Back

Poster Session B - Monday Morning
Category: Biliary/Pancreas
B0047 - Vasoactive Intestinal Peptide Tumors (VIPoma) Missed on CT but EUS to the Rescue
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- JO
Julie J. Oh, MD
University of California Irvine
Orange, CA
Presenting Author(s)
Julie J. Oh, MD1, Sagar Shah, MD2, Neil R. Jariwalla, MD1, Amirali Tavangar, MD1, Jason Samarasena, MD, MBA, FACG3
1University of California Irvine, Orange, CA; 2UCLA, Orange, CA; 3UC Irvine, Orange, CA
Introduction: Pancreatic neuroendocrine tumors (pNETs) are rare with >85% being non-functional. Amongst the functioning pNETs, vasoactive intestinal peptide tumors (VIPoma) account for < 2% pNETs. VIPoma secretes unregulated vasoactive intestinal peptide (VIP) hormones that can cause secretory diarrhea with electrolyte abnormalities with incidence rate of 0.05% to 2.0%. VIPoma are usually diagnosed with elevated serum VIP level. Imaging modalities are utilized to localize the tumor, usually with CT scans. Here we present a case of a diagnosed VIPoma patient with negative initial imaging, but lesions found with endoscopic ultrasound (EUS).
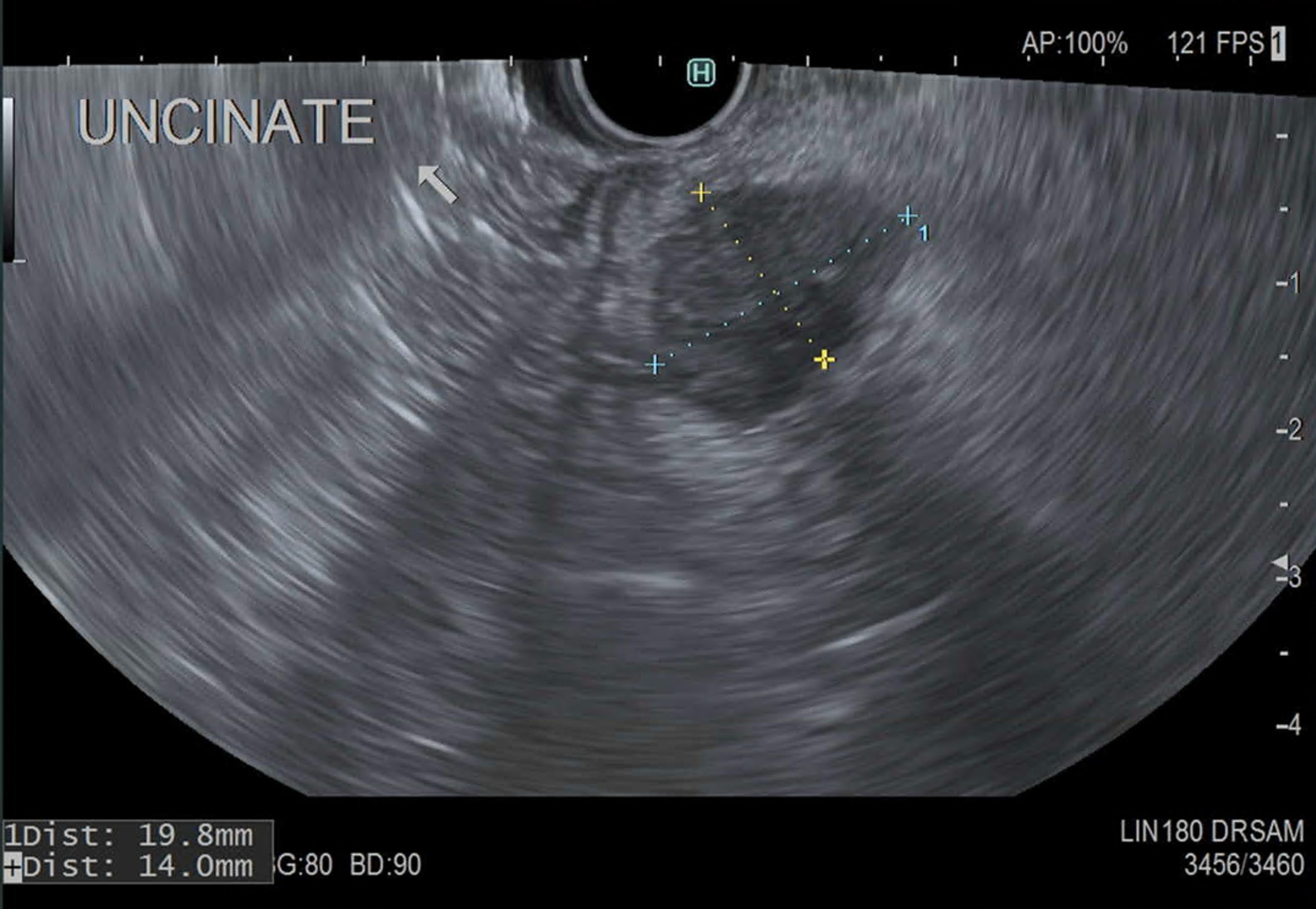
Case Description/Methods: 74year old female who has had recurrent urgent care visits for chronic diarrhea with dehydration for the past year. She was found to have elevated VIP (in the 900s) with hypokalemia and hypercalcemia, but CT abdomen and pelvis with IV contrast was negative for any lesions in the pancreas. Given the concern for a VIPoma, an EUS was ordered. EUS demonstrated a 19.8mm x 14.0mm hypoechoic mass in the uncinate process. Fine needle biopsy (FNB) was performed and revealed a well-differentiated neuroendocrine tumor that was WHO grade 1. Following diagnosis, the patient was started on octreotide for symptomatic management with further workup of MEN1. The patient showed hepatic lesion concerning metastasis on follow up MRI of abdomen. Repeat EUS with FNA of hepatic lesion showed pathology result suggestive of metastasis.
