Back

Poster Session A - Sunday Afternoon
Category: Stomach
A0720 - Unforeseen Postoperative Complication in a Bariatric Patient: The Rare Case of a Large Phytobezoar Causing Gastric Outlet Obstruction
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Aidaliz Llorens-Bonilla, MD
University of Puerto Rico, University District Hospital, PR
Presenting Author(s)
Aidaliz Llorens-Bonilla, MD, Victor Soto-Ayala, MD, Pedro Lopez-Martinez, MD, Gretchen Marrero-Lozada, MD, Ricardo Marrero, MD, Carlos Fernandez-Sifre, MD
University of Puerto Rico, University District Hospital, San Juan, Puerto Rico
Introduction: Bariatric surgery has become increasingly popular in the treatment of obesity to achieve sustainable weight loss. Despite its numerous benefits, complications can arise due to postoperative gastric hypoacidity and motility disorders. Phytobezoars is an infrequent complication of bariatric surgery that arise from impacted aggregates of indigestible fruit and vegetables. Rarely, bezoars can cause gastric outlet obstruction and/or perforation. The following case highlights the presentation, diagnosis and treatment of phytobezoars and the importance of diet compliance in bariatric patients.
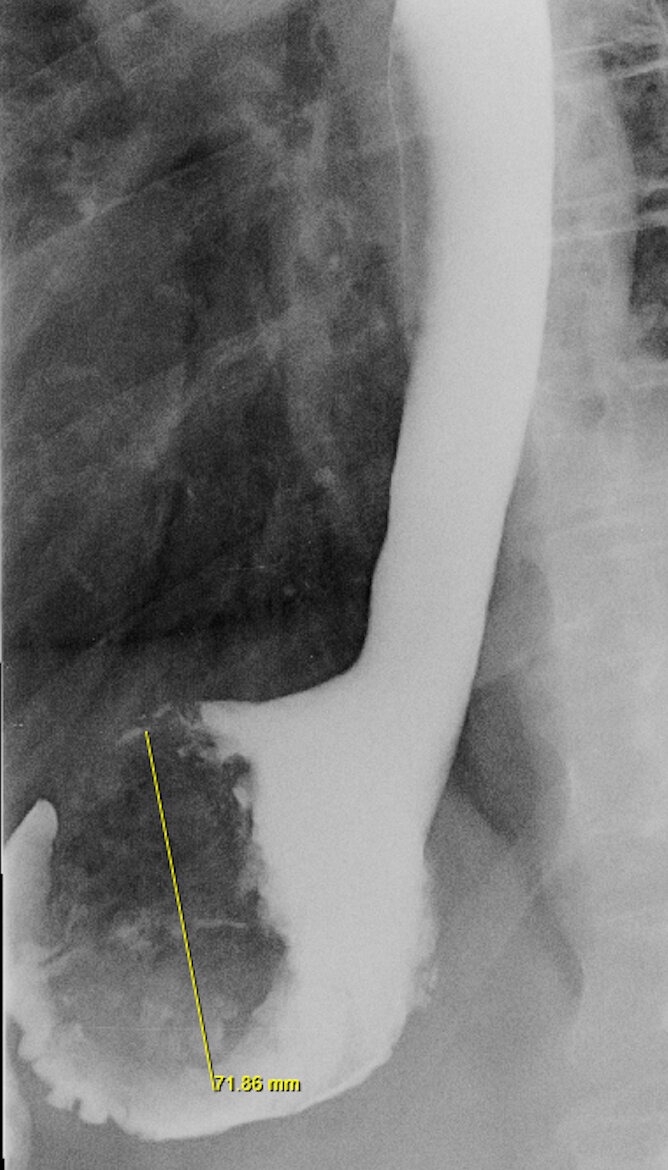
Case Description/Methods: A 60-year-old woman with hyperlipidemia was admitted due to progressive epigastric fullness and postprandial emesis of 2 weeks’ duration. Moreover, nausea was constant associated with abdominal bloating and 7-pound weight loss. Pepcid did not alleviate symptoms. She denied fever, chills, chest pain, shortness of breath, diarrhea, constipation, hematochezia nor hematemesis. Her past surgical history was pertinent for sleeve gastrectomy in 2017. She denied toxic habits. Labs were unremarkable except for isolated thrombocytopenia. Physical exam was pertinent for mild epigastric tenderness; no abdominal rigidity nor guarding present. Despite abdominopelvic CT revealing a gastric fundus dilation, an upper GI series was the study that diagnosed a large lobular filling defect compatible with a 7.2 cm phytobezoar1. Upon questioning, the patient reported that she arrived from a cruise vacation before onset of symptoms. She recalled consuming large amounts of vegetables, nuts and fruits. Initial intervention consisted of papain meat tenderizer to help dissolve bezoar. Nevertheless, symptoms persisted due to oral medication intolerance. Upper endoscopy was performed and phytobezoar was removed with Roth Net retriever. After procedure, patient was able to progressively tolerate diet and was discharge home with resolution of symptoms. Avoidance of excessive high fiber diet was recommended to prevent future bezoar formations.
