Back

Poster Session A - Sunday Afternoon
Category: Biliary/Pancreas
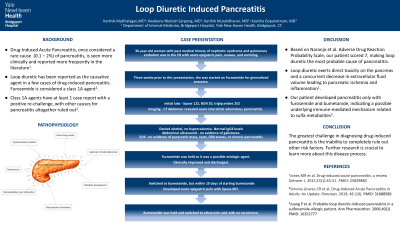
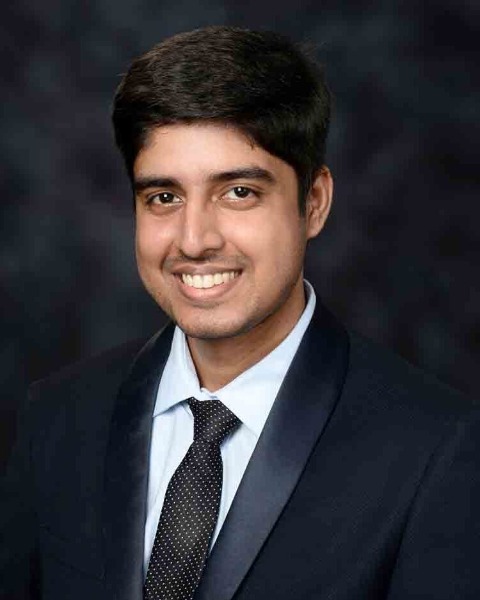
A0052 - Loop Diuretic-Induced Pancreatitis
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio
Karthik Mathialagan, MD
Bridgeport Hospital, Yale New Haven Health
Trumbull, CT
Presenting Author(s)
Karthik Mathialagan, MD, Kwabena Nketiah Sarpong, MD, Karthik Muralidharan, MD, Kavitha Gopalratnam, MD
Bridgeport Hospital, Yale New Haven Health, Bridgeport, CT
Introduction: Acute Pancreatitis (AP) has become the leading cause of hospitalization related to Gastrointestinal diseases in the US in recent years. More often than not, AP is usually associated with gall stones and alcohol abuse disorder. Drug-Induced Pancreatitis (DIP), once considered a rare cause (0.1 – 2%) of AP, is seen more clinically and is reported more frequently in the literature lately. Here, we describe a patient who developed acute pancreatitis after being on loop diuretic for a short duration.
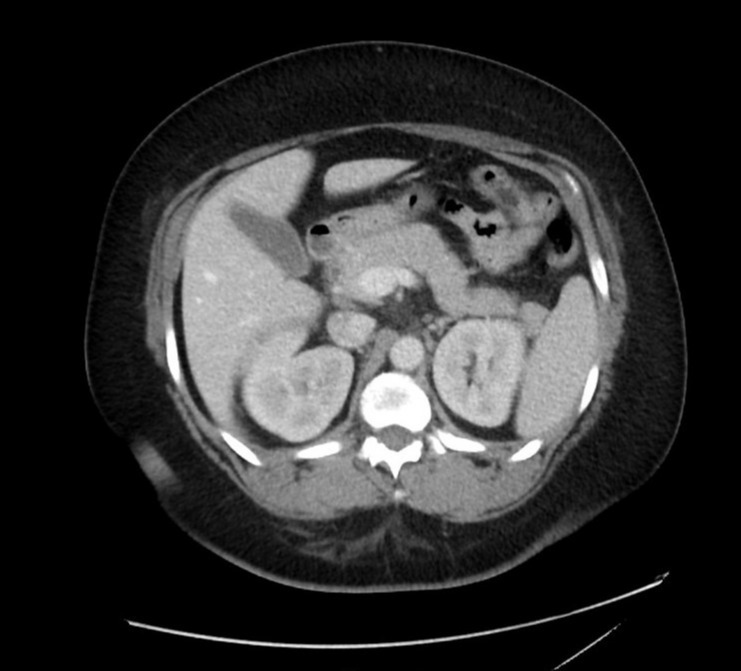
Case Description/Methods: A 36-year-old woman with past medical history of nephrotic syndrome of unknown etiology, mixed connective tissue disease, and pulmonary embolism presented to the ED with acute epigastric pain, nausea and vomiting. Her medications included Prednisone, Plaquenil, and Eliquis. Three weeks prior to this presentation, she was started on furosemide for anasarca. In the ED labs, her lipase was 122, BUN 20, WBC 8.8, and CT abdomen revealed acute interstitial edematous pancreatitis. She was treated with IV fluids and pain control. On workup, She denied alcohol and illicit drug usage, triglycerides were not significantly elevated (252), no hypercalcemia, and abdominal ultrasound showed no evidence of gallstones. IgG4 was negative, denied hereditary pancreatitis and sulfa drug allergy. Furosemide was held as it was a possible etiologic agent, and she improved. A month later, she was switched to bumetanide as an outpatient, but within 10 days of starting bumetanide, she was readmitted with epigastric pain and Lipase 907 and was diagnosed with AP. She had an Endoscopic ultrasound (EUS) that showed no evidence of pancreatic mass, cysts, common bile duct stones, or evidence of chronic pancreatitis. Bumetanide was held and later switched to ethacrynic acid with the resolution of symptoms.
