Back

Poster Session B - Monday Morning
Category: IBD
B0379 - Active Tuberculosis and Opportunistic Infections: Pooled Safety Analysis of Ustekinumab Through up to 5 Years Across All Approved Indications
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- EL
Edward V. Loftus, Jr., MD, FACG
Mayo Clinic College of Medicine and Science
Rochester, Minnesota
Presenting Author(s)
Edward V. Loftus, MD, FACG1, Millie Long, MD, MPH, FACG2, Elyssa Ott, MPH3, Christopher Gasink, MD3, Thomas Baker, MD4, Bridget Goodwin, MD3, Ye Miao, MS4, Subrata Ghosh, MD5
1Mayo Clinic College of Medicine and Science, Rochester, MN; 2UNC Chapel Hill, Chapel Hill, NC; 3Janssen Scientific Affairs, LLC, Horsham, PA; 4Janssen Research & Development, LLC, Spring House, PA; 5College of Medicine and Health, University College, Cork, Cork, Ireland
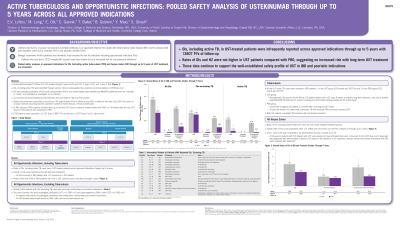
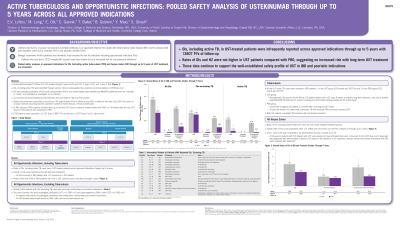
Introduction: Ustekinumab (UST) is an approved treatment for adults with inflammatory bowel disease (IBD: Crohn’s disease [CD] and ulcerative colitis [UC]), psoriasis (PsO), and psoriatic arthritis (PsA). Here, we present pooled safety analyses in these approved indications of patients (pts) with active tuberculosis (TB) and opportunistic infections (OIs) through 5 years (yrs) of UST treatment.
Methods: Pooled data included 13 Phase 2/3 UST studies through 5 yrs of CD and PsO, 2 yrs of UC, and 1 yr of PsA. OIs were identified by clinician review. Herpes zoster (HZ) was evaluated separately. Event rates per 100 pt yrs (PYs) are presented. Concomitant immunomodulators/corticosteroids were permitted in IBD and PsA pts. All pts who received ≥1 UST dose were included. In IBD, placebo (PBO) pts included data up to the first UST dose for pts initially treated with PBO, or >16 weeks after the last UST dose for UST pts who switched to PBO.
Results: Across all approved indications, 19 OIs including TB were reported, with rates in PBO of 0.40 and UST of 0.10 through 5 yrs in 13807 PYs of follow-up (Table 1); rates of HZ were 1.21 and 0.63, respectively. Of 19 OIs, 18 were in IBD pts and 1 in a PsO pt. Overall, 14/16 pts (12/13 UST) with OIs excluding TB were also receiving confounding concomitant medications. A total of 3 active TB cases (2 pts with CD and 1 pt with UC) were reported in PBO (n=2; 1 in a CD pt 10 months after receiving UST 130 mg IV) and UST pts (n=1) (Table 1). One active TB case was reported in an asymptomatic South African CD pt treated with UST who had a positive QuantiFERON®-TB Gold test on routine screening and bronchial brushings positive for M. tuberculosis. Both CD pts completed TB treatment with disease resolution. The most common OIs were esophageal candidiasis (UST n=3; PBO n=2) and cytomegalovirus colitis (UST n=3; PBO n=1).
Discussion: Rates of OIs, including active TB, in UST-treated pts were low across approved indications through up to 5 years with 13807 PYs of follow-up and not higher in UST pts vs PBO, suggesting no increased risk of OI with long-term UST treatment.
Disclosures:
Edward V. Loftus, MD, FACG1, Millie Long, MD, MPH, FACG2, Elyssa Ott, MPH3, Christopher Gasink, MD3, Thomas Baker, MD4, Bridget Goodwin, MD3, Ye Miao, MS4, Subrata Ghosh, MD5. B0379 - Active Tuberculosis and Opportunistic Infections: Pooled Safety Analysis of Ustekinumab Through up to 5 Years Across All Approved Indications, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Mayo Clinic College of Medicine and Science, Rochester, MN; 2UNC Chapel Hill, Chapel Hill, NC; 3Janssen Scientific Affairs, LLC, Horsham, PA; 4Janssen Research & Development, LLC, Spring House, PA; 5College of Medicine and Health, University College, Cork, Cork, Ireland
Introduction: Ustekinumab (UST) is an approved treatment for adults with inflammatory bowel disease (IBD: Crohn’s disease [CD] and ulcerative colitis [UC]), psoriasis (PsO), and psoriatic arthritis (PsA). Here, we present pooled safety analyses in these approved indications of patients (pts) with active tuberculosis (TB) and opportunistic infections (OIs) through 5 years (yrs) of UST treatment.
