Back

Poster Session B - Monday Morning
Category: Esophagus
B0225 - Esophageal Obstruction Due to Resorbable Hiatal Hernia Mesh: A Rare Surgical Complication Requiring Endoscopic Repair
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Matthew Barvo, MD
Creighton University
Phoenix, AZ
Presenting Author(s)
Matthew Barvo, MD, Hadiatou Barry, MD, MPH, Chinonso Ilo, MD, Brett Hughes, MD, Aida Rezaie, MD, Kayvon Sotoudeh, MD, Savio Reddymasu, MD
Creighton University, Phoenix, AZ
Introduction: Antireflux surgery restores the anatomical barrier, and may be a last resort option for patients with refractory GERD or PPI intolerance. Mesh reinforcement in antireflux surgery may cause complications including mesh migration, bleeding, esophageal perforation, and post-fundoplication stenosis. Intraluminal penetration of prosthetic surgical mesh is an extremely rare complication. This case report documents the diagnosis and endoscopic treatment of a patient with surgical mesh obstructing her distal esophageal lumen.
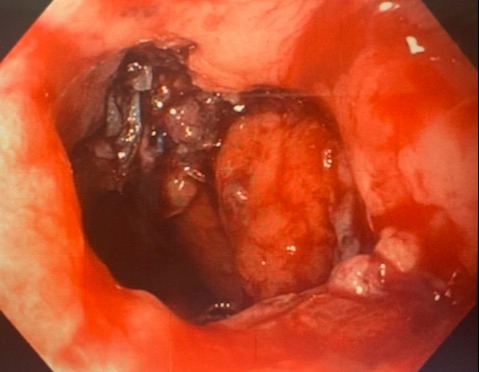
Case Description/Methods: A 73-year-old woman with a history of GERD due to large hiatal hernia underwent antireflux surgery with Toupet Fundoplication and robotic hiatal hernia repair with Phasix mesh. Shortly thereafter, she developed a perforation and stricture requiring emergency stent placement and a 2-month hospital stay. After returning home, the patient began experiencing dysphagia, regurgitation, substernal chest pain, and weight loss. She underwent an esophagram which showed delayed passage of contrast to the stomach. Upper endoscopy was performed, revealing a large piece of mesh partially obstructing the distal esophageal lumen. This was confirmed to be the Phasix mesh previously placed for her hiatal hernia repair, and the portion causing obstruction was trimmed with endoscopic suture cutters and a flexible grasper. After this procedure, the patient made a complete recovery and made no further complaints of dysphagia, chest pain, or regurgitation.
Discussion: Patients with refractory GERD or those intolerant to PPI therapy may be candidates for antireflux surgery. Mesh reinforcement of hiatal hernias greater than 5cm has been shown to decrease rates of recurrence compared to surgical suturing alone. Mesh migration is a rare complication, and most cases document permanent mesh migration through the esophageal wall. Higher erosion rates have been observed in patients with recurrent hiatal hernia repair. One study identified 50 cases of mesh migration between 1998 to 2019, with the most common erosion sites being the esophagus (50%) stomach (25%) and GE junction (23%). PTFE and polypropylene mesh were found to have the highest migration rates. Our patient experienced mesh erosion into the esophagus causing obstruction, an extremely rare complication. Providers should maintain a high index of suspicion in patients with a history of hiatal hernia repair and mesh placement who present with dysphagia or symptoms of obstruction due to the potential for mesh obstruction.
Disclosures:
Matthew Barvo, MD, Hadiatou Barry, MD, MPH, Chinonso Ilo, MD, Brett Hughes, MD, Aida Rezaie, MD, Kayvon Sotoudeh, MD, Savio Reddymasu, MD. B0225 - Esophageal Obstruction Due to Resorbable Hiatal Hernia Mesh: A Rare Surgical Complication Requiring Endoscopic Repair, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Creighton University, Phoenix, AZ
Introduction: Antireflux surgery restores the anatomical barrier, and may be a last resort option for patients with refractory GERD or PPI intolerance. Mesh reinforcement in antireflux surgery may cause complications including mesh migration, bleeding, esophageal perforation, and post-fundoplication stenosis. Intraluminal penetration of prosthetic surgical mesh is an extremely rare complication. This case report documents the diagnosis and endoscopic treatment of a patient with surgical mesh obstructing her distal esophageal lumen.
Case Description/Methods: A 73-year-old woman with a history of GERD due to large hiatal hernia underwent antireflux surgery with Toupet Fundoplication and robotic hiatal hernia repair with Phasix mesh. Shortly thereafter, she developed a perforation and stricture requiring emergency stent placement and a 2-month hospital stay. After returning home, the patient began experiencing dysphagia, regurgitation, substernal chest pain, and weight loss. She underwent an esophagram which showed delayed passage of contrast to the stomach. Upper endoscopy was performed, revealing a large piece of mesh partially obstructing the distal esophageal lumen. This was confirmed to be the Phasix mesh previously placed for her hiatal hernia repair, and the portion causing obstruction was trimmed with endoscopic suture cutters and a flexible grasper. After this procedure, the patient made a complete recovery and made no further complaints of dysphagia, chest pain, or regurgitation.
Discussion: Patients with refractory GERD or those intolerant to PPI therapy may be candidates for antireflux surgery. Mesh reinforcement of hiatal hernias greater than 5cm has been shown to decrease rates of recurrence compared to surgical suturing alone. Mesh migration is a rare complication, and most cases document permanent mesh migration through the esophageal wall. Higher erosion rates have been observed in patients with recurrent hiatal hernia repair. One study identified 50 cases of mesh migration between 1998 to 2019, with the most common erosion sites being the esophagus (50%) stomach (25%) and GE junction (23%). PTFE and polypropylene mesh were found to have the highest migration rates. Our patient experienced mesh erosion into the esophagus causing obstruction, an extremely rare complication. Providers should maintain a high index of suspicion in patients with a history of hiatal hernia repair and mesh placement who present with dysphagia or symptoms of obstruction due to the potential for mesh obstruction.
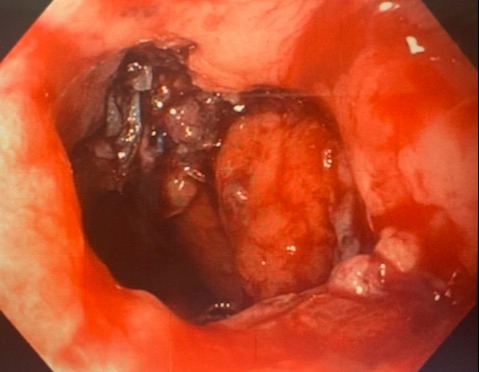
Figure: Phasix Mesh Seen Obstructing the Esophageal Lumen at the 10 O'clock Position
Disclosures:
Matthew Barvo indicated no relevant financial relationships.
Hadiatou Barry indicated no relevant financial relationships.
Chinonso Ilo indicated no relevant financial relationships.
Brett Hughes indicated no relevant financial relationships.
Aida Rezaie indicated no relevant financial relationships.
Kayvon Sotoudeh indicated no relevant financial relationships.
Savio Reddymasu indicated no relevant financial relationships.
Matthew Barvo, MD, Hadiatou Barry, MD, MPH, Chinonso Ilo, MD, Brett Hughes, MD, Aida Rezaie, MD, Kayvon Sotoudeh, MD, Savio Reddymasu, MD. B0225 - Esophageal Obstruction Due to Resorbable Hiatal Hernia Mesh: A Rare Surgical Complication Requiring Endoscopic Repair, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