Discussion: CT is used as primary method to localize the lesion, given that it is readily available and takes shorter time to obtain imaging. Though one study reported sensitivity of CT being >80%, another study reported CT sensitivity of 58%. As also demonstrated in this case, it can be a challenge to localize VIPoma with a single imaging test, and may require multi-modality approach, including CT, MRI, PET, and EUS. Modality used in our study, EUS, has shown detection rate of approximately 90%. To demonstrate this, EUS was able to detect lesions in 33% of the patients that tested negative on initial CT. It is important to keep in mind that VIP levels may be false negative given that VIPoma may secrete VIP intermittently. This case and literature review implore that in the setting of clinical suspicion with or without VIP elevation, even if CT is negative, it does not necessarily rule out VIPoma and further imaging should still be considered.
Disclosures:
Julie J. Oh, MD1, Sagar Shah, MD2, Neil R. Jariwalla, MD1, Amirali Tavangar, MD1, Jason Samarasena, MD, MBA, FACG3. B0047 - Vasoactive Intestinal Peptide Tumors (VIPoma) Missed on CT but EUS to the Rescue, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of California Irvine, Orange, CA; 2UCLA, Orange, CA; 3UC Irvine, Orange, CA
Introduction: Pancreatic neuroendocrine tumors (pNETs) are rare with >85% being non-functional. Amongst the functioning pNETs, vasoactive intestinal peptide tumors (VIPoma) account for < 2% pNETs. VIPoma secretes unregulated vasoactive intestinal peptide (VIP) hormones that can cause secretory diarrhea with electrolyte abnormalities with incidence rate of 0.05% to 2.0%. VIPoma are usually diagnosed with elevated serum VIP level. Imaging modalities are utilized to localize the tumor, usually with CT scans. Here we present a case of a diagnosed VIPoma patient with negative initial imaging, but lesions found with endoscopic ultrasound (EUS).
Case Description/Methods: 74year old female who has had recurrent urgent care visits for chronic diarrhea with dehydration for the past year. She was found to have elevated VIP (in the 900s) with hypokalemia and hypercalcemia, but CT abdomen and pelvis with IV contrast was negative for any lesions in the pancreas. Given the concern for a VIPoma, an EUS was ordered. EUS demonstrated a 19.8mm x 14.0mm hypoechoic mass in the uncinate process. Fine needle biopsy (FNB) was performed and revealed a well-differentiated neuroendocrine tumor that was WHO grade 1. Following diagnosis, the patient was started on octreotide for symptomatic management with further workup of MEN1. The patient showed hepatic lesion concerning metastasis on follow up MRI of abdomen. Repeat EUS with FNA of hepatic lesion showed pathology result suggestive of metastasis.
Discussion: CT is used as primary method to localize the lesion, given that it is readily available and takes shorter time to obtain imaging. Though one study reported sensitivity of CT being >80%, another study reported CT sensitivity of 58%. As also demonstrated in this case, it can be a challenge to localize VIPoma with a single imaging test, and may require multi-modality approach, including CT, MRI, PET, and EUS. Modality used in our study, EUS, has shown detection rate of approximately 90%. To demonstrate this, EUS was able to detect lesions in 33% of the patients that tested negative on initial CT. It is important to keep in mind that VIP levels may be false negative given that VIPoma may secrete VIP intermittently. This case and literature review implore that in the setting of clinical suspicion with or without VIP elevation, even if CT is negative, it does not necessarily rule out VIPoma and further imaging should still be considered.
