Back

Poster Session B - Monday Morning
Category: Functional Bowel Disease
B0262 - The Clinical Impact of Brain-Gut Psychotherapy on Psychological Symptoms for Patients With Complex Gastrointestinal Disorders: Outcomes in a Real World Practice Setting
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
Elyse Thakur, PhD
Atrium Health
Charlotte, NC
Presenting Author(s)
Elyse Thakur, PhD1, Kenneth Koch, MD2, Mackenzie McArthur, MPAM, PA-C, DMSc3, Thomas Pacicco, MD1, Baharak Moshiree, MD, MSCI, FACG1
1Atrium Health, Charlotte, NC; 2Wake Forest University School of Medicine, Winston-Salem, NC; 3Atrium Health Wake Forest, Charlotte, NC
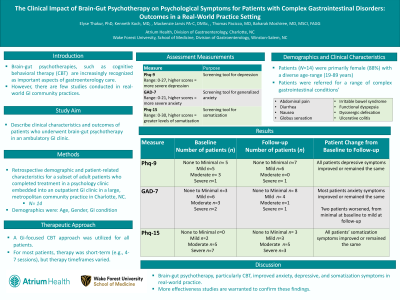
Introduction: Evidence-based brain-gut psychotherapies, such as cognitive behavioral therapy (CBT), are increasingly recognized as important aspects of gastroenterology (GI) care. However, there are few studies conducted in real-world GI community practices. Aim: To describe clinical characteristics and outcomes of patients who underwent brain-gut psychotherapy in an ambulatory GI clinic.
Methods: We retrospectively examined demographic and patient-related characteristics for a subset of patients who completed treatment in a psychology clinic embedded into an outpatient GI clinic in a large, metropolitan community practice. Depressive (Patient Health Questionnaire-9), anxiety (Generalized Anxiety Disorder-7) and somatization (Patient Health Questionnaire-15) symptoms were assessed.
Results: Patients (n=14) were primarily female (88%), with a diverse age-range (19-89 years). Patients were referred for complex gastrointestinal conditions; most had functional and/or motility and disorders and syndromes (i.e., IBS, functional dyspepsia, globus sensation, dyssenergic defection), and two patients had inflammatory bowel diseases. A GI-focused CBT approach was utilized for all patients. For most patients, therapy was short-term (e.g., 4-7 sessions), but therapy timeframes varied. At baseline, nine patients presented with depressive symptoms that ranged from mild (n=5) to moderate (n=3) to severe (n=1). At follow-up, depressive symptoms improved or remained the same; slightly half presented with mild symptoms (n=6), and one patient continued to have severe symptoms. At baseline, 11 patients presented with anxiety symptoms that ranged from mild (n=6) to moderate (n=3) to severe (n=2). At follow-up, anxiety symptoms improved or remained the same; only two patients presented with mild symptoms, and one patient continued to have severe symptoms. Two patients worsened, from minimal depressive symptoms at baseline to mild at follow-up. Somatization was the most elevated at baseline, with symptoms that ranged from mild (n=2), to moderate (n=5) to severe (n=7). At follow-up, all patients’ somatization symptoms improved or remained the same: three patients had mild symptoms, five were in the moderate range, and two remained severe.
Discussion: Brain-gut psychotherapy, particularly CBT, improved anxiety, depressive, and somatization symptoms in real-world practice. More effectiveness studies are warranted to confirm these findings.
Disclosures:
Elyse Thakur, PhD1, Kenneth Koch, MD2, Mackenzie McArthur, MPAM, PA-C, DMSc3, Thomas Pacicco, MD1, Baharak Moshiree, MD, MSCI, FACG1. B0262 - The Clinical Impact of Brain-Gut Psychotherapy on Psychological Symptoms for Patients With Complex Gastrointestinal Disorders: Outcomes in a Real World Practice Setting, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Atrium Health, Charlotte, NC; 2Wake Forest University School of Medicine, Winston-Salem, NC; 3Atrium Health Wake Forest, Charlotte, NC
Introduction: Evidence-based brain-gut psychotherapies, such as cognitive behavioral therapy (CBT), are increasingly recognized as important aspects of gastroenterology (GI) care. However, there are few studies conducted in real-world GI community practices. Aim: To describe clinical characteristics and outcomes of patients who underwent brain-gut psychotherapy in an ambulatory GI clinic.
Methods: We retrospectively examined demographic and patient-related characteristics for a subset of patients who completed treatment in a psychology clinic embedded into an outpatient GI clinic in a large, metropolitan community practice. Depressive (Patient Health Questionnaire-9), anxiety (Generalized Anxiety Disorder-7) and somatization (Patient Health Questionnaire-15) symptoms were assessed.
Results: Patients (n=14) were primarily female (88%), with a diverse age-range (19-89 years). Patients were referred for complex gastrointestinal conditions; most had functional and/or motility and disorders and syndromes (i.e., IBS, functional dyspepsia, globus sensation, dyssenergic defection), and two patients had inflammatory bowel diseases. A GI-focused CBT approach was utilized for all patients. For most patients, therapy was short-term (e.g., 4-7 sessions), but therapy timeframes varied. At baseline, nine patients presented with depressive symptoms that ranged from mild (n=5) to moderate (n=3) to severe (n=1). At follow-up, depressive symptoms improved or remained the same; slightly half presented with mild symptoms (n=6), and one patient continued to have severe symptoms. At baseline, 11 patients presented with anxiety symptoms that ranged from mild (n=6) to moderate (n=3) to severe (n=2). At follow-up, anxiety symptoms improved or remained the same; only two patients presented with mild symptoms, and one patient continued to have severe symptoms. Two patients worsened, from minimal depressive symptoms at baseline to mild at follow-up. Somatization was the most elevated at baseline, with symptoms that ranged from mild (n=2), to moderate (n=5) to severe (n=7). At follow-up, all patients’ somatization symptoms improved or remained the same: three patients had mild symptoms, five were in the moderate range, and two remained severe.
Discussion: Brain-gut psychotherapy, particularly CBT, improved anxiety, depressive, and somatization symptoms in real-world practice. More effectiveness studies are warranted to confirm these findings.
Disclosures:
Elyse Thakur: Mahana Therapeutics – Advisory Committee/Board Member.
Kenneth Koch indicated no relevant financial relationships.
Mackenzie McArthur: Abbvie – Speakers Bureau. Coloplast – Advisory Committee/Board Member. Evoke – Advisory Committee/Board Member. Phathom Pharmaceuticals – Advisory Committee/Board Member, Speakers Bureau. Salix Pharmaceuticals – Advisory Committee/Board Member, Speakers Bureau. Sanofi – Advisory Committee/Board Member.
Thomas Pacicco indicated no relevant financial relationships.
Baharak Moshiree indicated no relevant financial relationships.
Elyse Thakur, PhD1, Kenneth Koch, MD2, Mackenzie McArthur, MPAM, PA-C, DMSc3, Thomas Pacicco, MD1, Baharak Moshiree, MD, MSCI, FACG1. B0262 - The Clinical Impact of Brain-Gut Psychotherapy on Psychological Symptoms for Patients With Complex Gastrointestinal Disorders: Outcomes in a Real World Practice Setting, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
