Back

Poster Session A - Sunday Afternoon
Category: Small Intestine
A0662 - A Challenging Case of Eosinophilic Gastroenteritis!
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio
- AE
Abbinaya Elangovan, MD
University Hospitals Cleveland Medical Center/ Case Western Reserve University
Cleveland, OH
Presenting Author(s)
Abbinaya Elangovan, MD1, Dawn Zacharias, MD2, Fady G. Haddad, MD3
1University Hospitals Cleveland Medical Center/ Case Western Reserve University, Cleveland, OH; 2University Hospitals Cleveland Medical Center, Cleveland, OH; 3University Hospitals Cleveland Medical Center, Parma, OH
Introduction: Eosinophilic gastroenteritis (EGE) is an uncommon infiltrative eosinophilic disease. It is part of the spectrum of eosinophilic gastrointestinal disorders that also comprises eosinophilic esophagitis and eosinophilic colitis. Despite that EGE is described in the literature, its infrequent occurrence, unclear pathophysiology, and nonspecific symptoms result in substantial cases of missed and delayed diagnosis. Thus we report the case of a middle-aged woman who got diagnosed with EGE 15 years after the onset of her symptoms.
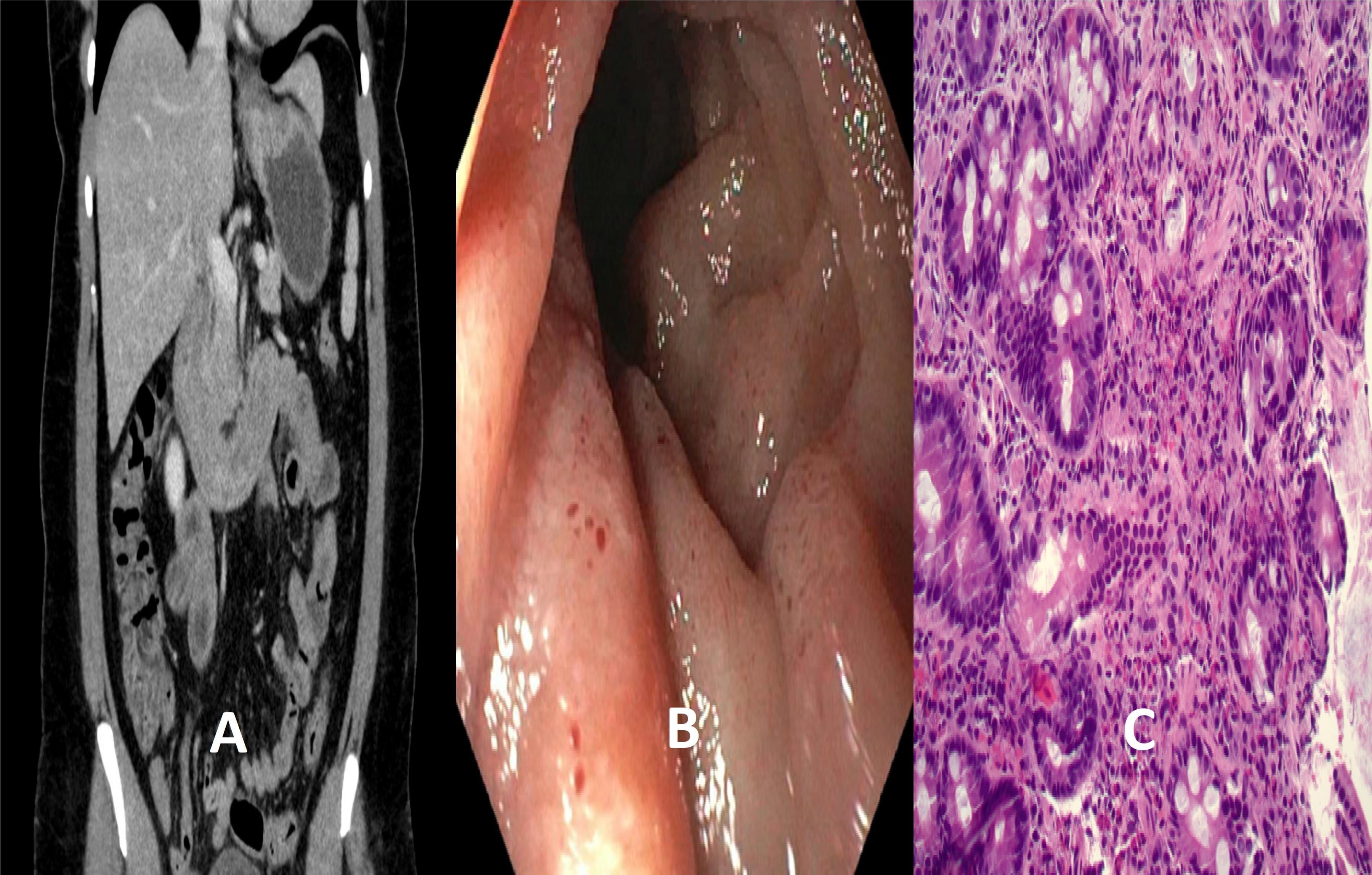
Case Description/Methods: A 43-year-old woman with a history of hypertension presented with worsening epigastric pain and postprandial vomiting for the last few weeks. She reports similar yearly episodes starting 15 years ago resolving spontaneously after a few weeks. Medications consisted of lisinopril and felodipine. Physical examination revealed epigastric tenderness. Lab tests showed a normal WBC of 8.4 (x109/L) with elevated eosinophil (Eo) count of 3.21 (x109/L) [normal range 0.00-0.70 (x109/L)] and high IgE level of 320 IU/mL [normal range 0-214 IU/mL]. Liver and kidney tests, blood smear, HIV serology, B12, tryptase levels, stool examination for ova and parasites were unrevealing. Abdominal CT scan showed wall thickening of the stomach and small intestine (panel A). Upper endoscopy showed erythema and nodularity of the gastric and duodenal mucosa (panel B). Biopsies showed 40 Eo/HPF in the gastric mucosa and 100 Eo/HPF in the duodenal mucosa suggestive of EGE (panel C). Colonoscopy and colon biopsies were unremarkable. Prednisone 40 mg daily was started with noted rapid resolution of symptoms within a few days of therapy. The patient was discharged home with a prednisone taper over 8 weeks.
