Back

Poster Session B - Monday Morning
Category: IBD
B0357 - Experiences With Bowel Preparation for Colonoscopy in Crohn’s Disease
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- JM
Jennifer K. Maratt, MD, MS
Indiana University School of Medicine
Indianapolis, IN
Presenting Author(s)
Jennifer K. Maratt, MD, MS1, Michael K. Allio, 2, Joshua R. Korzenik, MD3, Douglas K. Rex, MD, MACG1, Kelly Smith, 1, Melissa Thomas, BS4, Laura Barger, MSN, FNP5, Ziad H. Younes, MD5, Corey A. Siegel, MD, MS6
1Indiana University School of Medicine, Indianapolis, IN; 2ColonaryConcepts, LLC, Providence, RI; 3Brigham and Women's Hospital, Boston, MA; 4Indiana University Purdue University Indianapolis, Indianapolis, IN; 5Gastro One, Germantown, TN; 6Dartmouth-Hitchcock Medical Center, Lebanon, NH
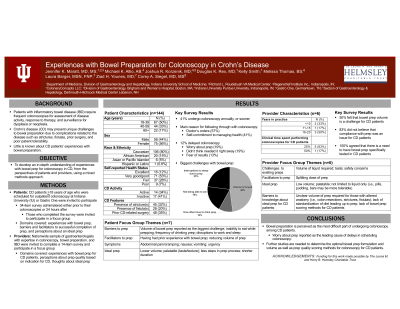
Introduction: Patients with inflammatory bowel disease (IBD) require frequent colonoscopies. Crohn’s disease (CD) may present unique challenges to bowel prep for colonoscopy due to the presence of strictures, fistulas, or prior bowel resections. Little is known about CD patients’ experiences with bowel preps. The purpose of this study was to develop an in-depth understanding of experiences with bowel prep for colonoscopy in CD, from the perspectives of patients and providers.
Methods: We used a mixed methods approach, inviting CD patients ≥ 18 years of age scheduled for outpatient colonoscopy at two medical centers between July 2021-January 2022, and gastroenterologists, to participate in a survey and focus groups. Domains that were covered included experiences with existing bowel preps, including barriers to tolerance, and perceptions about ideal preps.
Results: A total of 144 patients completed the survey and 7 participated in focus groups, with 50% between 18-39 years of age, 56% female, 80% Caucasian, and 65% reporting good/excellent health status. CD phenotypes included 32% with strictures, 20% with fistulas, 35% with prior bowel surgeries, and 34% with active disease. Reported challenges to bowel preps included the inability to eat, volume of liquid required, and disruptions to work and sleep. Ideal preps were described as lower volume, more palatable, and without the need to fast. Worry about the prep was one of the leading reasons that patients delayed their colonoscopies. Despite these challenges, 91% of patients would undergo colonoscopy again if recommended by their physician. Six gastroenterologists participated in the study. Volume, taste, and safety concerns were reported as limitations to currently-available preps. All agreed that, if available, they would favor a prep that was tested in CD patients. Barriers to optimizing colonoscopy bowel prep for CD patients included limited knowledge about ideal volume required, lack of standardization of dietary modifications, and lack of bowel prep quality scoring methods.
Discussion: Bowel preparation is perceived as the most difficult part of undergoing colonoscopy among CD patients with worry about the prep as one of the leading causes of delaying colonoscopies. Given that CD patients may have altered anatomy due to their disease phenotypes and require frequent colonoscopies, future studies are needed to determine the optimal prep formulation, volume, and prep quality scoring methods for patients with CD.
Disclosures:
Jennifer K. Maratt, MD, MS1, Michael K. Allio, 2, Joshua R. Korzenik, MD3, Douglas K. Rex, MD, MACG1, Kelly Smith, 1, Melissa Thomas, BS4, Laura Barger, MSN, FNP5, Ziad H. Younes, MD5, Corey A. Siegel, MD, MS6. B0357 - Experiences With Bowel Preparation for Colonoscopy in Crohn’s Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Indiana University School of Medicine, Indianapolis, IN; 2ColonaryConcepts, LLC, Providence, RI; 3Brigham and Women's Hospital, Boston, MA; 4Indiana University Purdue University Indianapolis, Indianapolis, IN; 5Gastro One, Germantown, TN; 6Dartmouth-Hitchcock Medical Center, Lebanon, NH
Introduction: Patients with inflammatory bowel disease (IBD) require frequent colonoscopies. Crohn’s disease (CD) may present unique challenges to bowel prep for colonoscopy due to the presence of strictures, fistulas, or prior bowel resections. Little is known about CD patients’ experiences with bowel preps. The purpose of this study was to develop an in-depth understanding of experiences with bowel prep for colonoscopy in CD, from the perspectives of patients and providers.
