Back

Poster Session B - Monday Morning
Category: Interventional Endoscopy
B0447 - Lumen-Apposing Metal Stents for Pancreatic Fluid Collections Reduce 90-Day Readmission Rates
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Jay B. Patel, MD
Temple University Hospital
Philadelphia, PA
Presenting Author(s)
Jay B. Patel, MD1, Rishabh Khatri, MD1, Jay Kanaparthi, MD1, Jun Song, MD1, Stephen Heller, MD2, Woo Jung Jay Lee, MB, BCh, BAO2, Frank Friedenberg, MD, MS2, Saraswathi Cappelle, DO2
1Temple University Hospital, Philadelphia, PA; 2Lewis Katz School of Medicine at Temple University, Philadelphia, PA
Introduction: Management of symptomatic mature pancreatic fluid collections (PFCs) such as pancreatic pseudocysts or walled-off necrosis now involve the use of lumen-apposing metal stents (LAMS) under endoscopic ultrasound (EUS) guidance. LAMS appear to be superior compared to traditional plastic stents however require close follow up. Numerous studies have shown a benefit of LAMS for short-term (e.g., 4-week) outcomes. However, there is a lack of data evaluating longer term outcomes. Our aim was to investigate 90-day readmission rates after LAMS placement over an 8-year period.
Methods: We identified all patients ≥ 18 years who underwent deployment of a LAMS from 01/01/2014 to 06/01/2021 at our urban, safety net hospital. We subsequently collected demographic data, cyst characteristics, and stent information. Follow-up upper endoscopies and imaging were examined to determine stent removal date and assess for complications. Hospital admission rates 90 days before and after stent placement were collected. Admissions were stratified into gastrointestinal (GI)-related or other.
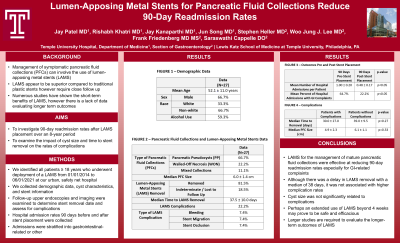
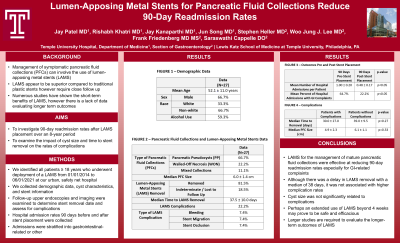
Results: We identified 27 patients who underwent LAMS for drainage of mature PFCs. Of these, 18 were simple pancreatic pseudocysts (PP), 6 walled-off necrosis (WON), and 3 mixed collections. Mean age was 52.1 ± 11.0 years, 66.7% male, 66.7 % non-white, and 59.3% reported alcohol use. The average collection was 6.6 ± 2.0 cm. Stents were removed in 81.5% of patients at a median of 37.5 days. 7.4% were lost to follow up, and 22.2% of patients had stent complications during follow-up: 2 bleeding, 2 stent migration, and 2 stent occlusions. Patients on average had 1.00 ± 0.20 hospital admissions in the 90 days prior to stent placement vs 0.48 ± 0.17 admissions 90 days after placement (mean difference 0.52 ± 0.17, p< 0.05). Of these patients, 64.7% of pre-stent hospitalizations were due to GI complaints vs 22.2% of post-stent hospitalizations (p< 0.05). Neither cyst size nor time to stent removal were significantly related to complications.
Discussion: LAMS for the management of mature pancreatic fluid collections were effective at reducing 90-day readmission rates especially in the setting of GI-related complaints. Although there was a delay in LAMS removal with a median of 38 days, it did not appear to translate into higher complication rates. Perhaps an extended use of LAMS beyond 4 weeks may prove to be safe and efficacious, however larger studies are required.
Disclosures:
Jay B. Patel, MD1, Rishabh Khatri, MD1, Jay Kanaparthi, MD1, Jun Song, MD1, Stephen Heller, MD2, Woo Jung Jay Lee, MB, BCh, BAO2, Frank Friedenberg, MD, MS2, Saraswathi Cappelle, DO2. B0447 - Lumen-Apposing Metal Stents for Pancreatic Fluid Collections Reduce 90-Day Readmission Rates, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Temple University Hospital, Philadelphia, PA; 2Lewis Katz School of Medicine at Temple University, Philadelphia, PA
Introduction: Management of symptomatic mature pancreatic fluid collections (PFCs) such as pancreatic pseudocysts or walled-off necrosis now involve the use of lumen-apposing metal stents (LAMS) under endoscopic ultrasound (EUS) guidance. LAMS appear to be superior compared to traditional plastic stents however require close follow up. Numerous studies have shown a benefit of LAMS for short-term (e.g., 4-week) outcomes. However, there is a lack of data evaluating longer term outcomes. Our aim was to investigate 90-day readmission rates after LAMS placement over an 8-year period.
Methods: We identified all patients ≥ 18 years who underwent deployment of a LAMS from 01/01/2014 to 06/01/2021 at our urban, safety net hospital. We subsequently collected demographic data, cyst characteristics, and stent information. Follow-up upper endoscopies and imaging were examined to determine stent removal date and assess for complications. Hospital admission rates 90 days before and after stent placement were collected. Admissions were stratified into gastrointestinal (GI)-related or other.
Results: We identified 27 patients who underwent LAMS for drainage of mature PFCs. Of these, 18 were simple pancreatic pseudocysts (PP), 6 walled-off necrosis (WON), and 3 mixed collections. Mean age was 52.1 ± 11.0 years, 66.7% male, 66.7 % non-white, and 59.3% reported alcohol use. The average collection was 6.6 ± 2.0 cm. Stents were removed in 81.5% of patients at a median of 37.5 days. 7.4% were lost to follow up, and 22.2% of patients had stent complications during follow-up: 2 bleeding, 2 stent migration, and 2 stent occlusions. Patients on average had 1.00 ± 0.20 hospital admissions in the 90 days prior to stent placement vs 0.48 ± 0.17 admissions 90 days after placement (mean difference 0.52 ± 0.17, p< 0.05). Of these patients, 64.7% of pre-stent hospitalizations were due to GI complaints vs 22.2% of post-stent hospitalizations (p< 0.05). Neither cyst size nor time to stent removal were significantly related to complications.
Discussion: LAMS for the management of mature pancreatic fluid collections were effective at reducing 90-day readmission rates especially in the setting of GI-related complaints. Although there was a delay in LAMS removal with a median of 38 days, it did not appear to translate into higher complication rates. Perhaps an extended use of LAMS beyond 4 weeks may prove to be safe and efficacious, however larger studies are required.
Disclosures:
Jay Patel indicated no relevant financial relationships.
Rishabh Khatri indicated no relevant financial relationships.
Jay Kanaparthi indicated no relevant financial relationships.
Jun Song indicated no relevant financial relationships.
Stephen Heller indicated no relevant financial relationships.
Woo Jung Jay Lee indicated no relevant financial relationships.
Frank Friedenberg indicated no relevant financial relationships.
Saraswathi Cappelle: Olympus – Consultant.
Jay B. Patel, MD1, Rishabh Khatri, MD1, Jay Kanaparthi, MD1, Jun Song, MD1, Stephen Heller, MD2, Woo Jung Jay Lee, MB, BCh, BAO2, Frank Friedenberg, MD, MS2, Saraswathi Cappelle, DO2. B0447 - Lumen-Apposing Metal Stents for Pancreatic Fluid Collections Reduce 90-Day Readmission Rates, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
