Back

Poster Session B - Monday Morning
Category: Esophagus
B0246 - Black Esophagus (Gurvits Syndrome): A Rare Case of Acute Esophageal Necrosis in a Young Adult
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Kaycee Umeoji, MD, MBA
Arnot Ogden Medical Center
Elmira, NY
Presenting Author(s)
Kaycee Umeoji, MD, MBA, Tenzin Tesky, DO, Pranjali Dakwale, MD, Erik Raborn, DO, Asad Nasir, MD, Uma Yoganathan, MD
Arnot Ogden Medical Center, Elmira, NY
Introduction: Acute esophageal necrosis (AEN), often referred to as ‘black esophagus’ is a poorly described disease process in medical literature. A literature review showed the estimated prevalence of AEN is low with a large autopsy series in the United States reporting 0.2% in 3000 cases (1). It affects men four times more than women with peak incidence in the sixth decade of life (1). The pathogenesis entails distal esophageal ischemia resulting from hypo-perfusion secondary to hemodynamic instability. There is associated corrosive injury from gastric contents with impaired mucosal barrier systems and reparative mechanisms typically in malnourished and debilitated states. Clinical symptoms include upper GI bleeding, epigastric pain, and dysphagia (2). AEN is characterized by diffuse circumferential black mucosal discoloration in the distal esophagus that abruptly stops at the gastroesophageal junction. Treatment includes correcting coexisting co-morbidities, restoring hemodynamic stability, and acid suppression (3).
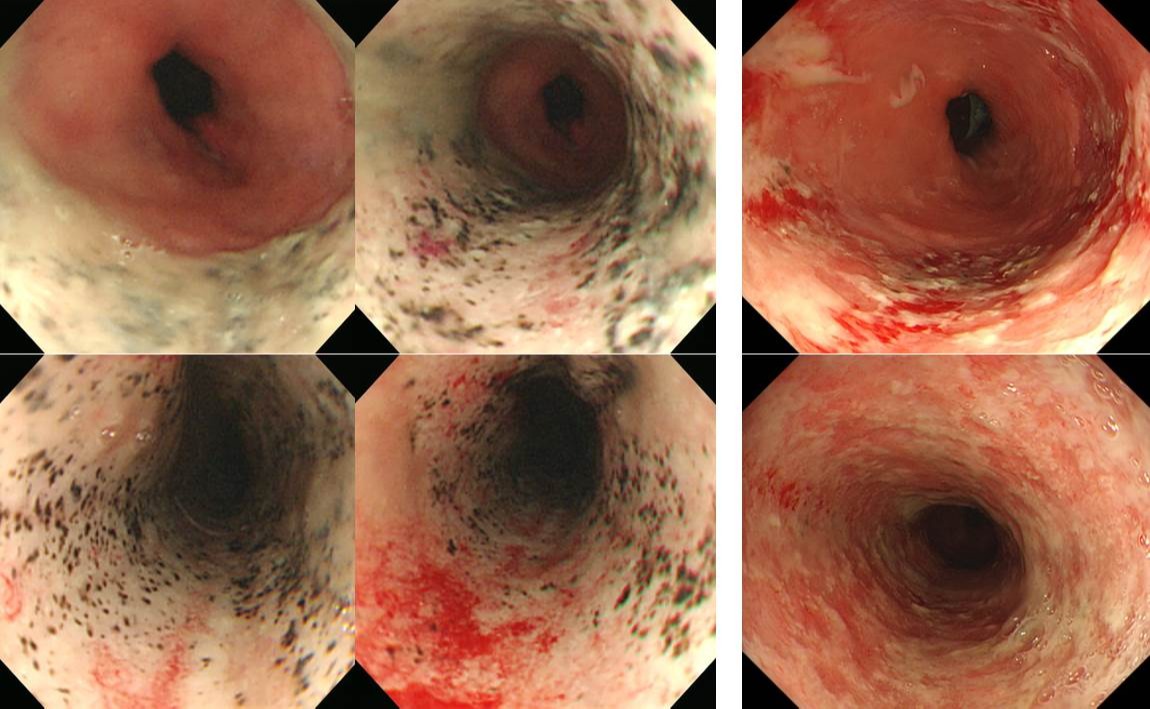
Case Description/Methods: A 39-year-old-male with poorly controlled DM (Hb A1c 14.3) was admitted with DKA and sepsis to the medical intensive care unit. The Patient was found obtunded at home. On arrival, the patient was slightly hypotensive at 80/50, with GCS of 3. Initial laboratory findings revealed a β hydroxybutyrate level of 12.46 mmol/L, FSG of 1159 and PH of 7.0. The Patient was intubated and sedated, given fluid boluses and commenced on an insulin infusion following DKA protocol. The patient was noted to have melena, four (4) days after admission. An upper GI endoscopy done revealed circumferential inflammation with black necrotic appearing esophageal mucosa present in the distal two thirds of the esophagus ending at the level of the esophageal-gastric junction. The patient was commenced on high dose proton pump inhibitors, antimicrobials, good glycemic control, fluid resuscitation and enteral diet as tolerated. The patient’s overall condition improved.
