Back

Poster Session B - Monday Morning
Category: Colon
B0097 - Age and Gender Influence the Phenotype of Pelvic Floor Dyssynergia
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Aryn Kormanis, DO
Internal Medicine Residency Program, Wake Forest University School of Medicine
Winston-Salem, NC
Presenting Author(s)
Ella LePage, MD1, Aryn Kormanis, DO1, Hiral Patel, MD1, Elizabeth Jensen, MPH, PhD2, Richard Weinberg, MD2, Nyree Thorne, MD2
1Internal Medicine Residency Program, Wake Forest University School of Medicine, Winston-Salem, NC; 2Wake Forest University School of Medicine, Winston-Salem, NC
Introduction: Pelvic floor dyssynergia (PFD) is a common cause of chronic constipation. There are four phenotypes of PFD, categorized based on the presence or absence of an adequate expulsion force and an appropriate or inappropriate external anal sphincter contraction (1). We assessed the differences in the clinical characteristics and demographics of the four phenotypes in patients with chronic constipation.
Methods: We conducted a retrospective cohort study on adult patients with constipation who underwent anorectal manometry and balloon expulsion test from January 1, 2017 to June 30, 2019. All studies were interpreted by a single gastroenterologist with expertise in anorectal disorders. Demographics and characteristics for each type of dyssynergia were analyzed using chi-square for proportions and odds ratio to account for differences. Differences found were then analyzed by t-tests or ANOVA.
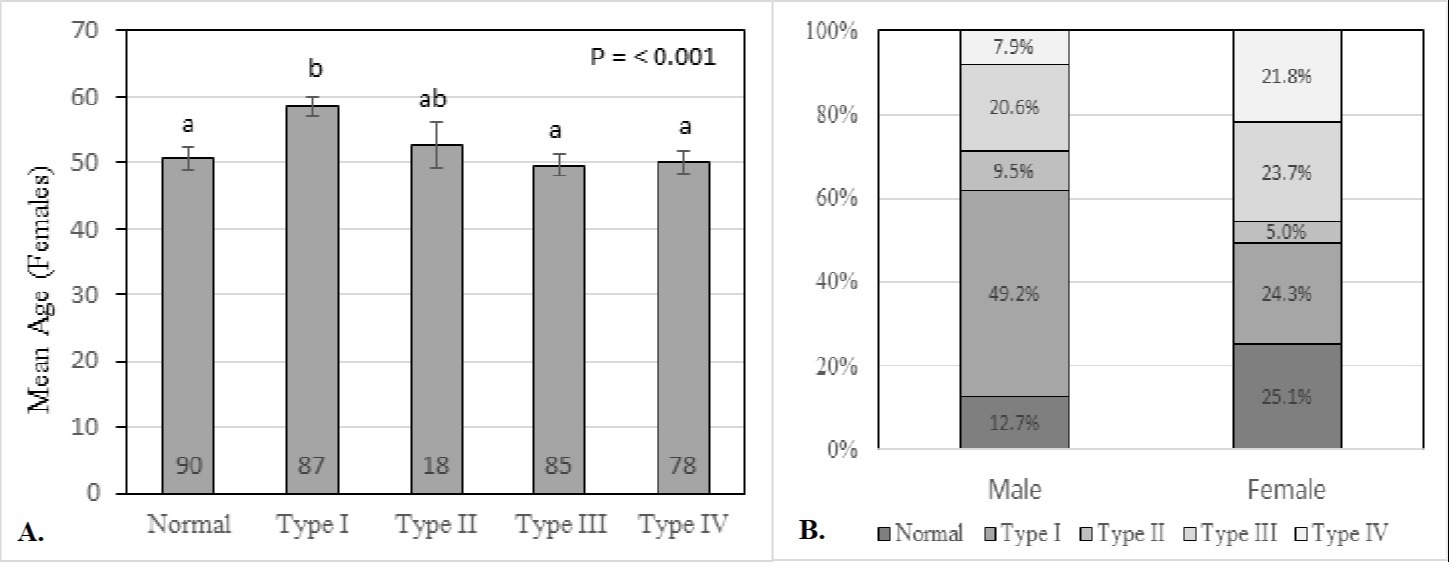
Results: Of the 421 patients diagnosed with constipation in our cohort, 323 were diagnosed with PFD. The cohort included 385 females and 63 males. The mean age was 53 years ± 0.8 years. There were significant differences in gender and age among the PFD phenotypes. Type 1 dyssynergia was the most common phenotype (n=118), followed by type 3 (n=98), type 4 (n=83), and type 2 (n=24). Females diagnosed with type 1 dyssynergia were significantly older (58.5 ± 1.5 years, p= < 0.001) than those with other phenotypes (Figure 1A). Type 1 dyssynergia was found to be significantly more common in males than females (p< 0.001) (Figure 1B). Demographic characteristics including ethnicity, BMI, and laxative use showed no significant difference between PFD phenotypes.