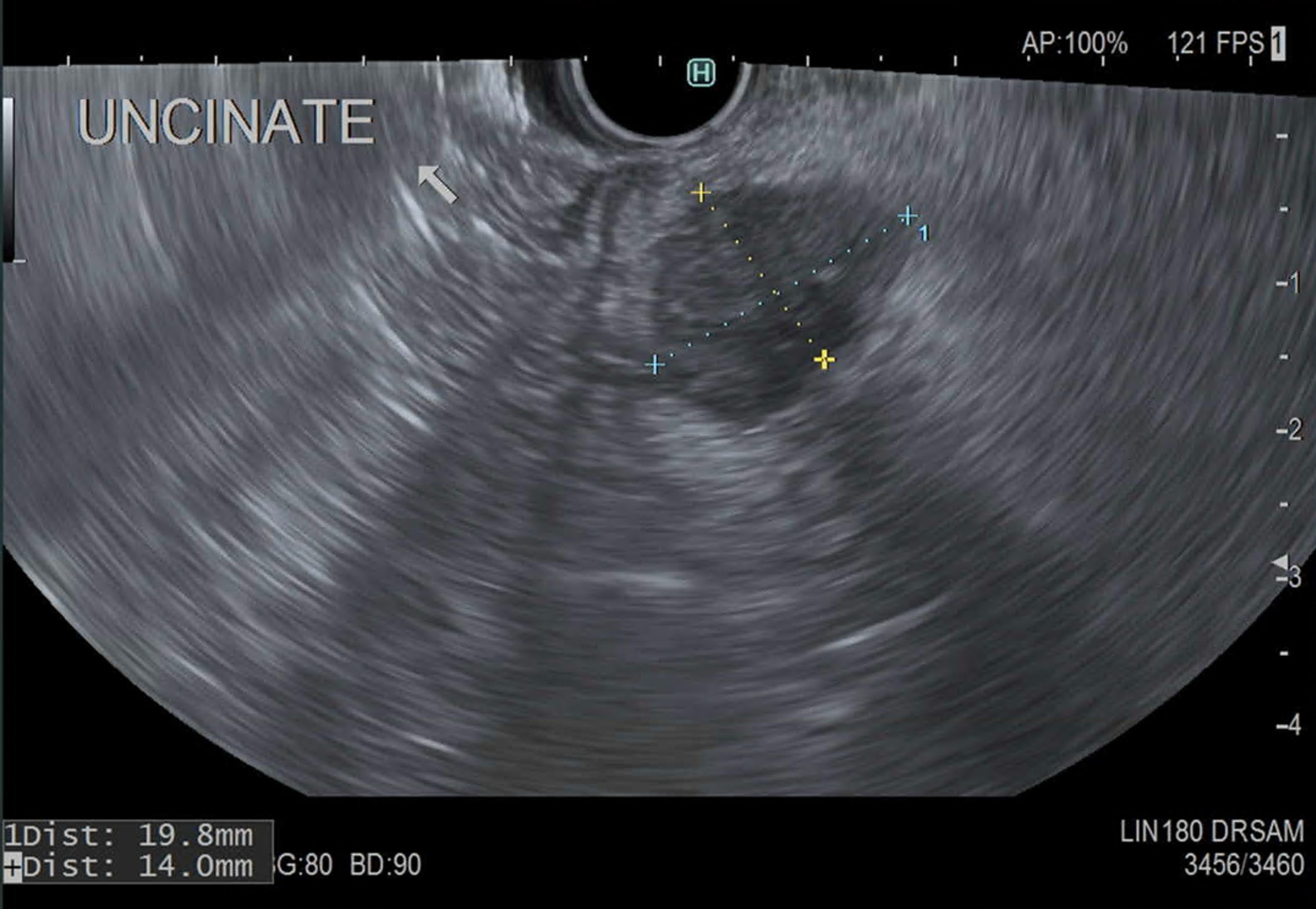
Figure: EUS showing uncinate mass
Disclosures:
Julie Oh indicated no relevant financial relationships.
Sagar Shah indicated no relevant financial relationships.
Neil Jariwalla indicated no relevant financial relationships.
Amirali Tavangar indicated no relevant financial relationships.
Jason Samarasena: Conmed – Consultant. Docbot – Stock Options. Mauna Kea – Consultant. Olympus – Consultant. Ovesco – Consultant. Steris – Consultant.
Julie J. Oh, MD1, Sagar Shah, MD2, Neil R. Jariwalla, MD1, Amirali Tavangar, MD1, Jason Samarasena, MD, MBA, FACG3. B0047 - Vasoactive Intestinal Peptide Tumors (VIPoma) Missed on CT but EUS to the Rescue, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
