Back

Poster Session B - Monday Morning
Category: Colon
B0133 - When GI Endoscopy Shines a Light on the Endometrium
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
Estephan Zayat, MD
University of Kansas School of Medicine
Wichita, KS
Presenting Author(s)
Award: Presidential Poster Award
Marisa-Nicole Zayat, BS1, Micah Vander Griend, MPH2, Joel Alderson, DO3, Estephan Zayat, MD1
1University of Kansas School of Medicine, Wichita, KS; 2University of Kansas Medical Center, Kansas City, KS; 3Ascension Via Christi, Wichita, KS
Introduction: The differential diagnosis for gastrointestinal bleeding ranges from more benign conditions, such as hemorrhoids, to more serious ones, such as colorectal cancer. Therefore, colonoscopy is an important diagnostic tool.
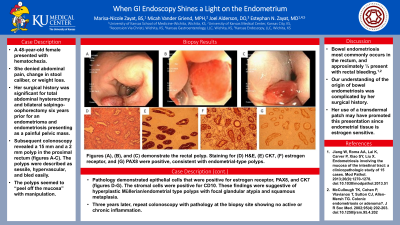
Case Description/Methods: A 48-year-old female presented with hematochezia. She denied abdominal pain, change in stool caliber, or weight loss. Her surgical history was significant for total abdominal hysterectomy and bilateral salpingo-oophorectomy six years prior for an endometrioma and endometriosis presenting as a painful pelvic mass.
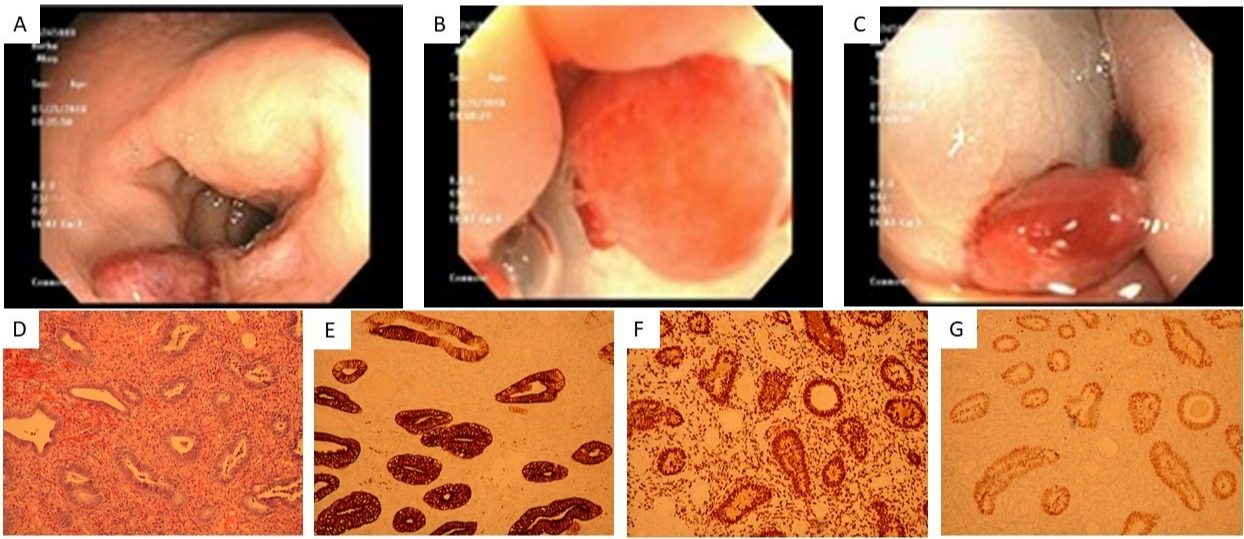
Subsequent colonoscopy revealed a 15 mm and a 2 mm polyp in the proximal rectum (figures A-C). The polyps were described as sessile, hypervascular, and bled easily. Tattoos were placed for surgical consultation. The patient was consented for endoscopic removal and surgical intervention if needed. Upon endoscopic manipulation, the polyps seemed to “peel off the mucosa.”
Pathological examination demonstrated epithelial cells that were positive for estrogen receptor, PAX8, and CK7 (figures D-G). The stromal cells were positive for CD10. These findings were suggestive of hyperplastic Müllerian/endometrial type polyps with focal glandular atypia and squamous metaplasia.
Three years later, repeat colonoscopy was largely unremarkable, with pathology at the biopsy site showing no active or chronic inflammation.
Discussion: Bowel endometriosis most commonly occurs in the rectum, and approximately ⅓ present with rectal bleeding.1,2 Her surgical history raises an important consideration of whether the tissue was seeded in the rectum prior to hysterectomy, the tissue migrated from ectopic endometrial tissue elsewhere post-hysterectomy, or the rectal tissue underwent metaplasia. Interestingly, it was noted that she was using an estradiol transdermal patch on initial consultation. This is significant since endometrial tissue is estrogen-sensitive and may have promoted this presentation.
References
1. Jiang W, Roma AA, Lai K, Carver P, Xiao SY, Liu X. Endometriosis involving the mucosa of the intestinal tract: a clinicopathologic study of 15 cases. Mod Pathol. 2013;26(9):1270-1278. doi:10.1038/modpathol.2013.51
2. McCullough TK, Cohen P, Vlavianos T, Sutton CJ, Allen-Mersh TG. Colonic endometriosis or adenoma?. J R Soc Med. 2002;95(4):202-203. doi:10.1258/jrsm.95.4.202
Disclosures:
Marisa-Nicole Zayat, BS1, Micah Vander Griend, MPH2, Joel Alderson, DO3, Estephan Zayat, MD1. B0133 - When GI Endoscopy Shines a Light on the Endometrium, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Marisa-Nicole Zayat, BS1, Micah Vander Griend, MPH2, Joel Alderson, DO3, Estephan Zayat, MD1
1University of Kansas School of Medicine, Wichita, KS; 2University of Kansas Medical Center, Kansas City, KS; 3Ascension Via Christi, Wichita, KS
Introduction: The differential diagnosis for gastrointestinal bleeding ranges from more benign conditions, such as hemorrhoids, to more serious ones, such as colorectal cancer. Therefore, colonoscopy is an important diagnostic tool.
