Back

Poster Session B - Monday Morning
Category: Functional Bowel Disease
B0274 - IgG-based Elimination Diets for Patients with IBS: Results From a Prospective, Multi-Center, Double-Blind, Placebo-Controlled Trial
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- AL
Anthony Lembo, MD, FACG
Beth Israel Deaconess Medical Center and Harvard Medical School
Boston, Massachusetts
Presenting Author(s)
Award: Presidential Poster Award
Anthony Lembo, MD, FACG1, William D. Chey, MD2, Brian E. Lacy, MD, PhD, FACG3, Charles W. Randall, MD4, Tisha Lundsford, MD5, Eamonn M. Quigley, MD, MACG6, Brooks D. Cash, MD, FACG7, Elisabeth I. Laderman, PhD8
1Beth Israel Deaconess Medical Center and Harvard Medical School, Boston, MA; 2Michigan Medicine, Ann Arbor, MI; 3Mayo Clinic, Jacksonville, FL; 4Gastroenterology Clinic of San Antonio, San Antonio, TX; 5Mayo Clinic Arizona, Scottsdale, AZ; 6Houston Methodist Hospital, Houston, TX; 7University of Texas Health Science Center, Houston, TX; 8Biomerica, Inc., Garden Grove, CA
Introduction: Studies indicate that diet modification can improve symptoms in patients with IBS. Food intolerances/sensitivities are common in patients with IBS but outcomes following self-directed elimination diets are poor. The role of IgG antibodies in identifying patients with food sensitivities is controversial. This study was designed to evaluate the utility of a novel, proprietary IgG-based elimination diet to improve symptoms in IBS patients.
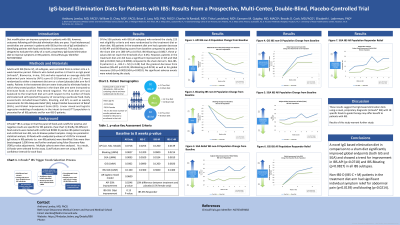
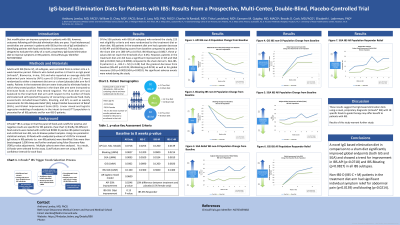
Methods: Adults with IBS (Rome IV), all subtypes, were enrolled from 6 centers into a 2-week baseline period. Patients who tested positive ≥ 1 food in an IgG panel (InFoods®, Biomerica, Irvine, CA) and who reported an average daily IBS abdominal pain intensity(API) score (0-10) between ≥3 - ≤7.5 were randomized to either a treatment diet arm or a sham(placebo) diet arm for 8 weeks. Patients in the treatment diet arm were instructed to eliminate foods to which they tested positive. Patients in the sham diet arm were instructed to eliminate foods to which they tested negative. The sham diet arm was balanced to the active diet arm with respect to the number of foods eliminated and self-reported frequency of consuming a particular food. Daily assessments included bowel habits, bloating, and API, as well as weekly assessments for IBS Adequate Relief(AR), Subject Global Assessment of Relief(SGA), and Global Improvement Scale(GIS). Linear mixed and logistic regression modeling of endpoints in the intent-to-treat (ITT) population is presented for all IBS patients and for non-IBS-D patients.
Results: 556 patients with IBS(all subtypes) entered the screening phase, 223 met eligibility criteria and entered the double-blind placebo-controlled diet treatment phase. IBS patients in the treatment diet arm showed a greater decrease in IBS-API and IBS-Bloating scores from baseline compared to patients in the sham diet arm (IBS-API p=0.0718; IBS-Bloating p=0.0827, these p-values did not reach the threshold of p< 0.05). However, GIS and SGA did show significant improvement (GIS p=0.0302; SGA p=0.0093). Non-IBS-D patients (n=149) showed the greatest decrease from baseline (IBS-API p=0.0139; IBS-Bloating p=0.0214) as well as for global measures (GIS p=0.0020; SGA p=0.0010). No significant adverse events were noted during the study.
