Back

Poster Session B - Monday Morning
Category: Interventional Endoscopy
B0482 - An Uncommon ERCP Complication: Delayed Uncovered Biliary Stent Migration into the Portal Vein in a Case of Locally Advanced Pancreatic Adenocarcinoma
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Ameen El-Swais, MD
University of Kansas School of Medicine
Wichita, KS
Presenting Author(s)
Ameen El-Swais, MD1, Bassem Matta, MD2
1University of Kansas School of Medicine, Wichita, KS; 2Kansas Gastroenterology, Wichita, KS
Introduction: ERCP with biliary stenting remains an important aspect of symptomatic and palliative management in malignant biliary obstruction. We wish to shed light on a newly reported complication of ERCP with biliary stenting demonstrated in a case of locally advanced pancreatic ductal adenocarcinoma (PDAC).
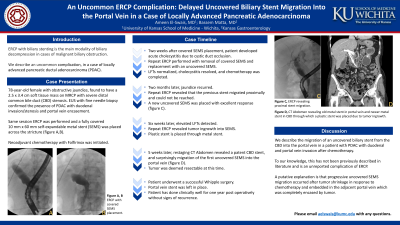
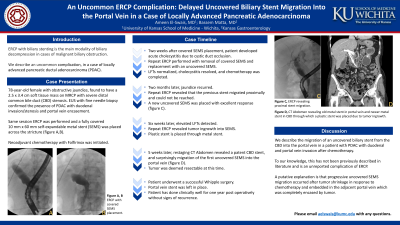
Case Description/Methods: We present a 78-year-old female with obstructive jaundice, found to have a 2.5 x 3.4 cm soft tissue mass on MRCP with proximal common bile duct (CBD) dilation and distal CBD narrowing. Initial attempt at ERCP failed due to duodenal stenosis (DS). Patient was referred to a therapeutic endoscopist where endoscopic ultrasound with fine needle biopsy confirmed the presence of PDAC with portal vein (PV) encasement and stenosis. Concurrent ERCP was successful after dilation of the DS, and a fully covered 10 mm x 60 mm self-expandable metal stent (SEMS) was placed into the CBD (Figure 1A, B). Neoadjuvant chemotherapy (CTX) was then initiated. Two weeks later, patient developed jaundice with acute cholecystitis thought to be related to cystic duct occlusion. Repeat ERCP was performed with removal of the covered stent and replacement with a similar size uncovered SEMS. The patient’s liver function tests (LFTs) normalized, cholecystitis resolved with antibiotics, and she was able to complete her CTX regimen. Jaundice recurred two months later, and a repeat ERCP revealed that the previous stent had migrated proximally and the previous DS had completely resolved. Biliary access was achieved, and a new uncovered SEMS was placed with excellent clinical response (Figure 1C). Due to repeat elevation in LFTs 1.5 months later, another ERCP was performed which revealed tumor ingrowth into the SEMS, and a plastic stent was placed through the metal stent. Five weeks later, CT scan showed a patent CBD stent, and surprisingly revealed migration of the first uncovered SEMS into the PV (Figure 1D). Patient underwent a successful Whipple procedure after CTX, with good recovery one year after surgery with the stent in place.
Discussion: We described the migration of an uncovered biliary stent into the PV in a patient with PDAC with duodenal and PV invasion after CTX, which is an unreported complication of ERCP biliary stenting. While it is unclear how this definitively occurred, a putative explanation is that partial distal uncovered SEMS migration occurred after tumor shrinkage in response to CTX and embedded in the adjacent PV which was completely encased by tumor.

Disclosures:
Ameen El-Swais, MD1, Bassem Matta, MD2. B0482 - An Uncommon ERCP Complication: Delayed Uncovered Biliary Stent Migration into the Portal Vein in a Case of Locally Advanced Pancreatic Adenocarcinoma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Kansas School of Medicine, Wichita, KS; 2Kansas Gastroenterology, Wichita, KS
Introduction: ERCP with biliary stenting remains an important aspect of symptomatic and palliative management in malignant biliary obstruction. We wish to shed light on a newly reported complication of ERCP with biliary stenting demonstrated in a case of locally advanced pancreatic ductal adenocarcinoma (PDAC).
Case Description/Methods: We present a 78-year-old female with obstructive jaundice, found to have a 2.5 x 3.4 cm soft tissue mass on MRCP with proximal common bile duct (CBD) dilation and distal CBD narrowing. Initial attempt at ERCP failed due to duodenal stenosis (DS). Patient was referred to a therapeutic endoscopist where endoscopic ultrasound with fine needle biopsy confirmed the presence of PDAC with portal vein (PV) encasement and stenosis. Concurrent ERCP was successful after dilation of the DS, and a fully covered 10 mm x 60 mm self-expandable metal stent (SEMS) was placed into the CBD (Figure 1A, B). Neoadjuvant chemotherapy (CTX) was then initiated. Two weeks later, patient developed jaundice with acute cholecystitis thought to be related to cystic duct occlusion. Repeat ERCP was performed with removal of the covered stent and replacement with a similar size uncovered SEMS. The patient’s liver function tests (LFTs) normalized, cholecystitis resolved with antibiotics, and she was able to complete her CTX regimen. Jaundice recurred two months later, and a repeat ERCP revealed that the previous stent had migrated proximally and the previous DS had completely resolved. Biliary access was achieved, and a new uncovered SEMS was placed with excellent clinical response (Figure 1C). Due to repeat elevation in LFTs 1.5 months later, another ERCP was performed which revealed tumor ingrowth into the SEMS, and a plastic stent was placed through the metal stent. Five weeks later, CT scan showed a patent CBD stent, and surprisingly revealed migration of the first uncovered SEMS into the PV (Figure 1D). Patient underwent a successful Whipple procedure after CTX, with good recovery one year after surgery with the stent in place.
Discussion: We described the migration of an uncovered biliary stent into the PV in a patient with PDAC with duodenal and PV invasion after CTX, which is an unreported complication of ERCP biliary stenting. While it is unclear how this definitively occurred, a putative explanation is that partial distal uncovered SEMS migration occurred after tumor shrinkage in response to CTX and embedded in the adjacent PV which was completely encased by tumor.

Figure: Figure 1: A,B) ERCP showing covered self-expandable metal stent (SEMS) placement. C) ERCP revealing proximal stent migration. D) CT revealing old metal stent in portal vein and newer metal stent in CBD through which a plastic stent was placed due to tumor ingrowth.
Disclosures:
Ameen El-Swais indicated no relevant financial relationships.
Bassem Matta indicated no relevant financial relationships.
Ameen El-Swais, MD1, Bassem Matta, MD2. B0482 - An Uncommon ERCP Complication: Delayed Uncovered Biliary Stent Migration into the Portal Vein in a Case of Locally Advanced Pancreatic Adenocarcinoma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