Discussion: EGE is a rare disorder with less than 300 reported cases. A personal or family history of atopy is frequently described. Pathogenesis is speculated to be related to a hypersensitivity response with eosinophilic infiltration of the bowel wall. Symptoms are nonspecific. Diagnosis relies on the presence of > 20 Eo/HPF on histopathological inspection of gastric and duodenal biopsies and exclusion of other pathologies potentially associated with bowel wall eosinophilia. Despite that spontaneous remission can be seen, the majority of patients require treatment. Current available therapeutic choices include dietary modifications and pharmacological options that mainly involve corticosteroids. Recurrence of symptoms is commonly reported requiring long-term treatment.
Disclosures:
Abbinaya Elangovan, MD1, Dawn Zacharias, MD2, Fady G. Haddad, MD3. A0662 - A Challenging Case of Eosinophilic Gastroenteritis!, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University Hospitals Cleveland Medical Center/ Case Western Reserve University, Cleveland, OH; 2University Hospitals Cleveland Medical Center, Cleveland, OH; 3University Hospitals Cleveland Medical Center, Parma, OH
Introduction: Eosinophilic gastroenteritis (EGE) is an uncommon infiltrative eosinophilic disease. It is part of the spectrum of eosinophilic gastrointestinal disorders that also comprises eosinophilic esophagitis and eosinophilic colitis. Despite that EGE is described in the literature, its infrequent occurrence, unclear pathophysiology, and nonspecific symptoms result in substantial cases of missed and delayed diagnosis. Thus we report the case of a middle-aged woman who got diagnosed with EGE 15 years after the onset of her symptoms.
Case Description/Methods: A 43-year-old woman with a history of hypertension presented with worsening epigastric pain and postprandial vomiting for the last few weeks. She reports similar yearly episodes starting 15 years ago resolving spontaneously after a few weeks. Medications consisted of lisinopril and felodipine. Physical examination revealed epigastric tenderness. Lab tests showed a normal WBC of 8.4 (x109/L) with elevated eosinophil (Eo) count of 3.21 (x109/L) [normal range 0.00-0.70 (x109/L)] and high IgE level of 320 IU/mL [normal range 0-214 IU/mL]. Liver and kidney tests, blood smear, HIV serology, B12, tryptase levels, stool examination for ova and parasites were unrevealing. Abdominal CT scan showed wall thickening of the stomach and small intestine (panel A). Upper endoscopy showed erythema and nodularity of the gastric and duodenal mucosa (panel B). Biopsies showed 40 Eo/HPF in the gastric mucosa and 100 Eo/HPF in the duodenal mucosa suggestive of EGE (panel C). Colonoscopy and colon biopsies were unremarkable. Prednisone 40 mg daily was started with noted rapid resolution of symptoms within a few days of therapy. The patient was discharged home with a prednisone taper over 8 weeks.
Discussion: EGE is a rare disorder with less than 300 reported cases. A personal or family history of atopy is frequently described. Pathogenesis is speculated to be related to a hypersensitivity response with eosinophilic infiltration of the bowel wall. Symptoms are nonspecific. Diagnosis relies on the presence of > 20 Eo/HPF on histopathological inspection of gastric and duodenal biopsies and exclusion of other pathologies potentially associated with bowel wall eosinophilia. Despite that spontaneous remission can be seen, the majority of patients require treatment. Current available therapeutic choices include dietary modifications and pharmacological options that mainly involve corticosteroids. Recurrence of symptoms is commonly reported requiring long-term treatment.
