Back

Poster Session A - Sunday Afternoon
Category: General Endoscopy
A0284 - Conservative Management of a Gastrosplenic Fistula Due to Splenic Abscess: A Success Story
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Anurag Sachan, MBBS, MD
Post Graduate Institute of Medical Education and Research
S.A.S. Nagar, Punjab, India
Presenting Author(s)
Anurag Sachan, MBBS, MD1, Anupam Singh, MBBS, MD, DM2
1Post Graduate Institute of Medical Education and Research, S.A.S. Nagar, Punjab, India; 2Post Graduate Institute of Medical Education and Research, Chandigarh, Chandigarh, India
Introduction: Splenic abscess in itself is a rare clinical scenario with data being limited to case reports and case series. Gastrosplenic fistula is a known complication and only few gastrosplenic fistula have been described with benign etiologies. In all these cases, the patient underwent surgical management. Historically, splenectomy was the gold standard of management for splenic abscess but recent case series have established efficacy of conservative approach for splenic abscess.
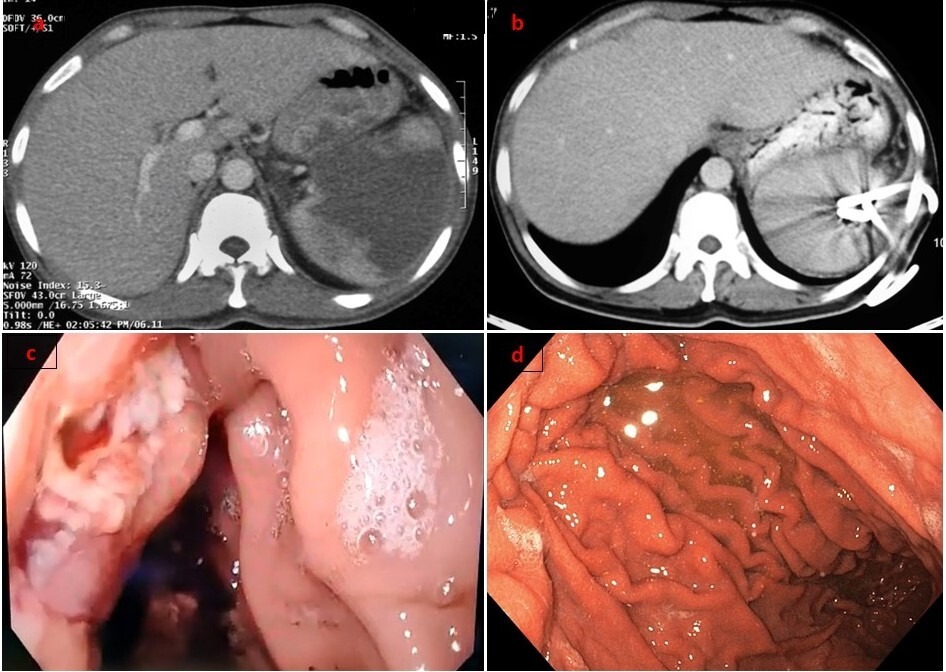
Case Description/Methods: A 35-year-old male with no known comorbidity presented with fever and recurrent malena to our emergency. He was found to have a large splenic abscess with a gastrosplenic fistula [Figure 1a] showing active ooze of pus and blood in gastric cavity on oesophagoduodenoscopy (EGD)[Figure 1c]. He was managed with broad spectrum antibiotics and multiple transfusions.A 10 french(fr) percutaneous drain (PCD) was inserted in the splenic abscess as a bridging modality to surgery. A multidisciplinary team comprising of intervention radiologist, surgeon and the treating gastroenterologist decided to try for upgrading the PCD before taking the patient for surgery due to high surgical morbidity in presence of gastrosplenic fistula and poor nutritional status.
The drain was later upgraded with two 14Fr PCD in the abscess [Figure 1b]. Pus cultures were sterile and no trophozoites were seen but the amoebic serology(IgG) was positive suggesting an amoebic etiology. On adding metronidazole, there was rapid clinical response with resolution of fever and malena. On regular follow up over 6 weeks, there was complete resolution of gastrosplenic fistula on EGD Figure 1d] with resolution of abscess.
Discussion: Our case is the first case to be reported where complete healing of gastrosplenic fistula has been demonstrated without requiring surgery. There are no set guidelines for management of splenic abscess. Historically, surgical management was considered as the gold standard of management but was associated with significant morbidity and mortality of upto 17%. Another recent review on management of gastrosplenic fistulas showed similar survival of 82% in all cases of gastrosplenic fistulas. However, in recent times safety and efficacy of PCD has been well established. PCD has been attempted in prior reports with gastrosplenic fistula but required surgery for definitive management. The choice of surgery is generally open splenectomy with partial gastric resection but laparoscopic techniques have been described.
