Back
Poster Session A - Sunday Afternoon
Category: Practice Management
A0632 - Increasing Inpatient Endoscopy Volumes Using the Model for Continuous Improvement
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom

David Hudson, MD
Western University
London, ON, Canada
Presenting Author(s)
Award: Presidential Poster Award
David Hudson, MD, Ziad Hindi, MD, Mohammed Alsager, MD, Christopher Lavalle, MD, Abdulaziz Alajmi, MD, Vadim Iablokov, MD, PhD, Jamie Gregor, MD, Nitin Khanna, MD, Brian Yan, MD, Karim Qumosani, MD, Mayur Brahmania,
Western University, London, ON, Canada
Introduction: Inpatient endoscopy volumes can affect patient care at many levels in a hospital system. At our academic center, inpatient procedural volume efficiency is 65% (defined as the number of completed procedures compared during the designated in-patient endoscopy time period). As a consequence, excess procedures are being completed on-call or on weekends. Our aim was to increase procedural volume by one (14%) additional procedure completed/day over a 12-month period.
Methods: An interprofessional team of Gastroenterology fellows and staff along with endoscopy nurses and managers was created to investigate throughput concerns. Baseline data was collected via direct observation and completion of a time study over 2 months. Subsequently, a process flow diagram was completed. A combination of root cause analysis tools (i.e. Ishikawa diagram and Pareto chart) were then utilized to identify areas for improvement. A delay in procedural start time was identified as a strong culprit for reduced efficiency. Potential PDSA (plan-do-study-act) cycles included: early physician handover start time, constructing a standardized patient procedure list, and improving timeliness of patient transfer to the endoscopy suite.
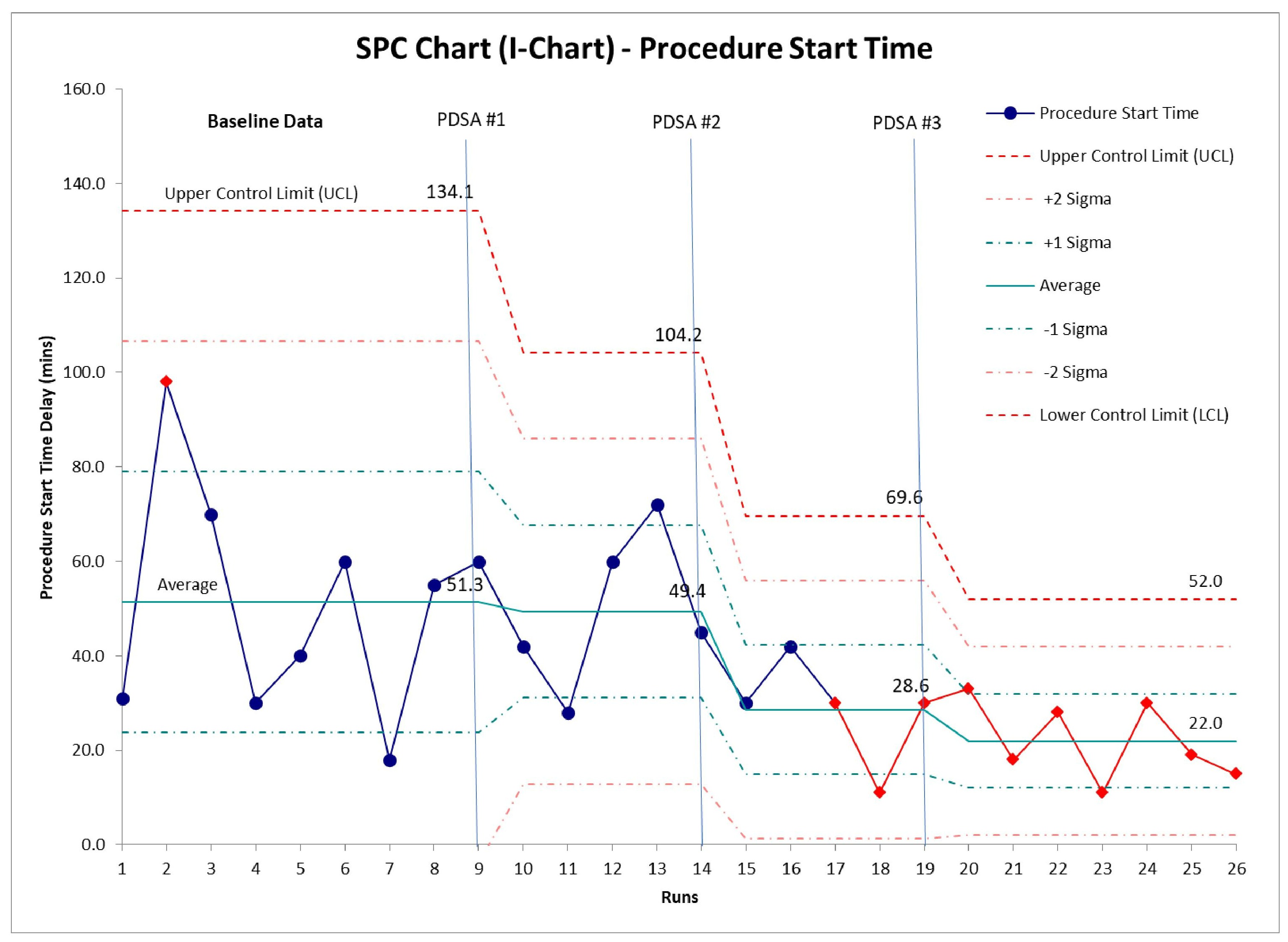
Results: Baseline data identified that the first case start time was delayed by 51 min when our actual start time is 08:00 am. Our first PDSA cycle involved a 15-minute earlier physician handover start time. PDSA cycle #1 reduced our mean procedural start time to 08:49 am [UCL: 104 minutes; LCL: -5.4 minutes]. Our second PDSA cycle, involved the standardization of a planned procedural list and mandate for the first procedure to be esophagogastroduodenoscopy (EGD). PDSA cycle #2 reduced start time reduced to 08:29 am [UCL: 69.6 minutes; LCL: -12.4 minutes]. Our third PDSA cycle, involved utilizing the standardized procedural list to pre-emptively organize timely patient transfer to account for delays secondary to hospital portering services, which reduced the mean start time further to 08:22 am [UCL: 52.0 minutes; LCL: -8.0 minutes].