Methods: Pooled data included 13 Phase 2/3 UST studies through 5 yrs of CD and PsO, 2 yrs of UC, and 1 yr of PsA. OIs were identified by clinician review. Herpes zoster (HZ) was evaluated separately. Event rates per 100 pt yrs (PYs) are presented. Concomitant immunomodulators/corticosteroids were permitted in IBD and PsA pts. All pts who received ≥1 UST dose were included. In IBD, placebo (PBO) pts included data up to the first UST dose for pts initially treated with PBO, or >16 weeks after the last UST dose for UST pts who switched to PBO.
Results: Across all approved indications, 19 OIs including TB were reported, with rates in PBO of 0.40 and UST of 0.10 through 5 yrs in 13807 PYs of follow-up (Table 1); rates of HZ were 1.21 and 0.63, respectively. Of 19 OIs, 18 were in IBD pts and 1 in a PsO pt. Overall, 14/16 pts (12/13 UST) with OIs excluding TB were also receiving confounding concomitant medications. A total of 3 active TB cases (2 pts with CD and 1 pt with UC) were reported in PBO (n=2; 1 in a CD pt 10 months after receiving UST 130 mg IV) and UST pts (n=1) (Table 1). One active TB case was reported in an asymptomatic South African CD pt treated with UST who had a positive QuantiFERON®-TB Gold test on routine screening and bronchial brushings positive for M. tuberculosis. Both CD pts completed TB treatment with disease resolution. The most common OIs were esophageal candidiasis (UST n=3; PBO n=2) and cytomegalovirus colitis (UST n=3; PBO n=1).
Discussion: Rates of OIs, including active TB, in UST-treated pts were low across approved indications through up to 5 years with 13807 PYs of follow-up and not higher in UST pts vs PBO, suggesting no increased risk of OI with long-term UST treatment.
Table: Table 1. Opportunistic infections (OIs) and active tuberculosis (TB) in Inflammatory Bowel Disease (CD, UC) and Psoriatic studies (PsO, PsA) through up to 5 yrs; numbers of events per 100 patient-years (PYs) of follow-up
Disclosures:
Edward Loftus: AbbVie – Consultant, Grant/Research Support. Amgen – Consultant, Grant/Research Support. Arena Pharmaceuticals – Consultant. Boehringer Ingelheim – Consultant. Bristol-Myers Squibb – Consultant, Grant/Research Support. Calibr – Consultant. Celgene – Consultant, Grant/Research Support. Eli Lilly – Consultant. Genentech – Consultant, Grant/Research Support. Gilead – Consultant, Grant/Research Support. Iterative Scopes – Consultant. Janssen – Consultant, Grant/Research Support. Morphic – Consultant. Ono Pharma – Consultant. Pfizer – Consultant, Grant/Research Support. Protagonist – Consultant. Receptos – Grant/Research Support. Robarts Clinical Trials – Grant/Research Support. Scipher Medicine – Consultant. Sun Pharma – Consultant. Surrozen – Consultant. Takeda – Consultant, Grant/Research Support. Theravance – Grant/Research Support. UCB – Consultant, Grant/Research Support.
Millie Long: AbbVie – Consultant. Bristol Myers Squibb – Consultant. Calibr – Consultant. Eli Lilly – Consultant. Genentech – Consultant. Janssen – Consultant. Pfizer – Consultant, Grant/Research Support. Prometheus – Consultant. Roche – Consultant. Salix – Consultant. Takeda – Consultant, Grant/Research Support. Target RWE – Consultant. Theravance – Consultant.
Elyssa Ott: Janssen – Employee, Stock-publicly held company(excluding mutual/index funds).
Christopher Gasink: Janssen – Employee, Stock-publicly held company(excluding mutual/index funds).
Thomas Baker: Janssen – Employee, Stock-publicly held company(excluding mutual/index funds).
Bridget Goodwin: Janssen Pharmaceutical Companies of Johnson and Johnson – Employee, Stock-publicly held company(excluding mutual/index funds).
Ye Miao: Janssen Research & Development, LLC – Employee, Stock-publicly held company(excluding mutual/index funds).
Subrata Ghosh: AbbVie – Advisory Committee/Board Member, steering committee, Speakers Bureau. Boehringer Ingelheim – steering committee. Bristol Myers Squibb – steering committee. Celgene – steering committee. Celltrion – Speakers Bureau. Eli Lilly – Advisory Committee/Board Member. Ferring – Speakers Bureau. Gilead – Advisory Committee/Board Member, steering committee. Janssen – Advisory Committee/Board Member, steering committee, Speakers Bureau. Pfizer – Advisory Committee/Board Member, Speakers Bureau. Roche – Advisory Committee/Board Member. Takeda – Advisory Committee/Board Member, Speakers Bureau.
Edward V. Loftus, MD, FACG1, Millie Long, MD, MPH, FACG2, Elyssa Ott, MPH3, Christopher Gasink, MD3, Thomas Baker, MD4, Bridget Goodwin, MD3, Ye Miao, MS4, Subrata Ghosh, MD5. B0379 - Active Tuberculosis and Opportunistic Infections: Pooled Safety Analysis of Ustekinumab Through up to 5 Years Across All Approved Indications, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
