Back

Poster Session B - Monday Morning
Category: IBD
B0353 - Physical Activity as an Adjunct Therapy in Quiescent and Mildly Active Inflammatory Bowel Disease: A Systematic Review and Meta-Analysis
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Banke Oketola, MSc
Applied Health Sciences Program, Faculty of Graduate Studies, University of Manitoba
Winnipeg, MB, Canada
Presenting Author(s)
Banke Oketola, MSc1, Olayinka Akinrolie, MSc1, Sandra Webber, PhD2, Harminder Singh, MD, MPH3, Nicole Askin, MLIS4, Rasheda Rabbani, MSc, PhD5, Ahmed Abou-Setta, MD, PhD3
1Applied Health Sciences Program, Faculty of Graduate Studies, University of Manitoba, Winnipeg, MB, Canada; 2College of Rehabilitation Sciences, Rady Faculty of Health Sciences, University of Manitoba, Winnipeg, MB, Canada; 3Max Rady College of Medicine, Rady Faculty of Health Sciences, University of Manitoba, Winnipeg, MB, Canada; 4University of Manitoba, Winnipeg, MB, Canada; 5George & Fay Yee Center for Healthcare Innovation, Rady Faculty of Health Sciences, University of Manitoba, Winnipeg, MB, Canada
Introduction: Individuals with IBD in remission (i.e. quiescent IBD) can continue to have several symptoms, such as fatigue and depression. Physical activity (PA) may benefit people with quiescent IBD by improving immunological response and psychological health. The aim of our study was to distill available evidence on the efficacy and safety of PA to relieve persistent symptoms of fatigue, joint pain, abdominal pain, stress, anxiety, and depression; and improve health-related quality of life (HRQoL) in individuals with quiescent or mildly active IBD.
Methods: We searched for RCTs and non-RCTs in eight databases, trial registries and conference proceedings. Trials using PA as an adjunct therapy in the management of adults ( >18 years) with quiescent or mildly active IBD, published in English between 2011 and 2021 were identified. Risk of bias of RCTs and non-RCTs was assessed using the Cochrane Risk of Bias tool and Newcastle Ottawa scale respectively.
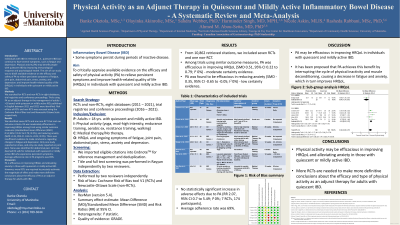
Results: We identified seven RCTs and one non-RCT that met our inclusion criteria. PA was moderately efficacious in improving HRQoL among trials using similar outcome measures (standardized mean difference (SMD) 0.51, 95% CI 0.22 to 0.79; I2 0%), and reducing anxiety (SMD -0.35, 95% CI -0.65 to -0.05; I2 0%). There was insufficient evidence to make conclusions regarding changes in fatigue and depression. Only one study reported on stress, and only one study reported on joint pain. None was identified for abdominal pain. All trials deemed PA safe for individuals with quiescent or mildly active IBD who experience persistent symptoms. Average adherence rate in PA programs was 69%.
Discussion: PA is efficacious in improving HRQoL and alleviating anxiety in those with quiescent or mildly active IBD. However, more RCTs are required to precisely estimate the magnitude of effect and make more definitive conclusions about the efficacy of PA as an adjunct therapy for adults with IBD.

Disclosures:
Banke Oketola, MSc1, Olayinka Akinrolie, MSc1, Sandra Webber, PhD2, Harminder Singh, MD, MPH3, Nicole Askin, MLIS4, Rasheda Rabbani, MSc, PhD5, Ahmed Abou-Setta, MD, PhD3. B0353 - Physical Activity as an Adjunct Therapy in Quiescent and Mildly Active Inflammatory Bowel Disease: A Systematic Review and Meta-Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Applied Health Sciences Program, Faculty of Graduate Studies, University of Manitoba, Winnipeg, MB, Canada; 2College of Rehabilitation Sciences, Rady Faculty of Health Sciences, University of Manitoba, Winnipeg, MB, Canada; 3Max Rady College of Medicine, Rady Faculty of Health Sciences, University of Manitoba, Winnipeg, MB, Canada; 4University of Manitoba, Winnipeg, MB, Canada; 5George & Fay Yee Center for Healthcare Innovation, Rady Faculty of Health Sciences, University of Manitoba, Winnipeg, MB, Canada
Introduction: Individuals with IBD in remission (i.e. quiescent IBD) can continue to have several symptoms, such as fatigue and depression. Physical activity (PA) may benefit people with quiescent IBD by improving immunological response and psychological health. The aim of our study was to distill available evidence on the efficacy and safety of PA to relieve persistent symptoms of fatigue, joint pain, abdominal pain, stress, anxiety, and depression; and improve health-related quality of life (HRQoL) in individuals with quiescent or mildly active IBD.
Methods: We searched for RCTs and non-RCTs in eight databases, trial registries and conference proceedings. Trials using PA as an adjunct therapy in the management of adults ( >18 years) with quiescent or mildly active IBD, published in English between 2011 and 2021 were identified. Risk of bias of RCTs and non-RCTs was assessed using the Cochrane Risk of Bias tool and Newcastle Ottawa scale respectively.
Results: We identified seven RCTs and one non-RCT that met our inclusion criteria. PA was moderately efficacious in improving HRQoL among trials using similar outcome measures (standardized mean difference (SMD) 0.51, 95% CI 0.22 to 0.79; I2 0%), and reducing anxiety (SMD -0.35, 95% CI -0.65 to -0.05; I2 0%). There was insufficient evidence to make conclusions regarding changes in fatigue and depression. Only one study reported on stress, and only one study reported on joint pain. None was identified for abdominal pain. All trials deemed PA safe for individuals with quiescent or mildly active IBD who experience persistent symptoms. Average adherence rate in PA programs was 69%.
Discussion: PA is efficacious in improving HRQoL and alleviating anxiety in those with quiescent or mildly active IBD. However, more RCTs are required to precisely estimate the magnitude of effect and make more definitive conclusions about the efficacy of PA as an adjunct therapy for adults with IBD.

Figure: Sub-Group Analysis HRQoL
Disclosures:
Banke Oketola indicated no relevant financial relationships.
Olayinka Akinrolie indicated no relevant financial relationships.
Sandra Webber indicated no relevant financial relationships.
Harminder Singh: Amgen Canada – Advisor or Review Panel Member. Bristol-Myers Squibb Canada – Advisor or Review Panel Member, Advisory Committee/Board Member, Consultant. Ferring Canada – Advisor or Review Panel Member. Guardant Health, Inc – Advisor or Review Panel Member, Advisory Committee/Board Member, Consultant. Pendopharm – Advisor or Review Panel Member. Roche Canada – Advisor or Review Panel Member. Sandoz Canada – Advisor or Review Panel Member. Takeda Canada – Advisory Committee/Board Member.
Nicole Askin indicated no relevant financial relationships.
Rasheda Rabbani indicated no relevant financial relationships.
Ahmed Abou-Setta indicated no relevant financial relationships.
Banke Oketola, MSc1, Olayinka Akinrolie, MSc1, Sandra Webber, PhD2, Harminder Singh, MD, MPH3, Nicole Askin, MLIS4, Rasheda Rabbani, MSc, PhD5, Ahmed Abou-Setta, MD, PhD3. B0353 - Physical Activity as an Adjunct Therapy in Quiescent and Mildly Active Inflammatory Bowel Disease: A Systematic Review and Meta-Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