Discussion: Using the model for continuous improvement we were able to increase procedural volumes by one (14%) per day. The most effective intervention included developing a standardized procedure list and mandating the first case as an EGD minimizing delays due to inadequate or incomplete bowel preparation.
Disclosures:
David Hudson, MD, Ziad Hindi, MD, Mohammed Alsager, MD, Christopher Lavalle, MD, Abdulaziz Alajmi, MD, Vadim Iablokov, MD, PhD, Jamie Gregor, MD, Nitin Khanna, MD, Brian Yan, MD, Karim Qumosani, MD, Mayur Brahmania, . A0632 - Increasing Inpatient Endoscopy Volumes Using the Model for Continuous Improvement, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
David Hudson, MD, Ziad Hindi, MD, Mohammed Alsager, MD, Christopher Lavalle, MD, Abdulaziz Alajmi, MD, Vadim Iablokov, MD, PhD, Jamie Gregor, MD, Nitin Khanna, MD, Brian Yan, MD, Karim Qumosani, MD, Mayur Brahmania,
Western University, London, ON, Canada
Introduction: Inpatient endoscopy volumes can affect patient care at many levels in a hospital system. At our academic center, inpatient procedural volume efficiency is 65% (defined as the number of completed procedures compared during the designated in-patient endoscopy time period). As a consequence, excess procedures are being completed on-call or on weekends. Our aim was to increase procedural volume by one (14%) additional procedure completed/day over a 12-month period.
Methods: An interprofessional team of Gastroenterology fellows and staff along with endoscopy nurses and managers was created to investigate throughput concerns. Baseline data was collected via direct observation and completion of a time study over 2 months. Subsequently, a process flow diagram was completed. A combination of root cause analysis tools (i.e. Ishikawa diagram and Pareto chart) were then utilized to identify areas for improvement. A delay in procedural start time was identified as a strong culprit for reduced efficiency. Potential PDSA (plan-do-study-act) cycles included: early physician handover start time, constructing a standardized patient procedure list, and improving timeliness of patient transfer to the endoscopy suite.
Results: Baseline data identified that the first case start time was delayed by 51 min when our actual start time is 08:00 am. Our first PDSA cycle involved a 15-minute earlier physician handover start time. PDSA cycle #1 reduced our mean procedural start time to 08:49 am [UCL: 104 minutes; LCL: -5.4 minutes]. Our second PDSA cycle, involved the standardization of a planned procedural list and mandate for the first procedure to be esophagogastroduodenoscopy (EGD). PDSA cycle #2 reduced start time reduced to 08:29 am [UCL: 69.6 minutes; LCL: -12.4 minutes]. Our third PDSA cycle, involved utilizing the standardized procedural list to pre-emptively organize timely patient transfer to account for delays secondary to hospital portering services, which reduced the mean start time further to 08:22 am [UCL: 52.0 minutes; LCL: -8.0 minutes].
Discussion: Using the model for continuous improvement we were able to increase procedural volumes by one (14%) per day. The most effective intervention included developing a standardized procedure list and mandating the first case as an EGD minimizing delays due to inadequate or incomplete bowel preparation.
