Back

Poster Session B - Monday Morning
Category: Colon
B0147 - Colonoscopy-Associated Tension Pneumoperitoneum After Endoscopic Submucosal Dissection (ESD)
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- JO
Julie J. Oh, MD
University of California Irvine
Orange, CA
Presenting Author(s)
Julie J. Oh, MD1, Sagar Shah, MD2, Neil R. Jariwalla, MD1, Amirali Tavangar, MD1, James Han, MD3, Jason Samarasena, MD, MBA, FACG1
1University of California Irvine, Orange, CA; 2UCLA, Orange, CA; 3UC Irvine, Orange, CA
Introduction: Colonoscopy is a low-risk procedure with complications including bleeding or perforation. Although rare, perforation can result in tension pneumoperitoneum, which can be fatal. There is little guidance for the management of this potentially fatal complication. Here we present a case of an ESD complicated by tension pneumoperitoneum treated with needle decompression.
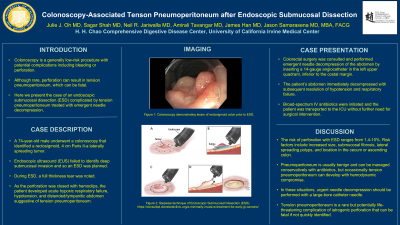
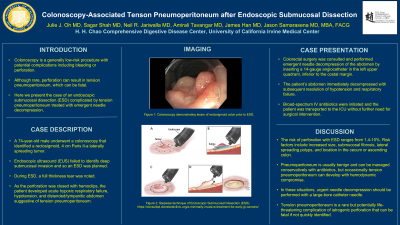
Case Description/Methods: A 74 year old male underwent a colonoscopy that identified a rectosigmoid 4 cm Paris II-a laterally spreading tumor. EUS failed to identify deep submucosal invasion and endoscopic mucosal dissection (ESD) was planned. During ESD, a full thickness tear was noted. As the perforation was closed with hemoclips, the patient developed hypoxic respiratory failure, hypotension, and distended/tympanic abdomen, suggesting of tension pneumoperitoneum. Colorectal surgery team was consulted and performed needle decompression of the abdomen by inserting a 14 gauge angiocatheter in the left upper quadrant, inferior to the costal margin. The patient’s abdomen immediately decompressed and his hypoxia and blood pressure stabilized. Broad spectrum IV antibiotics was started and patient was admitted to the ICU without requiring further surgical interventions.
Discussion: Perforation risk from ESD ranges from 1.4% to 10%. Risk factors for perforation include increased size, submucosal fibrosis, lateral spreading polyps, and location in cecum or ascending colon. Pneumoperitoneum is usually benign and can be managed conservatively with antibiotics. However, rarely tension pneumoperitoneum occurs, where excessive pressure builds in the peritoneal space. This can compress the inferior vena cava and diaphragm, leading to lowered cardiac output and reduced lung volumes.
If there is evidence of hemodynamic instability, immediate needle decompression should be performed. A large bore catheter needle should be inserted either 2cm below umbilicus or 5cm superior and medial to the anterior superior iliac spines, preferably the left side. Angiocatheters are ideal because they can puncture sharp but when the needle is removed the plastic catheter is unlikely to cause injury. Successful placement should lead to expulsion of air and improvement of hemodynamics.
Tension pneumothorax is a rare complication that results from iatrogenic perforation and can be fatal if not quickly identified. Needle decompression is a skill that gastroenterologists should be familiar with because it can be life saving.
Disclosures:
Julie J. Oh, MD1, Sagar Shah, MD2, Neil R. Jariwalla, MD1, Amirali Tavangar, MD1, James Han, MD3, Jason Samarasena, MD, MBA, FACG1. B0147 - Colonoscopy-Associated Tension Pneumoperitoneum After Endoscopic Submucosal Dissection (ESD), ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of California Irvine, Orange, CA; 2UCLA, Orange, CA; 3UC Irvine, Orange, CA
Introduction: Colonoscopy is a low-risk procedure with complications including bleeding or perforation. Although rare, perforation can result in tension pneumoperitoneum, which can be fatal. There is little guidance for the management of this potentially fatal complication. Here we present a case of an ESD complicated by tension pneumoperitoneum treated with needle decompression.
Case Description/Methods: A 74 year old male underwent a colonoscopy that identified a rectosigmoid 4 cm Paris II-a laterally spreading tumor. EUS failed to identify deep submucosal invasion and endoscopic mucosal dissection (ESD) was planned. During ESD, a full thickness tear was noted. As the perforation was closed with hemoclips, the patient developed hypoxic respiratory failure, hypotension, and distended/tympanic abdomen, suggesting of tension pneumoperitoneum. Colorectal surgery team was consulted and performed needle decompression of the abdomen by inserting a 14 gauge angiocatheter in the left upper quadrant, inferior to the costal margin. The patient’s abdomen immediately decompressed and his hypoxia and blood pressure stabilized. Broad spectrum IV antibiotics was started and patient was admitted to the ICU without requiring further surgical interventions.
Discussion: Perforation risk from ESD ranges from 1.4% to 10%. Risk factors for perforation include increased size, submucosal fibrosis, lateral spreading polyps, and location in cecum or ascending colon. Pneumoperitoneum is usually benign and can be managed conservatively with antibiotics. However, rarely tension pneumoperitoneum occurs, where excessive pressure builds in the peritoneal space. This can compress the inferior vena cava and diaphragm, leading to lowered cardiac output and reduced lung volumes.
If there is evidence of hemodynamic instability, immediate needle decompression should be performed. A large bore catheter needle should be inserted either 2cm below umbilicus or 5cm superior and medial to the anterior superior iliac spines, preferably the left side. Angiocatheters are ideal because they can puncture sharp but when the needle is removed the plastic catheter is unlikely to cause injury. Successful placement should lead to expulsion of air and improvement of hemodynamics.
Tension pneumothorax is a rare complication that results from iatrogenic perforation and can be fatal if not quickly identified. Needle decompression is a skill that gastroenterologists should be familiar with because it can be life saving.
Disclosures:
Julie Oh indicated no relevant financial relationships.
Sagar Shah indicated no relevant financial relationships.
Neil Jariwalla indicated no relevant financial relationships.
Amirali Tavangar indicated no relevant financial relationships.
James Han indicated no relevant financial relationships.
Jason Samarasena: Conmed – Consultant. Docbot – Owner/Ownership Interest. Mauna Kea – Consultant. Medtronic – Consultant. Neptune Medical – Consultant. Olympus – Consultant. Ovesco – Consultant. Steris – Consultant.
Julie J. Oh, MD1, Sagar Shah, MD2, Neil R. Jariwalla, MD1, Amirali Tavangar, MD1, James Han, MD3, Jason Samarasena, MD, MBA, FACG1. B0147 - Colonoscopy-Associated Tension Pneumoperitoneum After Endoscopic Submucosal Dissection (ESD), ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