Discussion: Though perceived as a rare cause, the true incidence of DIP is much higher, as they are predominantly underreported and underdiagnosed. Based on Naranjo et al. Naranjo adverse drug reaction probability scale, our patient scored 7 (yes to questions 1,2,3,4,10), making loop diuretic the most probable cause of AP. Literature suggests loop diuretic exerts direct toxicity on pancreas and a concurrent decrease in extracellular fluid volume leads to pancreatic ischemia and inflammation. Nevertheless, our patient developed AP only with furosemide and bumetanide, indicating an added immune-mediated pathway involving sulfa metabolites likely contributing to AP, which also has been reported in the literature.
Disclosures:
Karthik Mathialagan, MD, Kwabena Nketiah Sarpong, MD, Karthik Muralidharan, MD, Kavitha Gopalratnam, MD. A0052 - Loop Diuretic-Induced Pancreatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Bridgeport Hospital, Yale New Haven Health, Bridgeport, CT
Introduction: Acute Pancreatitis (AP) has become the leading cause of hospitalization related to Gastrointestinal diseases in the US in recent years. More often than not, AP is usually associated with gall stones and alcohol abuse disorder. Drug-Induced Pancreatitis (DIP), once considered a rare cause (0.1 – 2%) of AP, is seen more clinically and is reported more frequently in the literature lately. Here, we describe a patient who developed acute pancreatitis after being on loop diuretic for a short duration.
Case Description/Methods: A 36-year-old woman with past medical history of nephrotic syndrome of unknown etiology, mixed connective tissue disease, and pulmonary embolism presented to the ED with acute epigastric pain, nausea and vomiting. Her medications included Prednisone, Plaquenil, and Eliquis. Three weeks prior to this presentation, she was started on furosemide for anasarca. In the ED labs, her lipase was 122, BUN 20, WBC 8.8, and CT abdomen revealed acute interstitial edematous pancreatitis. She was treated with IV fluids and pain control. On workup, She denied alcohol and illicit drug usage, triglycerides were not significantly elevated (252), no hypercalcemia, and abdominal ultrasound showed no evidence of gallstones. IgG4 was negative, denied hereditary pancreatitis and sulfa drug allergy. Furosemide was held as it was a possible etiologic agent, and she improved. A month later, she was switched to bumetanide as an outpatient, but within 10 days of starting bumetanide, she was readmitted with epigastric pain and Lipase 907 and was diagnosed with AP. She had an Endoscopic ultrasound (EUS) that showed no evidence of pancreatic mass, cysts, common bile duct stones, or evidence of chronic pancreatitis. Bumetanide was held and later switched to ethacrynic acid with the resolution of symptoms.
Discussion: Though perceived as a rare cause, the true incidence of DIP is much higher, as they are predominantly underreported and underdiagnosed. Based on Naranjo et al. Naranjo adverse drug reaction probability scale, our patient scored 7 (yes to questions 1,2,3,4,10), making loop diuretic the most probable cause of AP. Literature suggests loop diuretic exerts direct toxicity on pancreas and a concurrent decrease in extracellular fluid volume leads to pancreatic ischemia and inflammation. Nevertheless, our patient developed AP only with furosemide and bumetanide, indicating an added immune-mediated pathway involving sulfa metabolites likely contributing to AP, which also has been reported in the literature.
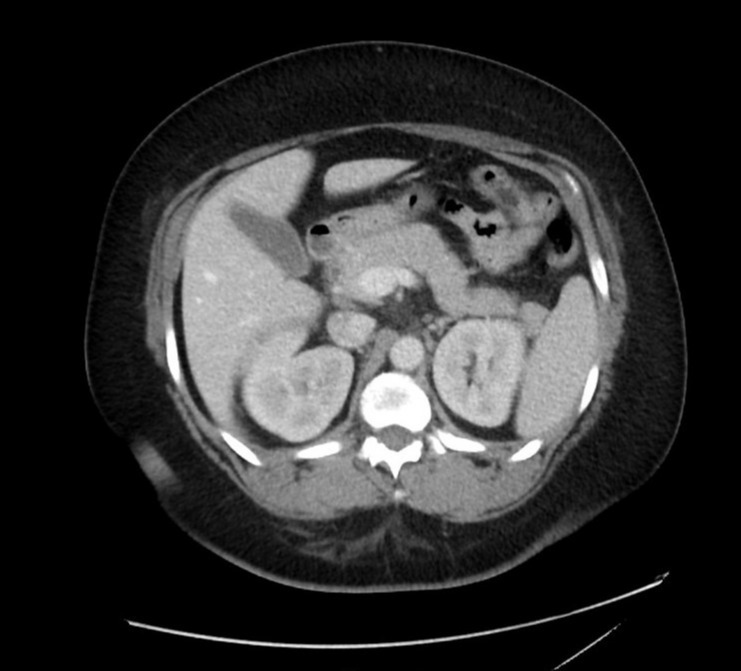
Figure: CT abdomen from the time of initial ED presentation demonstrating edematous pancreas with minimal surrounding fat stranding and fluid in the region of the head and uncinate process, consistent with acute interstitial pancreatitis.
Disclosures:
Karthik Mathialagan indicated no relevant financial relationships.
Kwabena Nketiah Sarpong indicated no relevant financial relationships.
Karthik Muralidharan indicated no relevant financial relationships.
Kavitha Gopalratnam indicated no relevant financial relationships.
Karthik Mathialagan, MD, Kwabena Nketiah Sarpong, MD, Karthik Muralidharan, MD, Kavitha Gopalratnam, MD. A0052 - Loop Diuretic-Induced Pancreatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