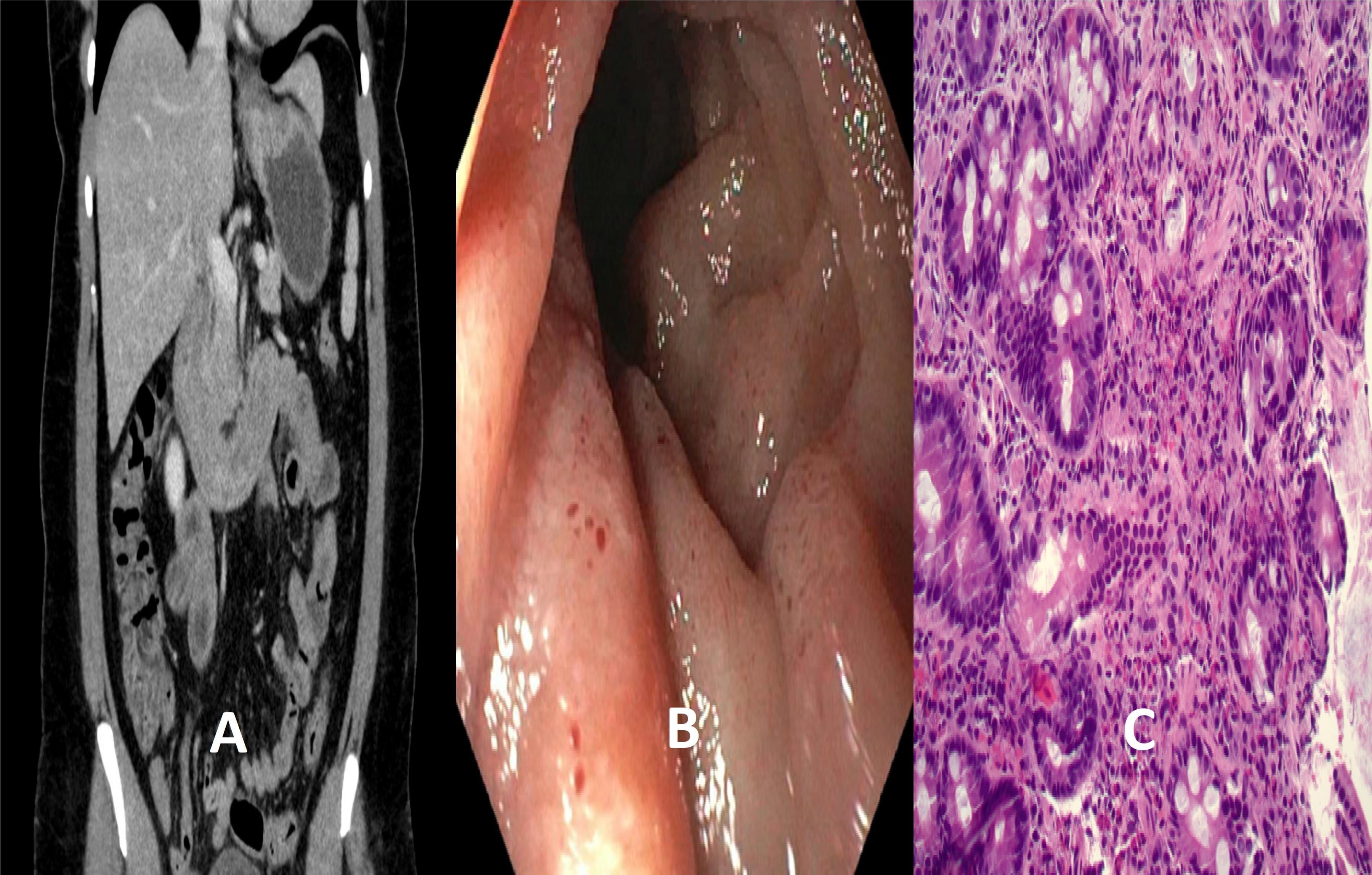
Figure: Panel A - CT Abdomen and pelvis showing wall thickening of stomach and small intestine
Panel B - Upper endoscopy showing erythema and nodularity of the gastric and duodenal mucosa
Panel C- Biopsy of the duodenal mucosa showing up to 100 eosinophils per high power field (Hematoxylin and eosin, original magnification 20 x)
Panel B - Upper endoscopy showing erythema and nodularity of the gastric and duodenal mucosa
Panel C- Biopsy of the duodenal mucosa showing up to 100 eosinophils per high power field (Hematoxylin and eosin, original magnification 20 x)
Disclosures:
Abbinaya Elangovan indicated no relevant financial relationships.
Dawn Zacharias indicated no relevant financial relationships.
Fady G. Haddad indicated no relevant financial relationships.
Abbinaya Elangovan, MD1, Dawn Zacharias, MD2, Fady G. Haddad, MD3. A0662 - A Challenging Case of Eosinophilic Gastroenteritis!, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
