Back

Poster Session B - Monday Morning
Category: Esophagus
B0243 - Complete Esophageal Obstruction Secondary to Variceal Banding
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Colin Martyn, MD
Indiana University Internal Medicine Residency - Southwest
Vincennes, IN
Presenting Author(s)
Colin Martyn, MD1, Betty Li, MD2, Benjamin Freije, BA2, Nicholas Rogers, MD2
1Indiana University Internal Medicine Residency - Southwest, Vincennes, IN; 2Indiana University School of Medicine, Indianapolis, IN
Introduction: One effective strategy for primary and secondary prophylaxis of esophageal varices is variceal banding. Known complications include bleeding, ulceration, dysphagia, and stricture. Rarely, variceal banding can cause complete esophageal obstruction and has been described in only 14 cases to date. We present a cirrhotic patient with complete esophageal obstruction from a banded varix.
Case Description/Methods: A 78-year-old female with NASH cirrhosis and esophageal stricture was transferred to our facility for intractable nausea and vomiting after outside hospital EGD for hematemesis. The EGD found 3 columns of grade 2-3 esophageal varices and variceal band ligation was performed. Her symptoms persisted despite use of octreotide, proton pump inhibitors, and antiemetics.
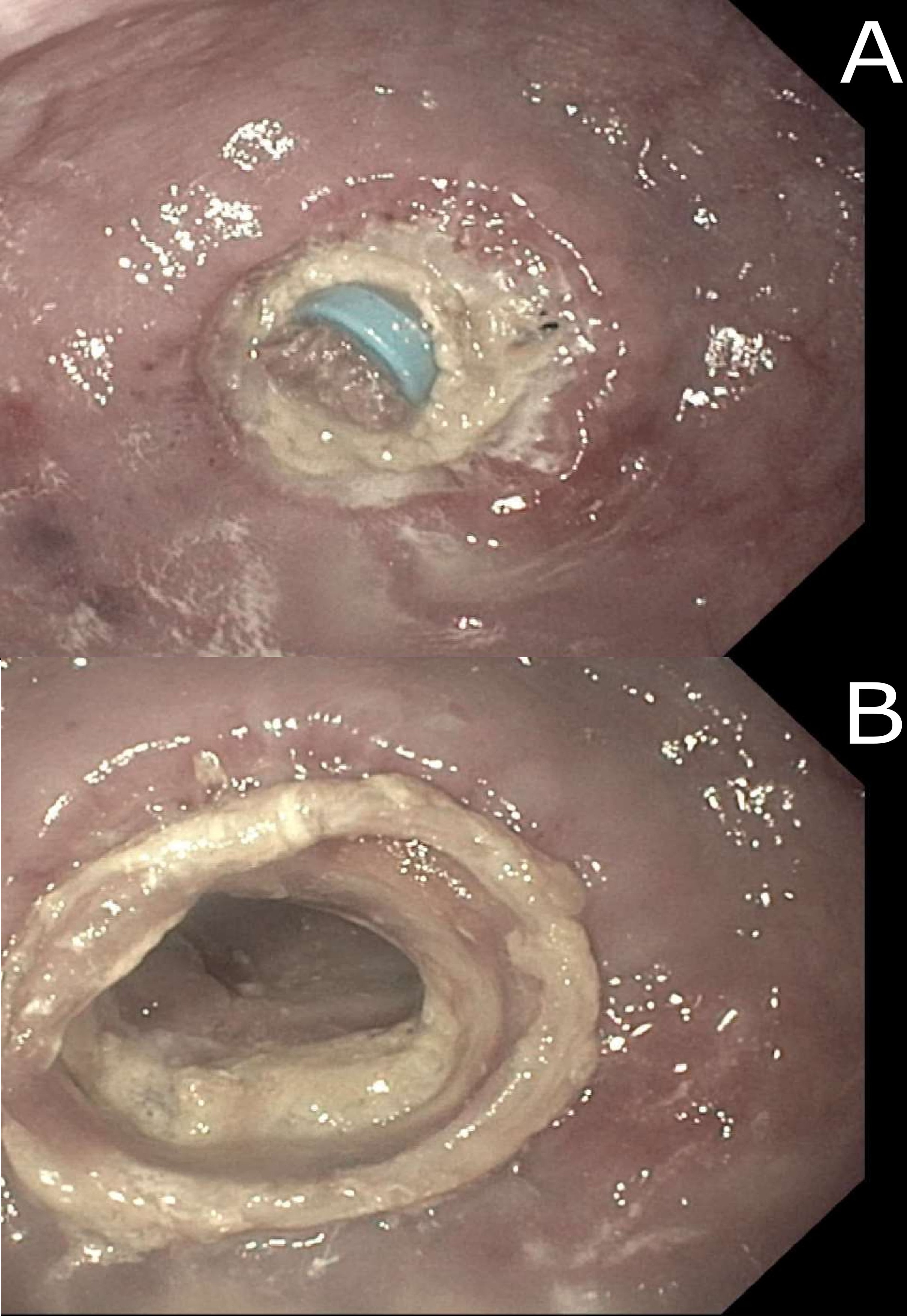
Vital signs and physical examination were unremarkable aside from epigastric tenderness with ascites. Labs demonstrated acute on chronic kidney injury and chronic normocytic anemia with normal coagulation profile. Barium esophagogram showed distal esophageal obstruction. Repeat EGD (8 days post initial EGD) found a banded varix completely obstructing the distal esophageal lumen with surrounding necrotic tissue (Figure 1-A). The esophageal lumen was restored after band removal with rat-toothed forceps. Two benign-appearing circumferential and ulcerated strictures were distal to the obstruction (Figure 1-B) and a nasojejunal tube was passed without resistance. The patient’s hospitalization was complicated by ascites and new diagnosis of hepatocellular carcinoma. Repeat EGD (1 week post band removal) was performed to place esophageal stents for persistent regurgitation and a TIPS procedure was performed. The patient discharged on hospital day 19 tolerating a dysphagia diet.
