4, David Cave, MD, PhD5. A0642 - Device-Assisted Enteroscopy (DAE) in the Surveillance of Intestinal Polyposis in Peutz-Jeghers Syndrome, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