Discussion: Etiologies leading of AEN include infections, broad-spectrum antibiotics use, gastric volvulus, paraoesophageal hernias, hyperglycemia, DKA, and malignancy (6). Endoscopy finding include circumferential black discolorations with a sharp transition to normal appearing mucosa at the gastro-esophageal junction. In our patient, the underlying etiology is most likely hyperglycemia and DKA due to uncontrolled DM type 2. Initial management involves controlling the hyperglycemia with insulin and providing adequate fluid hydration.
Disclosures:
Kaycee Umeoji, MD, MBA, Tenzin Tesky, DO, Pranjali Dakwale, MD, Erik Raborn, DO, Asad Nasir, MD, Uma Yoganathan, MD. B0246 - Black Esophagus (Gurvits Syndrome): A Rare Case of Acute Esophageal Necrosis in a Young Adult, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Arnot Ogden Medical Center, Elmira, NY
Introduction: Acute esophageal necrosis (AEN), often referred to as ‘black esophagus’ is a poorly described disease process in medical literature. A literature review showed the estimated prevalence of AEN is low with a large autopsy series in the United States reporting 0.2% in 3000 cases (1). It affects men four times more than women with peak incidence in the sixth decade of life (1). The pathogenesis entails distal esophageal ischemia resulting from hypo-perfusion secondary to hemodynamic instability. There is associated corrosive injury from gastric contents with impaired mucosal barrier systems and reparative mechanisms typically in malnourished and debilitated states. Clinical symptoms include upper GI bleeding, epigastric pain, and dysphagia (2). AEN is characterized by diffuse circumferential black mucosal discoloration in the distal esophagus that abruptly stops at the gastroesophageal junction. Treatment includes correcting coexisting co-morbidities, restoring hemodynamic stability, and acid suppression (3).
Case Description/Methods: A 39-year-old-male with poorly controlled DM (Hb A1c 14.3) was admitted with DKA and sepsis to the medical intensive care unit. The Patient was found obtunded at home. On arrival, the patient was slightly hypotensive at 80/50, with GCS of 3. Initial laboratory findings revealed a β hydroxybutyrate level of 12.46 mmol/L, FSG of 1159 and PH of 7.0. The Patient was intubated and sedated, given fluid boluses and commenced on an insulin infusion following DKA protocol. The patient was noted to have melena, four (4) days after admission. An upper GI endoscopy done revealed circumferential inflammation with black necrotic appearing esophageal mucosa present in the distal two thirds of the esophagus ending at the level of the esophageal-gastric junction. The patient was commenced on high dose proton pump inhibitors, antimicrobials, good glycemic control, fluid resuscitation and enteral diet as tolerated. The patient’s overall condition improved.
