Back

Poster Session B - Monday Morning
Category: IBD
B0354 - Racial and Ethnic Disparities in Hospitalizations and Emergency Department Use of Persons With Inflammatory Bowel Disease: A Systematic Review and Meta-Analysis
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- PT
Parul Tandon, DO
Mount Sinai Hospital
Toronto, ON, Canada
Presenting Author(s)
Parul Tandon, DO1, Tarun Chhibba, MD1, Navneet Natt, MD1, Gurmun Singh Brar, MD1, Gurpreet Malhi, MD2, Geoffrey Nguyen, MD, PhD3
1Mount Sinai Hospital, Toronto, ON, Canada; 2Western University, Toronto, ON, Canada; 3University of Toronto, Toronto, ON, Canada
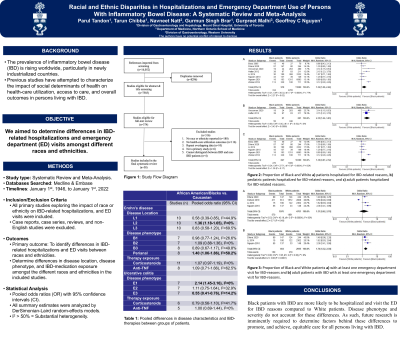
Introduction: The prevalence of inflammatory bowel disease (IBD) is rising worldwide though it remains unknown how race or ethnicity influences IBD-related healthcare utilization. We aimed to determine potential differences in IBD-related hospitalizations and emergency department (ED) visits amongst different races and ethnicities.
Methods: Electronic databases (Medline and Embase) were searched through December 20th, 2021. All studies reporting IBD-related hospitalizations, readmission after discharge, and ED visits by race or ethnicity were included. Differences in IBD location, phenotype, and treatment between races and ethnicities were assessed. Effect estimates were reported as odds ratios (OR) with 95% confidence intervals (CI). Where applicable, subgroup analysis restricting patient age (pediatric vs. adult) was performed. Heterogeneity was assessed using the I2 statistic, with >50% suggesting significant heterogeneity.
Results: Twenty-three observational studies assessed the influence of race and ethnicity on IBD-related hospitalizations and 7 studies on ED visits. Compared to White patients, the likelihood of IBD-related hospitalization was higher in Black (OR 1.54, 95% CI, 1.06-2.24, I2=77.0%) and Hispanic (OR 1.38, 95% CI, 1.01-1.88, I2=37.0%) but not Asian (OR 0.34, 95% CI, 0.02-7.40, I2=95.0%) or South Asian (OR 1.09, 95% CI, 0.47-2.53, I2=60.0%) patients. Furthermore, Black patients had a higher likelihood of readmission to the hospital up to 12 months after discharge compared to White patients (OR 1.41, 95% CI, 1.09-1.82, I2=41.0%). Black adult, but not pediatric, patients had greater odds of IBD-related ED visits compared to adult White patients (OR 1.74, 95% CI, 1.32-2.30, I2=0%). Compared to White patients, Black patients were less likely to have ileal disease, more likely to have perianal disease, and have similar likelihood of receiving biologic therapy. No differences in disease phenotype or therapy exposure were observed between other races.
Discussion: Black patients with IBD are more likely to be hospitalized, readmitted within 12 months, and visit the ED for IBD reasons compared to White patients. Disease phenotype and severity do not account for these differences. As such, future research is imminently required to determine factors behind these differences to promote, and achieve, equitable care for all persons living with IBD.
Disclosures:
Parul Tandon, DO1, Tarun Chhibba, MD1, Navneet Natt, MD1, Gurmun Singh Brar, MD1, Gurpreet Malhi, MD2, Geoffrey Nguyen, MD, PhD3. B0354 - Racial and Ethnic Disparities in Hospitalizations and Emergency Department Use of Persons With Inflammatory Bowel Disease: A Systematic Review and Meta-Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Mount Sinai Hospital, Toronto, ON, Canada; 2Western University, Toronto, ON, Canada; 3University of Toronto, Toronto, ON, Canada
Introduction: The prevalence of inflammatory bowel disease (IBD) is rising worldwide though it remains unknown how race or ethnicity influences IBD-related healthcare utilization. We aimed to determine potential differences in IBD-related hospitalizations and emergency department (ED) visits amongst different races and ethnicities.
Methods: Electronic databases (Medline and Embase) were searched through December 20th, 2021. All studies reporting IBD-related hospitalizations, readmission after discharge, and ED visits by race or ethnicity were included. Differences in IBD location, phenotype, and treatment between races and ethnicities were assessed. Effect estimates were reported as odds ratios (OR) with 95% confidence intervals (CI). Where applicable, subgroup analysis restricting patient age (pediatric vs. adult) was performed. Heterogeneity was assessed using the I2 statistic, with >50% suggesting significant heterogeneity.
Results: Twenty-three observational studies assessed the influence of race and ethnicity on IBD-related hospitalizations and 7 studies on ED visits. Compared to White patients, the likelihood of IBD-related hospitalization was higher in Black (OR 1.54, 95% CI, 1.06-2.24, I2=77.0%) and Hispanic (OR 1.38, 95% CI, 1.01-1.88, I2=37.0%) but not Asian (OR 0.34, 95% CI, 0.02-7.40, I2=95.0%) or South Asian (OR 1.09, 95% CI, 0.47-2.53, I2=60.0%) patients. Furthermore, Black patients had a higher likelihood of readmission to the hospital up to 12 months after discharge compared to White patients (OR 1.41, 95% CI, 1.09-1.82, I2=41.0%). Black adult, but not pediatric, patients had greater odds of IBD-related ED visits compared to adult White patients (OR 1.74, 95% CI, 1.32-2.30, I2=0%). Compared to White patients, Black patients were less likely to have ileal disease, more likely to have perianal disease, and have similar likelihood of receiving biologic therapy. No differences in disease phenotype or therapy exposure were observed between other races.
Discussion: Black patients with IBD are more likely to be hospitalized, readmitted within 12 months, and visit the ED for IBD reasons compared to White patients. Disease phenotype and severity do not account for these differences. As such, future research is imminently required to determine factors behind these differences to promote, and achieve, equitable care for all persons living with IBD.
Disclosures:
Parul Tandon indicated no relevant financial relationships.
Tarun Chhibba indicated no relevant financial relationships.
Navneet Natt indicated no relevant financial relationships.
Gurmun Singh Brar indicated no relevant financial relationships.
Gurpreet Malhi indicated no relevant financial relationships.
Geoffrey Nguyen indicated no relevant financial relationships.
Parul Tandon, DO1, Tarun Chhibba, MD1, Navneet Natt, MD1, Gurmun Singh Brar, MD1, Gurpreet Malhi, MD2, Geoffrey Nguyen, MD, PhD3. B0354 - Racial and Ethnic Disparities in Hospitalizations and Emergency Department Use of Persons With Inflammatory Bowel Disease: A Systematic Review and Meta-Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