Discussion: The incidence of large phytobezoars has been reported as low as 0.3% in the general population, and therefore, its identification is a diagnostic challenge. Even though most of the patients remain asymptomatic, large bezoars can cause gastric outlet obstruction that could end in perforation if not treated promptly. This case emphasizes the importance of considering phytobezoars as a cause of GI symptoms and the importance of diet education in bariatric patients.
Disclosures:
Aidaliz Llorens-Bonilla, MD, Victor Soto-Ayala, MD, Pedro Lopez-Martinez, MD, Gretchen Marrero-Lozada, MD, Ricardo Marrero, MD, Carlos Fernandez-Sifre, MD. A0720 - Unforeseen Postoperative Complication in a Bariatric Patient: The Rare Case of a Large Phytobezoar Causing Gastric Outlet Obstruction, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
University of Puerto Rico, University District Hospital, San Juan, Puerto Rico
Introduction: Bariatric surgery has become increasingly popular in the treatment of obesity to achieve sustainable weight loss. Despite its numerous benefits, complications can arise due to postoperative gastric hypoacidity and motility disorders. Phytobezoars is an infrequent complication of bariatric surgery that arise from impacted aggregates of indigestible fruit and vegetables. Rarely, bezoars can cause gastric outlet obstruction and/or perforation. The following case highlights the presentation, diagnosis and treatment of phytobezoars and the importance of diet compliance in bariatric patients.
Case Description/Methods: A 60-year-old woman with hyperlipidemia was admitted due to progressive epigastric fullness and postprandial emesis of 2 weeks’ duration. Moreover, nausea was constant associated with abdominal bloating and 7-pound weight loss. Pepcid did not alleviate symptoms. She denied fever, chills, chest pain, shortness of breath, diarrhea, constipation, hematochezia nor hematemesis. Her past surgical history was pertinent for sleeve gastrectomy in 2017. She denied toxic habits. Labs were unremarkable except for isolated thrombocytopenia. Physical exam was pertinent for mild epigastric tenderness; no abdominal rigidity nor guarding present. Despite abdominopelvic CT revealing a gastric fundus dilation, an upper GI series was the study that diagnosed a large lobular filling defect compatible with a 7.2 cm phytobezoar1. Upon questioning, the patient reported that she arrived from a cruise vacation before onset of symptoms. She recalled consuming large amounts of vegetables, nuts and fruits. Initial intervention consisted of papain meat tenderizer to help dissolve bezoar. Nevertheless, symptoms persisted due to oral medication intolerance. Upper endoscopy was performed and phytobezoar was removed with Roth Net retriever. After procedure, patient was able to progressively tolerate diet and was discharge home with resolution of symptoms. Avoidance of excessive high fiber diet was recommended to prevent future bezoar formations.