Discussion: Dysphagia after variceal banding is typically from dysmotility and esophageal spasm. Symptoms usually resolve once the banded varix sloughs off within 2-3 days after band ligation. Thus, complete esophageal obstruction by a banded varix is extremely rare. Conservative management with nil-per-os and TPN or IV fluids has been used successfully although esophageal strictures can form. Band removal is recommended by some groups to produce immediate symptomatic relief and reduce length of stay. However, strictures can still form, and iatrogenic esophageal intraluminal dissection has been described. Whether band removal improves outcomes is still a matter of debate, but dysphagia after variceal banding should raise suspicion for esophageal obstruction.
Disclosures:
Colin Martyn, MD1, Betty Li, MD2, Benjamin Freije, BA2, Nicholas Rogers, MD2. B0243 - Complete Esophageal Obstruction Secondary to Variceal Banding, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Indiana University Internal Medicine Residency - Southwest, Vincennes, IN; 2Indiana University School of Medicine, Indianapolis, IN
Introduction: One effective strategy for primary and secondary prophylaxis of esophageal varices is variceal banding. Known complications include bleeding, ulceration, dysphagia, and stricture. Rarely, variceal banding can cause complete esophageal obstruction and has been described in only 14 cases to date. We present a cirrhotic patient with complete esophageal obstruction from a banded varix.
Case Description/Methods: A 78-year-old female with NASH cirrhosis and esophageal stricture was transferred to our facility for intractable nausea and vomiting after outside hospital EGD for hematemesis. The EGD found 3 columns of grade 2-3 esophageal varices and variceal band ligation was performed. Her symptoms persisted despite use of octreotide, proton pump inhibitors, and antiemetics.
Vital signs and physical examination were unremarkable aside from epigastric tenderness with ascites. Labs demonstrated acute on chronic kidney injury and chronic normocytic anemia with normal coagulation profile. Barium esophagogram showed distal esophageal obstruction. Repeat EGD (8 days post initial EGD) found a banded varix completely obstructing the distal esophageal lumen with surrounding necrotic tissue (Figure 1-A). The esophageal lumen was restored after band removal with rat-toothed forceps. Two benign-appearing circumferential and ulcerated strictures were distal to the obstruction (Figure 1-B) and a nasojejunal tube was passed without resistance. The patient’s hospitalization was complicated by ascites and new diagnosis of hepatocellular carcinoma. Repeat EGD (1 week post band removal) was performed to place esophageal stents for persistent regurgitation and a TIPS procedure was performed. The patient discharged on hospital day 19 tolerating a dysphagia diet.
Discussion: Dysphagia after variceal banding is typically from dysmotility and esophageal spasm. Symptoms usually resolve once the banded varix sloughs off within 2-3 days after band ligation. Thus, complete esophageal obstruction by a banded varix is extremely rare. Conservative management with nil-per-os and TPN or IV fluids has been used successfully although esophageal strictures can form. Band removal is recommended by some groups to produce immediate symptomatic relief and reduce length of stay. However, strictures can still form, and iatrogenic esophageal intraluminal dissection has been described. Whether band removal improves outcomes is still a matter of debate, but dysphagia after variceal banding should raise suspicion for esophageal obstruction.
Figure: A. Complete obstruction of the distal esophageal lumen by a banded varix. B. Two circumferential and ulcerated strictures distal to the obstruction.
Disclosures:
Colin Martyn indicated no relevant financial relationships.
Betty Li indicated no relevant financial relationships.
Benjamin Freije indicated no relevant financial relationships.
Nicholas Rogers indicated no relevant financial relationships.
Colin Martyn, MD1, Betty Li, MD2, Benjamin Freije, BA2, Nicholas Rogers, MD2. B0243 - Complete Esophageal Obstruction Secondary to Variceal Banding, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