Discussion: Our cohort of 421 patients composes the largest study of the distribution of PFD phenotypes. Currently, there is no literature to explain how gender and age influence the phenotypes of PFD. We speculate that anatomic differences between males and females cause different dyssynergia types to be more prevalent in each gender and that the effects of aging cause type 1 dyssynergia to be more common in older women. Future prospective studies are needed to evaluate for the increased prevalence of type 1 dyssynergia in men and older women.
1. Rao, S.S., Dyssynergic defecation and biofeedback therapy. Gastroenterol Clin North Am, 2008. 37(3): p. 569-86, viii.
Disclosures:
Ella LePage, MD1, Aryn Kormanis, DO1, Hiral Patel, MD1, Elizabeth Jensen, MPH, PhD2, Richard Weinberg, MD2, Nyree Thorne, MD2. B0097 - Age and Gender Influence the Phenotype of Pelvic Floor Dyssynergia, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Internal Medicine Residency Program, Wake Forest University School of Medicine, Winston-Salem, NC; 2Wake Forest University School of Medicine, Winston-Salem, NC
Introduction: Pelvic floor dyssynergia (PFD) is a common cause of chronic constipation. There are four phenotypes of PFD, categorized based on the presence or absence of an adequate expulsion force and an appropriate or inappropriate external anal sphincter contraction (1). We assessed the differences in the clinical characteristics and demographics of the four phenotypes in patients with chronic constipation.
Methods: We conducted a retrospective cohort study on adult patients with constipation who underwent anorectal manometry and balloon expulsion test from January 1, 2017 to June 30, 2019. All studies were interpreted by a single gastroenterologist with expertise in anorectal disorders. Demographics and characteristics for each type of dyssynergia were analyzed using chi-square for proportions and odds ratio to account for differences. Differences found were then analyzed by t-tests or ANOVA.
Results: Of the 421 patients diagnosed with constipation in our cohort, 323 were diagnosed with PFD. The cohort included 385 females and 63 males. The mean age was 53 years ± 0.8 years. There were significant differences in gender and age among the PFD phenotypes. Type 1 dyssynergia was the most common phenotype (n=118), followed by type 3 (n=98), type 4 (n=83), and type 2 (n=24). Females diagnosed with type 1 dyssynergia were significantly older (58.5 ± 1.5 years, p= < 0.001) than those with other phenotypes (Figure 1A). Type 1 dyssynergia was found to be significantly more common in males than females (p< 0.001) (Figure 1B). Demographic characteristics including ethnicity, BMI, and laxative use showed no significant difference between PFD phenotypes.
Discussion: Our cohort of 421 patients composes the largest study of the distribution of PFD phenotypes. Currently, there is no literature to explain how gender and age influence the phenotypes of PFD. We speculate that anatomic differences between males and females cause different dyssynergia types to be more prevalent in each gender and that the effects of aging cause type 1 dyssynergia to be more common in older women. Future prospective studies are needed to evaluate for the increased prevalence of type 1 dyssynergia in men and older women.