Discussion: The incidence of large phytobezoars has been reported as low as 0.3% in the general population, and therefore, its identification is a diagnostic challenge. Even though most of the patients remain asymptomatic, large bezoars can cause gastric outlet obstruction that could end in perforation if not treated promptly. This case emphasizes the importance of considering phytobezoars as a cause of GI symptoms and the importance of diet education in bariatric patients.
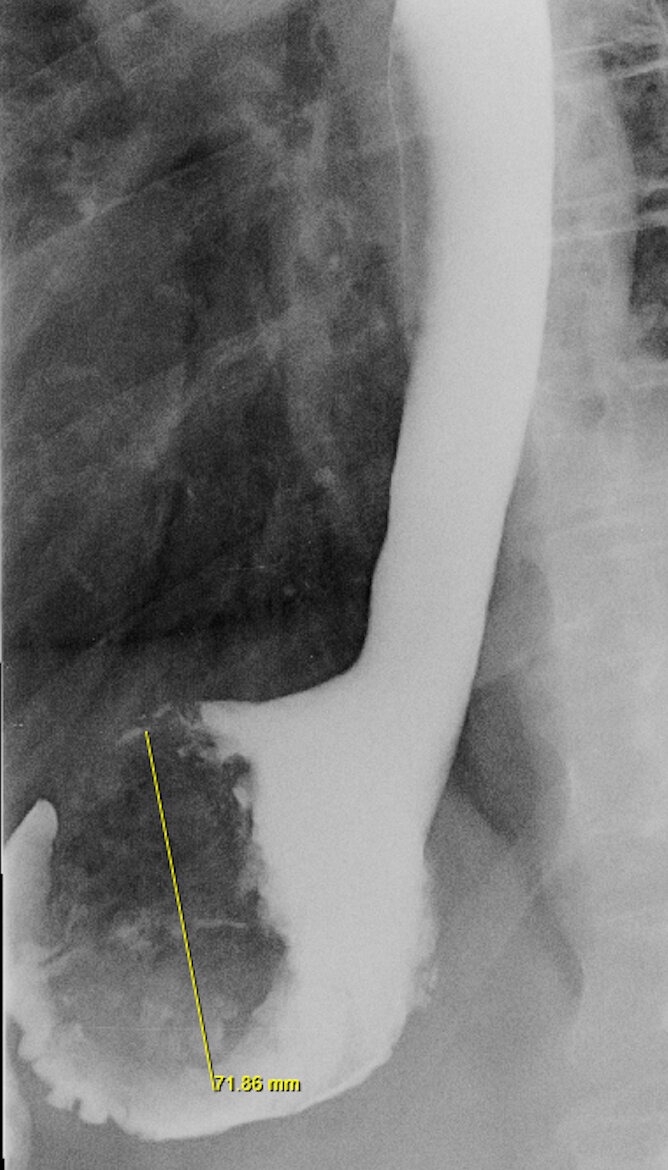
Figure: 1. Upper GI series X-ray showing a 7.2 cm phytobezoar causing a large lobular filling defect in the stomach fundus.
Disclosures:
Aidaliz Llorens-Bonilla indicated no relevant financial relationships.
Victor Soto-Ayala indicated no relevant financial relationships.
Pedro Lopez-Martinez indicated no relevant financial relationships.
Gretchen Marrero-Lozada indicated no relevant financial relationships.
Ricardo Marrero indicated no relevant financial relationships.
Carlos Fernandez-Sifre indicated no relevant financial relationships.
Aidaliz Llorens-Bonilla, MD, Victor Soto-Ayala, MD, Pedro Lopez-Martinez, MD, Gretchen Marrero-Lozada, MD, Ricardo Marrero, MD, Carlos Fernandez-Sifre, MD. A0720 - Unforeseen Postoperative Complication in a Bariatric Patient: The Rare Case of a Large Phytobezoar Causing Gastric Outlet Obstruction, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
