Back

Poster Session A - Sunday Afternoon
Category: Small Intestine
A0664 - Olmesartan-Induced Enteritis: When Symptoms Do Not Improve With Drug Discontinuation
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Lindsey Jones, MD
Mather Hospital, Northwell Health
Port Jefferson, NY
Presenting Author(s)
Lindsey Jones, MD, Pratik Patel, MD, Vishal Rana, MD, Menatallah Algohary, MD
Mather Hospital, Northwell Health, Port Jefferson, NY
Introduction: Severe diarrhea is a well-known, but rare, complication of Olmesartan. The enteropathy caused by Olmesartan is histologically similar to Celiac disease, however celiac serologies are negative and it lacks a response to a gluten free diet. In most cases, symptoms resolve with the discontinuation of the medication. We present a case of Olmesartan induced enteropathy that only improved after the initiation of budesonide.
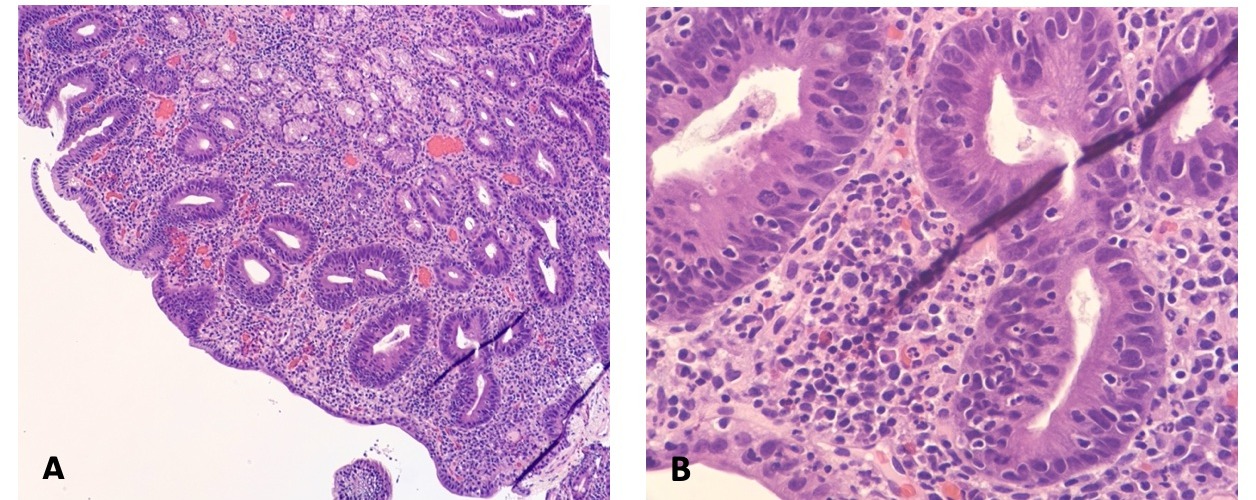
Case Description/Methods: A 73-year-old female with a history of hypertension presented with complaints of nausea, vomiting and watery diarrhea. Initial workup with bloodwork, stool studies and imaging were all unremarkable. Recent outpatient colonoscopy was unremarkable. Review of her medications did not reveal any typical culprits of microscopic colitis. Given persistent nausea and vomiting, an upper endoscopy was pursued. Celiac serologic testing, including issue transglutaminase (tTg) IgA and IgG, anti-gliadin IgA and anti-endomysial IgA antibodies were all normal. Qualitative IgA levels were within normal limits. Upper endoscopy was performed with duodenal biopsies revealing moderate active chronic duodenitis with blunting of villous architecture and increased intraepithelial lymphocytic infiltrate, suspicious for celiac sprue. At this point, a closer review of her medications revealed a prescription for Olmesartan. Olmesartan was discontinued, however she continued to have significant diarrhea, up to 2.5L daily, for over a week after discontinuation. Given persistent diarrhea, nausea and vomiting, resulting in significant electrolyte abnormalities, the decision was made to initiate Budesonide. She experienced rapid improvement in symptoms after the initiation of Budesonide and only reported two loose stools per day on discharge.
Discussion: The initial workup for chronic diarrhea involves a thorough medication review. Physicians who prescribe Olmesartan should be aware of the enteropathy it can cause, as it is likely more common than expected. Other drugs such as azathioprine, colchicine, mycophenolate, methotrexate and neomycin have also been implicated in a similar enteropathy. Timely diagnosis can help decrease healthcare utilization and patient discomfort. In cases such as ours, the enteropathy can be severe enough to result in hospital admission. Immunosuppressant’s such as steroids or azathioprine have shown great efficacy in treatment of these refractory cases.