1. Rao, S.S., Dyssynergic defecation and biofeedback therapy. Gastroenterol Clin North Am, 2008. 37(3): p. 569-86, viii.
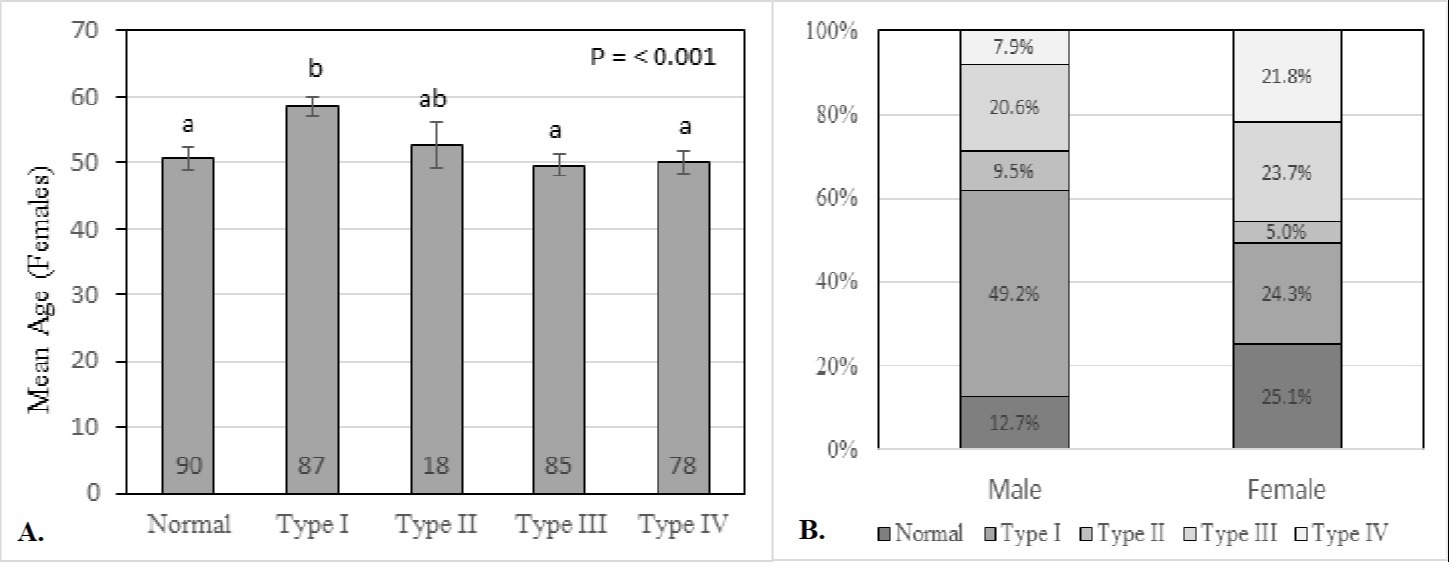
Figure: Figure 1- A. Mean age of females in each type of dyssynergia. B. Distribution of types of dyssynergia by gender.
Disclosures:
Ella LePage indicated no relevant financial relationships.
Aryn Kormanis indicated no relevant financial relationships.
Hiral Patel indicated no relevant financial relationships.
Elizabeth Jensen indicated no relevant financial relationships.
Richard Weinberg indicated no relevant financial relationships.
Nyree Thorne indicated no relevant financial relationships.
Ella LePage, MD1, Aryn Kormanis, DO1, Hiral Patel, MD1, Elizabeth Jensen, MPH, PhD2, Richard Weinberg, MD2, Nyree Thorne, MD2. B0097 - Age and Gender Influence the Phenotype of Pelvic Floor Dyssynergia, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

