Back

Poster Session B - Monday Morning
Category: Esophagus
B0255 - An Incidental Finding of Multiple Esophageal Intramural Pseudo-Diverticuli
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Aastha Chokshi, MD
Warren Alpert Medical School of Brown University
Providence, RI
Presenting Author(s)
Aastha Chokshi, MD1, Daniel Marino, MD, MBA2, May Min, MD3, Sarah M. Hyder, MD, MBA4
1Warren Alpert Medical School of Brown University , Providence, RI; 2Warren Alpert Medical School of Brown University, Providence, RI; 3Brown University, Providence, RI; 4Lifespan Physician Group - Brown University, East Providence, RI
Introduction: Esophageal intramural pseudo-diverticulosis (EIP) is characterized by multiple small outpouches protruding from the esophageal lumen. It is a rare disorder, found in 0.15% of esophagrams. Clinical manifestations include progressive dysphagia, food impaction, and occasionally bleeding. Esophageal strictures are the most common complication of EIP. We present a case of EIP thought to be due to multiple etiologies causing chronic esophageal inflammation.
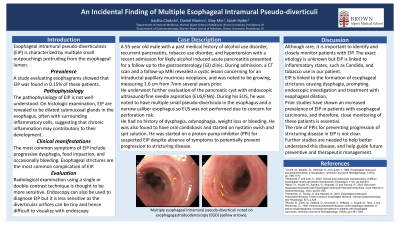
Case Description/Methods: A 55-year old male with a past medical history of alcohol use disorder, recurrent pancreatitis, tobacco use disorder, and hypertension with a recent admission for likely alcohol induced acute pancreatitis presented for a follow up to the clinic. During admission, a CT scan revealed a cystic lesion concerning for an intraductal papillary mucinous neoplasm. A follow up MRI showed a growing cystic pancreatic head lesion, measuring 1.6 cm from 7mm several years prior. He was referred to GI for further evaluation of the pancreatic cyst with endoscopic ultrasound/fine needle aspiration (EUS/FNA). During his EUS, he was noted to have multiple small pseudo-diverticula in the esophagus and a narrow caliber esophagus so EUS was not performed due to concern for perforation risk (Figure 1). He had no history of dysphagia, odynophagia, weight loss or bleeding. He was also found to have oral candidiasis and started on nystatin swish and spit solution. He was started on a proton-pump inhibitor (PPI) for suspected EIP despite absence of symptoms to potentially prevent progression to stricturing disease.
Discussion: Although rare, it is important to identify and closely monitor patients with EIP. The exact etiology is unknown but findings of EIP are linked to chronic inflammatory states. In our patient, chronic alcohol and tobacco use as well as oral candidiasis can contribute to development of EIP. EIP is linked to formation of esophageal strictures causing dysphagia symptoms prompting investigation and treatment with esophageal dilation. Our patient was asymptomatic and EIP was an incidental finding. However, prior studies have shown an increased prevalence of EIP in patients with esophageal carcinoma so close monitoring of patients with findings of EIP is essential. The role of therapies such as PPIs for preventing progression of stricturing disease in EIP is not clear. Further studies are needed to help us better understand this disease.

Disclosures:
Aastha Chokshi, MD1, Daniel Marino, MD, MBA2, May Min, MD3, Sarah M. Hyder, MD, MBA4. B0255 - An Incidental Finding of Multiple Esophageal Intramural Pseudo-Diverticuli, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Warren Alpert Medical School of Brown University , Providence, RI; 2Warren Alpert Medical School of Brown University, Providence, RI; 3Brown University, Providence, RI; 4Lifespan Physician Group - Brown University, East Providence, RI
Introduction: Esophageal intramural pseudo-diverticulosis (EIP) is characterized by multiple small outpouches protruding from the esophageal lumen. It is a rare disorder, found in 0.15% of esophagrams. Clinical manifestations include progressive dysphagia, food impaction, and occasionally bleeding. Esophageal strictures are the most common complication of EIP. We present a case of EIP thought to be due to multiple etiologies causing chronic esophageal inflammation.
Case Description/Methods: A 55-year old male with a past medical history of alcohol use disorder, recurrent pancreatitis, tobacco use disorder, and hypertension with a recent admission for likely alcohol induced acute pancreatitis presented for a follow up to the clinic. During admission, a CT scan revealed a cystic lesion concerning for an intraductal papillary mucinous neoplasm. A follow up MRI showed a growing cystic pancreatic head lesion, measuring 1.6 cm from 7mm several years prior. He was referred to GI for further evaluation of the pancreatic cyst with endoscopic ultrasound/fine needle aspiration (EUS/FNA). During his EUS, he was noted to have multiple small pseudo-diverticula in the esophagus and a narrow caliber esophagus so EUS was not performed due to concern for perforation risk (Figure 1). He had no history of dysphagia, odynophagia, weight loss or bleeding. He was also found to have oral candidiasis and started on nystatin swish and spit solution. He was started on a proton-pump inhibitor (PPI) for suspected EIP despite absence of symptoms to potentially prevent progression to stricturing disease.
Discussion: Although rare, it is important to identify and closely monitor patients with EIP. The exact etiology is unknown but findings of EIP are linked to chronic inflammatory states. In our patient, chronic alcohol and tobacco use as well as oral candidiasis can contribute to development of EIP. EIP is linked to formation of esophageal strictures causing dysphagia symptoms prompting investigation and treatment with esophageal dilation. Our patient was asymptomatic and EIP was an incidental finding. However, prior studies have shown an increased prevalence of EIP in patients with esophageal carcinoma so close monitoring of patients with findings of EIP is essential. The role of therapies such as PPIs for preventing progression of stricturing disease in EIP is not clear. Further studies are needed to help us better understand this disease.

Figure: Figure 1. Multiple esophageal intramural psuedo-diverticuli noted on esophagoduodenoscopy (EGD) (yellow arrows).
Disclosures:
Aastha Chokshi indicated no relevant financial relationships.
Daniel Marino indicated no relevant financial relationships.
May Min indicated no relevant financial relationships.
Sarah Hyder indicated no relevant financial relationships.
Aastha Chokshi, MD1, Daniel Marino, MD, MBA2, May Min, MD3, Sarah M. Hyder, MD, MBA4. B0255 - An Incidental Finding of Multiple Esophageal Intramural Pseudo-Diverticuli, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