Methods: We used a mixed methods approach, inviting CD patients ≥ 18 years of age scheduled for outpatient colonoscopy at two medical centers between July 2021-January 2022, and gastroenterologists, to participate in a survey and focus groups. Domains that were covered included experiences with existing bowel preps, including barriers to tolerance, and perceptions about ideal preps.
Results: A total of 144 patients completed the survey and 7 participated in focus groups, with 50% between 18-39 years of age, 56% female, 80% Caucasian, and 65% reporting good/excellent health status. CD phenotypes included 32% with strictures, 20% with fistulas, 35% with prior bowel surgeries, and 34% with active disease. Reported challenges to bowel preps included the inability to eat, volume of liquid required, and disruptions to work and sleep. Ideal preps were described as lower volume, more palatable, and without the need to fast. Worry about the prep was one of the leading reasons that patients delayed their colonoscopies. Despite these challenges, 91% of patients would undergo colonoscopy again if recommended by their physician. Six gastroenterologists participated in the study. Volume, taste, and safety concerns were reported as limitations to currently-available preps. All agreed that, if available, they would favor a prep that was tested in CD patients. Barriers to optimizing colonoscopy bowel prep for CD patients included limited knowledge about ideal volume required, lack of standardization of dietary modifications, and lack of bowel prep quality scoring methods.
Discussion: Bowel preparation is perceived as the most difficult part of undergoing colonoscopy among CD patients with worry about the prep as one of the leading causes of delaying colonoscopies. Given that CD patients may have altered anatomy due to their disease phenotypes and require frequent colonoscopies, future studies are needed to determine the optimal prep formulation, volume, and prep quality scoring methods for patients with CD.
Disclosures:
Jennifer Maratt indicated no relevant financial relationships.
Michael Allio: ColonaryConcepts, LLC – Advisor or Review Panel Member, Intellectual Property/Patents, Owner/Ownership Interest.
Joshua Korzenik: Bilayer Therapeutics – Intellectual Property/Patents, Owner/Ownership Interest. ClostraBio – Advisor or Review Panel Member. ColonaryConcepts – Intellectual Property/Patents. Pfizer – Grant/Research Support. Promakhos – Advisor or Review Panel Member. Steritas – Advisor or Review Panel Member.
Douglas Rex: Acacia Pharmaceuticals – Consultant. Aries Pharmaceutical – Consultant. Boston Scientific – Consultant. Braintree Laboratories – Consultant, Grant/Research Support. EndoAId – Grant/Research Support. Endokey – Consultant. Erbe USA – Grant/Research Support. GI Supply – Consultant. Lumendi, Ltd – Consultant. Medivators – Grant/Research Support. Medtronic – Consultant. Norgine – Consultant. Olympus Corporation – Consultant, Grant/Research Support. Satisfai Health – Stock Options.
Kelly Smith indicated no relevant financial relationships.
Melissa Thomas indicated no relevant financial relationships.
Laura Barger: Janssen – Consultant.
Ziad Younes: Colonary Concepts – Stock-privately held company.
Corey Siegel: Abbvie – Consultant, Grant/Research Support. Jannsen – Consultant. Lilly – Consultant, Grant/Research Support. MiTest Health, LLC – Intellectual Property/Patents, Owner/Ownership Interest. Napo Pharmaceuticals – Consultant. Pfizer – Advisor or Review Panel Member, Consultant, Grant/Research Support. Prometheus – Consultant. Prometheus Biosciences – Consultant. Takeda – Advisor or Review Panel Member, Grant/Research Support, Royalties.
Jennifer K. Maratt, MD, MS1, Michael K. Allio, 2, Joshua R. Korzenik, MD3, Douglas K. Rex, MD, MACG1, Kelly Smith, 1, Melissa Thomas, BS4, Laura Barger, MSN, FNP5, Ziad H. Younes, MD5, Corey A. Siegel, MD, MS6. B0357 - Experiences With Bowel Preparation for Colonoscopy in Crohn’s Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