Discussion: These results suggest that IgG-based elimination diets using a novel, proprietary diagnostic to guide therapy may offer benefit to patients with IBS. Results of this study should help guide other studies.

Disclosures:
Anthony Lembo, MD, FACG1, William D. Chey, MD2, Brian E. Lacy, MD, PhD, FACG3, Charles W. Randall, MD4, Tisha Lundsford, MD5, Eamonn M. Quigley, MD, MACG6, Brooks D. Cash, MD, FACG7, Elisabeth I. Laderman, PhD8. B0274 - IgG-based Elimination Diets for Patients with IBS: Results From a Prospective, Multi-Center, Double-Blind, Placebo-Controlled Trial, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Anthony Lembo, MD, FACG1, William D. Chey, MD2, Brian E. Lacy, MD, PhD, FACG3, Charles W. Randall, MD4, Tisha Lundsford, MD5, Eamonn M. Quigley, MD, MACG6, Brooks D. Cash, MD, FACG7, Elisabeth I. Laderman, PhD8
1Beth Israel Deaconess Medical Center and Harvard Medical School, Boston, MA; 2Michigan Medicine, Ann Arbor, MI; 3Mayo Clinic, Jacksonville, FL; 4Gastroenterology Clinic of San Antonio, San Antonio, TX; 5Mayo Clinic Arizona, Scottsdale, AZ; 6Houston Methodist Hospital, Houston, TX; 7University of Texas Health Science Center, Houston, TX; 8Biomerica, Inc., Garden Grove, CA
Introduction: Studies indicate that diet modification can improve symptoms in patients with IBS. Food intolerances/sensitivities are common in patients with IBS but outcomes following self-directed elimination diets are poor. The role of IgG antibodies in identifying patients with food sensitivities is controversial. This study was designed to evaluate the utility of a novel, proprietary IgG-based elimination diet to improve symptoms in IBS patients.
Methods: Adults with IBS (Rome IV), all subtypes, were enrolled from 6 centers into a 2-week baseline period. Patients who tested positive ≥ 1 food in an IgG panel (InFoods®, Biomerica, Irvine, CA) and who reported an average daily IBS abdominal pain intensity(API) score (0-10) between ≥3 - ≤7.5 were randomized to either a treatment diet arm or a sham(placebo) diet arm for 8 weeks. Patients in the treatment diet arm were instructed to eliminate foods to which they tested positive. Patients in the sham diet arm were instructed to eliminate foods to which they tested negative. The sham diet arm was balanced to the active diet arm with respect to the number of foods eliminated and self-reported frequency of consuming a particular food. Daily assessments included bowel habits, bloating, and API, as well as weekly assessments for IBS Adequate Relief(AR), Subject Global Assessment of Relief(SGA), and Global Improvement Scale(GIS). Linear mixed and logistic regression modeling of endpoints in the intent-to-treat (ITT) population is presented for all IBS patients and for non-IBS-D patients.
Results: 556 patients with IBS(all subtypes) entered the screening phase, 223 met eligibility criteria and entered the double-blind placebo-controlled diet treatment phase. IBS patients in the treatment diet arm showed a greater decrease in IBS-API and IBS-Bloating scores from baseline compared to patients in the sham diet arm (IBS-API p=0.0718; IBS-Bloating p=0.0827, these p-values did not reach the threshold of p< 0.05). However, GIS and SGA did show significant improvement (GIS p=0.0302; SGA p=0.0093). Non-IBS-D patients (n=149) showed the greatest decrease from baseline (IBS-API p=0.0139; IBS-Bloating p=0.0214) as well as for global measures (GIS p=0.0020; SGA p=0.0010). No significant adverse events were noted during the study.
Discussion: These results suggest that IgG-based elimination diets using a novel, proprietary diagnostic to guide therapy may offer benefit to patients with IBS. Results of this study should help guide other studies.