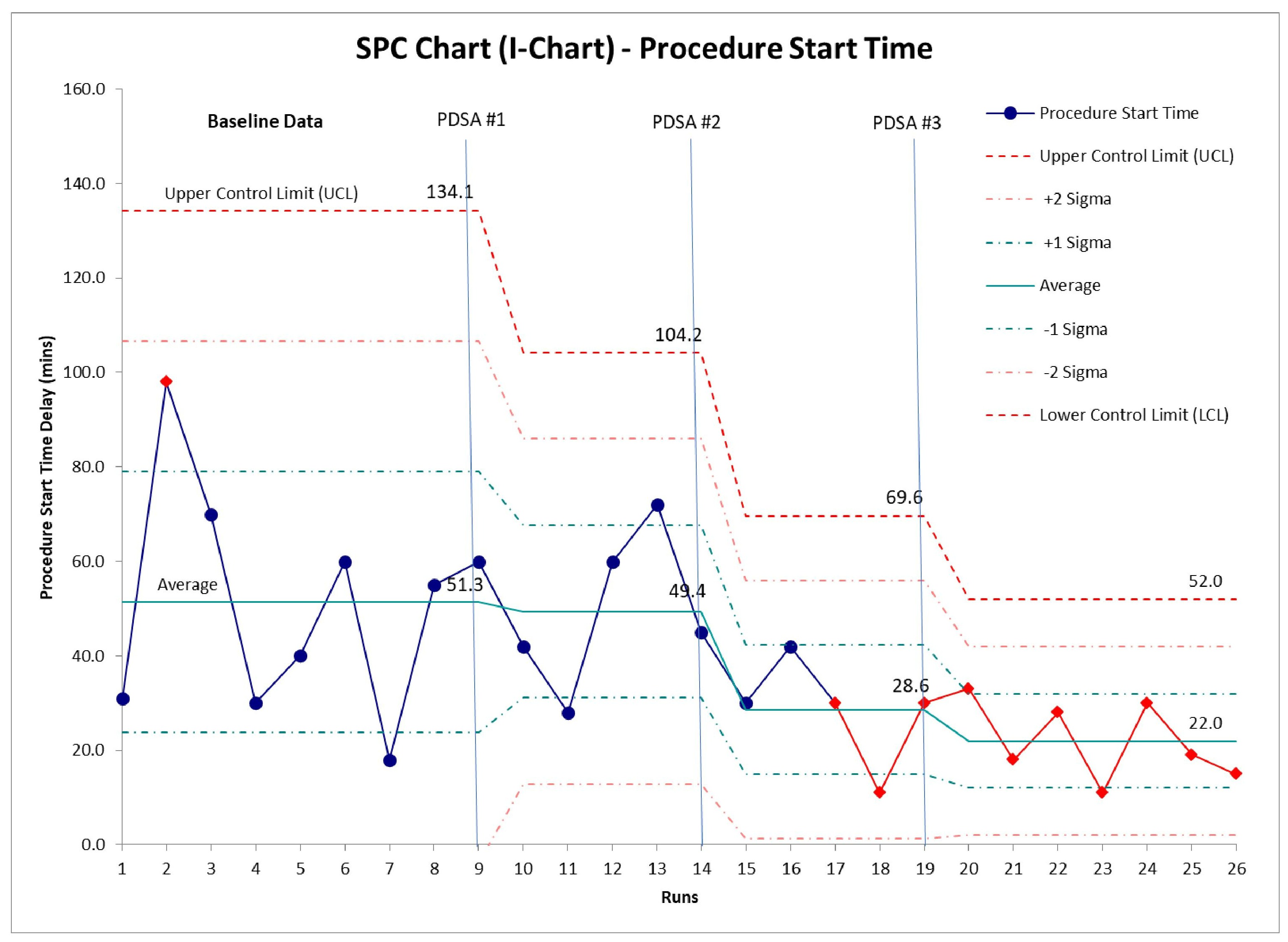
Figure: Figure 1: A statistical process control chart (SPC) demonstrating baseline data on endoscopy procedural start time and interventions (PDSA #1, PDSA#2, PDSA#3) that were effective in reducing the delay in procedure start time and resulted in a subsequent increase in endoscopy unit efficiency.
Disclosures:
David Hudson indicated no relevant financial relationships.
Ziad Hindi indicated no relevant financial relationships.
Mohammed Alsager indicated no relevant financial relationships.
Christopher Lavalle indicated no relevant financial relationships.
Abdulaziz Alajmi indicated no relevant financial relationships.
Vadim Iablokov indicated no relevant financial relationships.
Jamie Gregor: AbbVie – Advisor or Review Panel Member. Allergan – Advisor or Review Panel Member. Janssen – Advisor or Review Panel Member. Takeda – Advisor or Review Panel Member, Grant/Research Support.
Nitin Khanna indicated no relevant financial relationships.
Brian Yan indicated no relevant financial relationships.
Karim Qumosani indicated no relevant financial relationships.
Mayur Brahmania indicated no relevant financial relationships.
David Hudson, MD, Ziad Hindi, MD, Mohammed Alsager, MD, Christopher Lavalle, MD, Abdulaziz Alajmi, MD, Vadim Iablokov, MD, PhD, Jamie Gregor, MD, Nitin Khanna, MD, Brian Yan, MD, Karim Qumosani, MD, Mayur Brahmania, . A0632 - Increasing Inpatient Endoscopy Volumes Using the Model for Continuous Improvement, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