Disclosures:
Anurag Sachan, MBBS, MD1, Anupam Singh, MBBS, MD, DM2. A0284 - Conservative Management of a Gastrosplenic Fistula Due to Splenic Abscess: A Success Story, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Post Graduate Institute of Medical Education and Research, S.A.S. Nagar, Punjab, India; 2Post Graduate Institute of Medical Education and Research, Chandigarh, Chandigarh, India
Introduction: Splenic abscess in itself is a rare clinical scenario with data being limited to case reports and case series. Gastrosplenic fistula is a known complication and only few gastrosplenic fistula have been described with benign etiologies. In all these cases, the patient underwent surgical management. Historically, splenectomy was the gold standard of management for splenic abscess but recent case series have established efficacy of conservative approach for splenic abscess.
Case Description/Methods: A 35-year-old male with no known comorbidity presented with fever and recurrent malena to our emergency. He was found to have a large splenic abscess with a gastrosplenic fistula [Figure 1a] showing active ooze of pus and blood in gastric cavity on oesophagoduodenoscopy (EGD)[Figure 1c]. He was managed with broad spectrum antibiotics and multiple transfusions.A 10 french(fr) percutaneous drain (PCD) was inserted in the splenic abscess as a bridging modality to surgery. A multidisciplinary team comprising of intervention radiologist, surgeon and the treating gastroenterologist decided to try for upgrading the PCD before taking the patient for surgery due to high surgical morbidity in presence of gastrosplenic fistula and poor nutritional status.
The drain was later upgraded with two 14Fr PCD in the abscess [Figure 1b]. Pus cultures were sterile and no trophozoites were seen but the amoebic serology(IgG) was positive suggesting an amoebic etiology. On adding metronidazole, there was rapid clinical response with resolution of fever and malena. On regular follow up over 6 weeks, there was complete resolution of gastrosplenic fistula on EGD Figure 1d] with resolution of abscess.
Discussion: Our case is the first case to be reported where complete healing of gastrosplenic fistula has been demonstrated without requiring surgery. There are no set guidelines for management of splenic abscess. Historically, surgical management was considered as the gold standard of management but was associated with significant morbidity and mortality of upto 17%. Another recent review on management of gastrosplenic fistulas showed similar survival of 82% in all cases of gastrosplenic fistulas. However, in recent times safety and efficacy of PCD has been well established. PCD has been attempted in prior reports with gastrosplenic fistula but required surgery for definitive management. The choice of surgery is generally open splenectomy with partial gastric resection but laparoscopic techniques have been described.
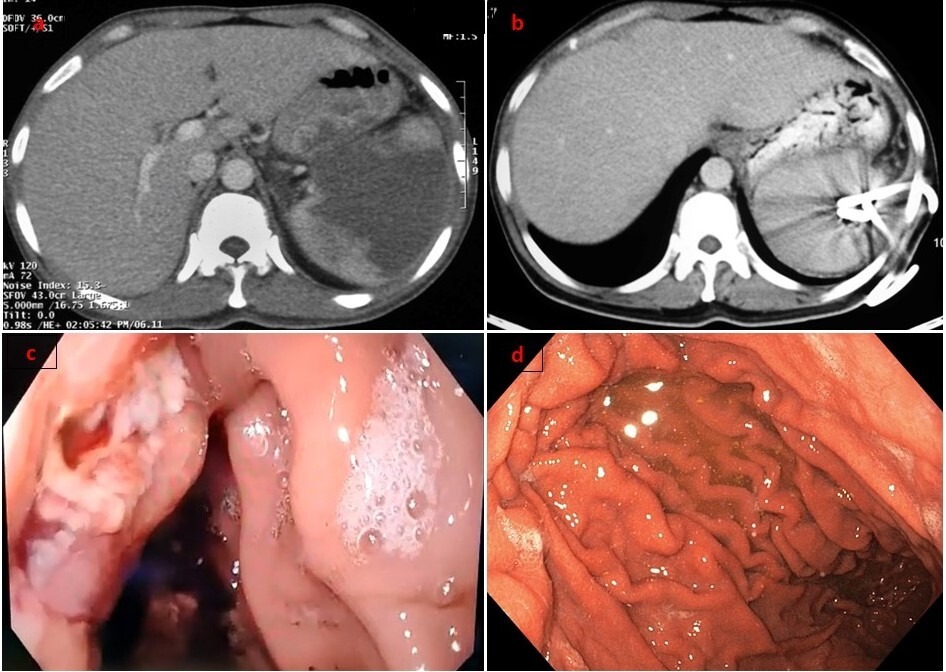
Figure: Figure 1 : (a) Large splenic abscess with loss of fat planes with stomach (b) Resolution of abscess with double pigtail catheters (c) Gastrosplenic fistula opening seen in body of stomach on endoscopy (d) Healed gastric wall after 6 weeks of initial presentation
Disclosures:
Anurag Sachan indicated no relevant financial relationships.
Anupam Singh indicated no relevant financial relationships.
Anurag Sachan, MBBS, MD1, Anupam Singh, MBBS, MD, DM2. A0284 - Conservative Management of a Gastrosplenic Fistula Due to Splenic Abscess: A Success Story, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