Figure: Summary of GLMM and LMM analyses
Disclosures:
Anthony Lembo: Alkermes – Consultant. Arena Pharmaceuticals, Inc. – Consultant. Bayer – Consultant. Bristol-Myers Squibb – Stock Options. Gemelli Biotech – Consultant. Ironwood Pharmaceuticals, Inc. – Consultant. Johnson & Johnson – Stock Options. OrphoMed, Inc. – Consultant. Salix Pharmaceuticals, Inc. – Consultant. Shire, a Takeda company – Consultant. Takeda Pharmaceuticals – Consultant. Vibrant – Advisor or Review Panel Member. Vibrant Pharma Inc. – Consultant.
William Chey: Abbvie – Consultant. Allakos – Consultant. Alnylam – Consultant. Arena – Consultant. Biomerica – Consultant. Commonwealth Diagnostics International – Consultant. Gemelli – Consultant. GI OnDEMAND – Stock Options. Ironwood – Consultant. Isothrive – Consultant. Isothrive – Stock Options. Modify Health – Stock Options. Nestle – Consultant. Phathom – Consultant. Progenity – Consultant. QOL Medical – Consultant, Grant/Research Support. Redhill – Consultant. Salix – Consultant, Grant/Research Support. Urovant – Consultant. Vibrant – Consultant.
Brian Lacy: Allakos – Advisory Committee/Board Member. Allergan Pharmaceuticals – Advisory Committee/Board Member. Arena Pharmaceuticals, Inc. – Advisory Committee/Board Member. Cosmos – Advisory Committee/Board Member. Ironwood Pharmaceuticals, Inc. – Advisory Committee/Board Member. Salix Pharmaceuticals, Inc. – Advisory Committee/Board Member. Viver Health – Consultant.
Charles Randall: 9. Meters – Independent Contractor. Abbvie – Speakers Bureau. Astra zeneca – Grant/Research Support. Bioamerica – Grant/Research Support. BioAmerica – Grant/Research Support. BMS – Advisory Committee/Board Member. BMS – Advisory Committee/Board Member, Grant/Research Support. BMS – Grant/Research Support. Eli Lilly – Consultant, Grant/Research Support. Exact sciences – Grant/Research Support. Gilead – Advisory Committee/Board Member. Gilead – Advisory Committee/Board Member, Grant/Research Support. Gilead – Grant/Research Support. Janssen – Advisor or Review Panel Member. Janssen – Advisor or Review Panel Member, Advisory Committee/Board Member. Janssen – Advisory Committee/Board Member, Consultant. Janssen – Consultant, Grant/Research Support. Janssen – Grant/Research Support, Independent Contractor, Speakers Bureau. Janssen – Speakers Bureau. Phathom – Grant/Research Support, Speakers Bureau. Regeneron – Grant/Research Support. Regeneron – Grant/Research Support. Takeda – Grant/Research Support. Takeda – Grant/Research Support. Ucb – Advisory Committee/Board Member. UCB – Advisory Committee/Board Member.
Tisha Lundsford indicated no relevant financial relationships.
Eamonn Quigley: Biomerica – Grant/Research Support. Vibrant – Advisor or Review Panel Member. Vibrant – Clinical Advisory Board.
Brooks Cash: AbbVie – Consultant, Speakers Bureau. Ardelyx – Consultant, Speakers Bureau. Motus – Consultant. QOL – Consultant, Speakers Bureau. RedHill – Consultant, Speakers Bureau. Salix – Consultant, Speakers Bureau. Takeda Pharmaceuticals – Consultant.
Elisabeth Laderman indicated no relevant financial relationships.
Anthony Lembo, MD, FACG1, William D. Chey, MD2, Brian E. Lacy, MD, PhD, FACG3, Charles W. Randall, MD4, Tisha Lundsford, MD5, Eamonn M. Quigley, MD, MACG6, Brooks D. Cash, MD, FACG7, Elisabeth I. Laderman, PhD8. B0274 - IgG-based Elimination Diets for Patients with IBS: Results From a Prospective, Multi-Center, Double-Blind, Placebo-Controlled Trial, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.