Discussion: Etiologies leading of AEN include infections, broad-spectrum antibiotics use, gastric volvulus, paraoesophageal hernias, hyperglycemia, DKA, and malignancy (6). Endoscopy finding include circumferential black discolorations with a sharp transition to normal appearing mucosa at the gastro-esophageal junction. In our patient, the underlying etiology is most likely hyperglycemia and DKA due to uncontrolled DM type 2. Initial management involves controlling the hyperglycemia with insulin and providing adequate fluid hydration.
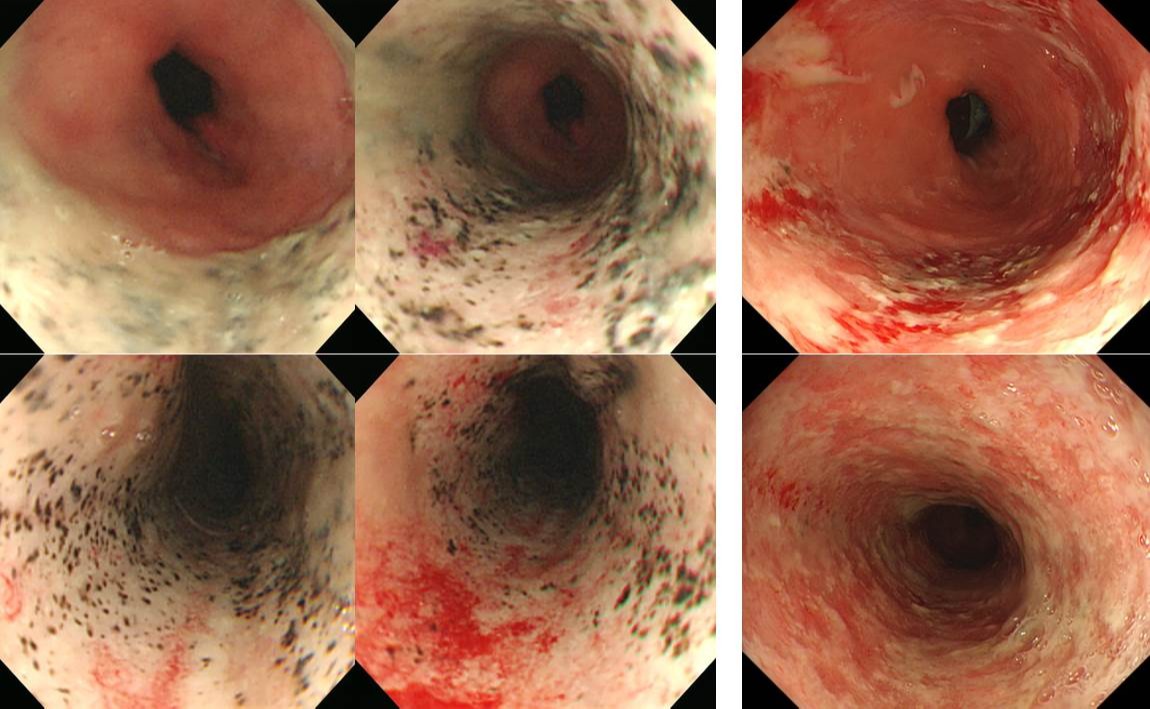
Figure: A rare case of black esophagus in a young adult
Disclosures:
Kaycee Umeoji indicated no relevant financial relationships.
Tenzin Tesky indicated no relevant financial relationships.
Pranjali Dakwale indicated no relevant financial relationships.
Erik Raborn indicated no relevant financial relationships.
Asad Nasir indicated no relevant financial relationships.
Uma Yoganathan indicated no relevant financial relationships.
Kaycee Umeoji, MD, MBA, Tenzin Tesky, DO, Pranjali Dakwale, MD, Erik Raborn, DO, Asad Nasir, MD, Uma Yoganathan, MD. B0246 - Black Esophagus (Gurvits Syndrome): A Rare Case of Acute Esophageal Necrosis in a Young Adult, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