Case Description/Methods: A 48-year-old female presented with hematochezia. She denied abdominal pain, change in stool caliber, or weight loss. Her surgical history was significant for total abdominal hysterectomy and bilateral salpingo-oophorectomy six years prior for an endometrioma and endometriosis presenting as a painful pelvic mass.
Subsequent colonoscopy revealed a 15 mm and a 2 mm polyp in the proximal rectum (figures A-C). The polyps were described as sessile, hypervascular, and bled easily. Tattoos were placed for surgical consultation. The patient was consented for endoscopic removal and surgical intervention if needed. Upon endoscopic manipulation, the polyps seemed to “peel off the mucosa.”
Pathological examination demonstrated epithelial cells that were positive for estrogen receptor, PAX8, and CK7 (figures D-G). The stromal cells were positive for CD10. These findings were suggestive of hyperplastic Müllerian/endometrial type polyps with focal glandular atypia and squamous metaplasia.
Three years later, repeat colonoscopy was largely unremarkable, with pathology at the biopsy site showing no active or chronic inflammation.
Discussion: Bowel endometriosis most commonly occurs in the rectum, and approximately ⅓ present with rectal bleeding.1,2 Her surgical history raises an important consideration of whether the tissue was seeded in the rectum prior to hysterectomy, the tissue migrated from ectopic endometrial tissue elsewhere post-hysterectomy, or the rectal tissue underwent metaplasia. Interestingly, it was noted that she was using an estradiol transdermal patch on initial consultation. This is significant since endometrial tissue is estrogen-sensitive and may have promoted this presentation.
References
1. Jiang W, Roma AA, Lai K, Carver P, Xiao SY, Liu X. Endometriosis involving the mucosa of the intestinal tract: a clinicopathologic study of 15 cases. Mod Pathol. 2013;26(9):1270-1278. doi:10.1038/modpathol.2013.51
2. McCullough TK, Cohen P, Vlavianos T, Sutton CJ, Allen-Mersh TG. Colonic endometriosis or adenoma?. J R Soc Med. 2002;95(4):202-203. doi:10.1258/jrsm.95.4.202
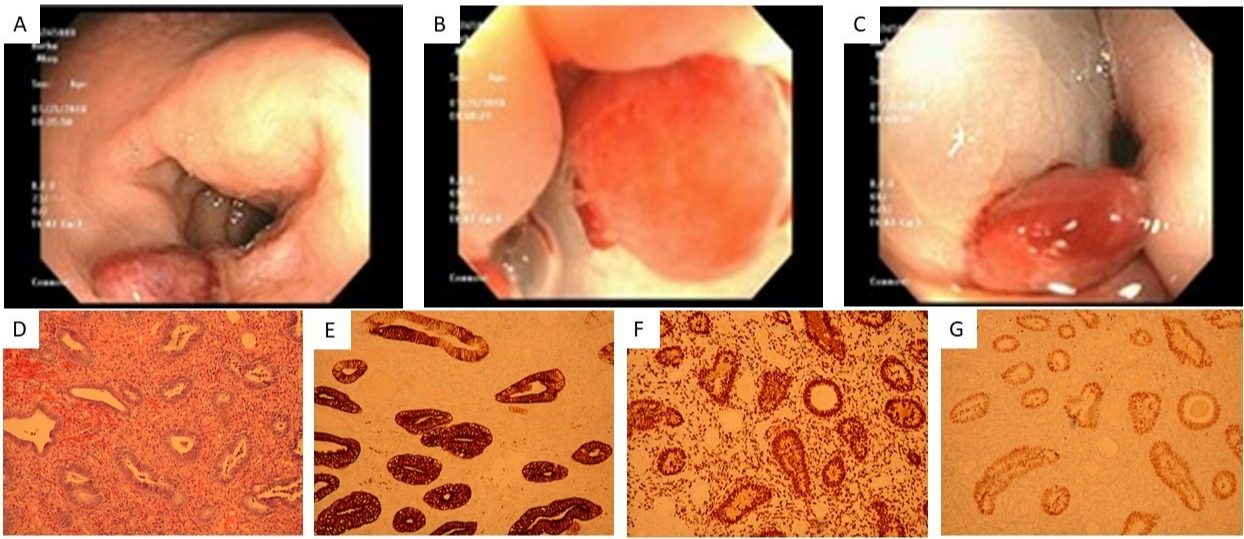
Figure: Figures (A), (B), and (C) demonstrate the rectal polyp. Staining for (D) H&E, (E) CK7, (F) estrogen receptor, and (G) PAX8 were positive, consistent with endometrial-type polyps.
Disclosures:
Marisa-Nicole Zayat indicated no relevant financial relationships.
Micah Vander Griend indicated no relevant financial relationships.
Joel Alderson indicated no relevant financial relationships.
Estephan Zayat indicated no relevant financial relationships.
Marisa-Nicole Zayat, BS1, Micah Vander Griend, MPH2, Joel Alderson, DO3, Estephan Zayat, MD1. B0133 - When GI Endoscopy Shines a Light on the Endometrium, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.