Disclosures:
Lindsey Jones, MD, Pratik Patel, MD, Vishal Rana, MD, Menatallah Algohary, MD. A0664 - Olmesartan-Induced Enteritis: When Symptoms Do Not Improve With Drug Discontinuation, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Mather Hospital, Northwell Health, Port Jefferson, NY
Introduction: Severe diarrhea is a well-known, but rare, complication of Olmesartan. The enteropathy caused by Olmesartan is histologically similar to Celiac disease, however celiac serologies are negative and it lacks a response to a gluten free diet. In most cases, symptoms resolve with the discontinuation of the medication. We present a case of Olmesartan induced enteropathy that only improved after the initiation of budesonide.
Case Description/Methods: A 73-year-old female with a history of hypertension presented with complaints of nausea, vomiting and watery diarrhea. Initial workup with bloodwork, stool studies and imaging were all unremarkable. Recent outpatient colonoscopy was unremarkable. Review of her medications did not reveal any typical culprits of microscopic colitis. Given persistent nausea and vomiting, an upper endoscopy was pursued. Celiac serologic testing, including issue transglutaminase (tTg) IgA and IgG, anti-gliadin IgA and anti-endomysial IgA antibodies were all normal. Qualitative IgA levels were within normal limits. Upper endoscopy was performed with duodenal biopsies revealing moderate active chronic duodenitis with blunting of villous architecture and increased intraepithelial lymphocytic infiltrate, suspicious for celiac sprue. At this point, a closer review of her medications revealed a prescription for Olmesartan. Olmesartan was discontinued, however she continued to have significant diarrhea, up to 2.5L daily, for over a week after discontinuation. Given persistent diarrhea, nausea and vomiting, resulting in significant electrolyte abnormalities, the decision was made to initiate Budesonide. She experienced rapid improvement in symptoms after the initiation of Budesonide and only reported two loose stools per day on discharge.
Discussion: The initial workup for chronic diarrhea involves a thorough medication review. Physicians who prescribe Olmesartan should be aware of the enteropathy it can cause, as it is likely more common than expected. Other drugs such as azathioprine, colchicine, mycophenolate, methotrexate and neomycin have also been implicated in a similar enteropathy. Timely diagnosis can help decrease healthcare utilization and patient discomfort. In cases such as ours, the enteropathy can be severe enough to result in hospital admission. Immunosuppressant’s such as steroids or azathioprine have shown great efficacy in treatment of these refractory cases.
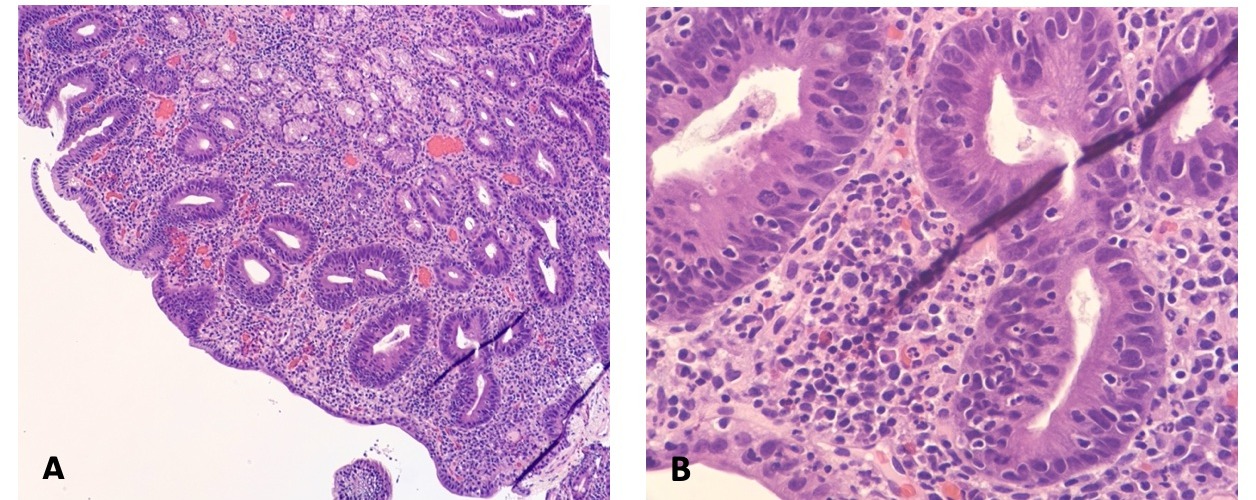
Figure: Histology of duodenal biopsy showing (A) Moderate active chronic duodenitis with blunting of villous architecture and (B) Increased intraepithelial lymphocytic infiltrate
Disclosures:
Lindsey Jones indicated no relevant financial relationships.
Pratik Patel indicated no relevant financial relationships.
Vishal Rana indicated no relevant financial relationships.
Menatallah Algohary indicated no relevant financial relationships.
Lindsey Jones, MD, Pratik Patel, MD, Vishal Rana, MD, Menatallah Algohary, MD. A0664 - Olmesartan-Induced Enteritis: When Symptoms Do Not Improve With Drug Discontinuation, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
