Back

Poster Session B - Monday Morning
Category: IBD
B0356 - Trends in Hospitalization for Small Bowel Obstruction in Crohn’s Disease Patients: A Nationwide Analysis From 2008 to 2018
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- MT
Muhammad Waqas Tahir, MD
Rochester General Hospital
Rochester, NY
Presenting Author(s)
Muhammad Waqas Tahir, MD1, Raseen Tariq, MD2, Zoya Tahir, MD3, Sahil Khanna, MBBS, MS, FACG2
1Rochester General Hospital, Rochester, NY; 2Mayo Clinic, Rochester, MN; 3Gujrat Hospital, Bear, DE
Introduction: Small bowel obstruction (SBO) is a known complication of Crohn’s disease (CD). Over the last decade, there have been advances in management of CD including early treatment and newer immunosuppressives. The impact of these interventions on SBO remains unknown. We aim to study the trends in SBO related hospitalization in CD patients.
Methods: We used the National Inpatient Sample (NIS) database from 2008 to 2018 to identify patients with CD with concurrent diagnosis of SBO using ICD-9 and ICD-10 codes. We calculated trends in nationwide estimates for annual admissions, length of stay (LOS), in-patient mortality and complications of SBO including mortality, peritonitis and sepsis. We used the Cochran-Armitage test for trend significance. We used logistic regression to identify predictors of mortality among these admissions.
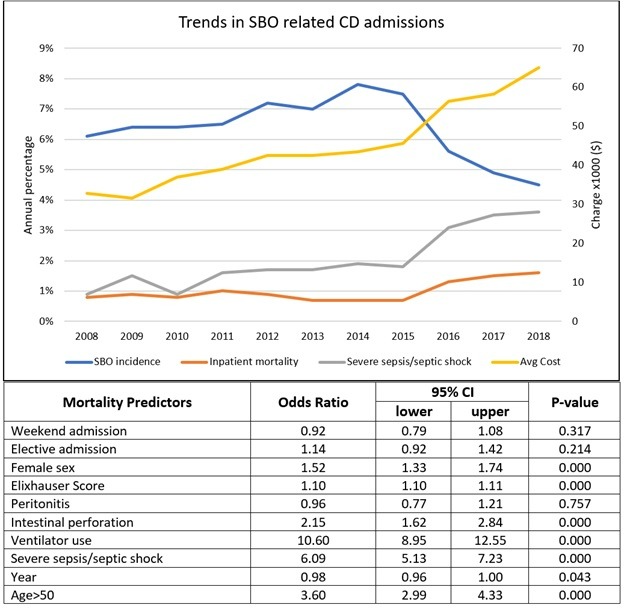
Results: There were a total of 2,195,512 admissions with CD between 2008 and 2018. Of those SBO accounted for 139,440 (6.78%) of these admissions. Of the patients admitted with SBO, the average age was 50 years and 52.6% were female. There was an increase in Elixhauser comorbidity index from a mean score of 3.0 in 2008 to 5.2 in 2018 (p< 0.001). There was a rising proportion of SBO cases among all CD admissions initially, rising from 6.0% in 2008 to a peak of 7.8% in 2014, followed by a significant decline down to 4.5% in 2018.
Overall, 88.8% of SBO related admissions were emergent, with an increasing trend (from 86.1% to 92.3%, p-trend< 0.001) signifying more emergent admissions recently. The median LOS was 4 days, with a decrease from 4 days in 2008 period to 3 days in 2018. The overall mortality was 1.0%, with a stable trend until 2015 but an increase during last 3 years to 1.6% (p-trend< 0.001). There were no changes in the proportion with peritonitis (mean 3.3%) or intestinal perforation (mean 1.3%). Severe/sepsis/septic shock was present in 1.9% cases overall with an increasing rising proportion from 0.9% to 3.6% (p-trend< 0.001). Regression analysis showed ventilator use (OR 10.6, 95% CI 8.9 – 12.6), severe sepsis/septic shock (OR 6.1, 95% CI 5.1 – 7.3), age >50 (OR 3.4, 95% CI 3.0 – 4.3), intestinal perforation (OR 2.1, 95% CI 1.6 – 2.8) and female sex (OR1.5, 95% CI 1.3 – 1.7) were significant predictors of inpatient mortality.
Discussion: SBO remains a known complication of Crohn’s disease. The proportion of CD patients with SBO seem to be decreasing but among these patients, inpatient mortality seems to be increasing which needs further investigation
Disclosures:
Muhammad Waqas Tahir, MD1, Raseen Tariq, MD2, Zoya Tahir, MD3, Sahil Khanna, MBBS, MS, FACG2. B0356 - Trends in Hospitalization for Small Bowel Obstruction in Crohn’s Disease Patients: A Nationwide Analysis From 2008 to 2018, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Rochester General Hospital, Rochester, NY; 2Mayo Clinic, Rochester, MN; 3Gujrat Hospital, Bear, DE
Introduction: Small bowel obstruction (SBO) is a known complication of Crohn’s disease (CD). Over the last decade, there have been advances in management of CD including early treatment and newer immunosuppressives. The impact of these interventions on SBO remains unknown. We aim to study the trends in SBO related hospitalization in CD patients.
Methods: We used the National Inpatient Sample (NIS) database from 2008 to 2018 to identify patients with CD with concurrent diagnosis of SBO using ICD-9 and ICD-10 codes. We calculated trends in nationwide estimates for annual admissions, length of stay (LOS), in-patient mortality and complications of SBO including mortality, peritonitis and sepsis. We used the Cochran-Armitage test for trend significance. We used logistic regression to identify predictors of mortality among these admissions.
Results: There were a total of 2,195,512 admissions with CD between 2008 and 2018. Of those SBO accounted for 139,440 (6.78%) of these admissions. Of the patients admitted with SBO, the average age was 50 years and 52.6% were female. There was an increase in Elixhauser comorbidity index from a mean score of 3.0 in 2008 to 5.2 in 2018 (p< 0.001). There was a rising proportion of SBO cases among all CD admissions initially, rising from 6.0% in 2008 to a peak of 7.8% in 2014, followed by a significant decline down to 4.5% in 2018.
Overall, 88.8% of SBO related admissions were emergent, with an increasing trend (from 86.1% to 92.3%, p-trend< 0.001) signifying more emergent admissions recently. The median LOS was 4 days, with a decrease from 4 days in 2008 period to 3 days in 2018. The overall mortality was 1.0%, with a stable trend until 2015 but an increase during last 3 years to 1.6% (p-trend< 0.001). There were no changes in the proportion with peritonitis (mean 3.3%) or intestinal perforation (mean 1.3%). Severe/sepsis/septic shock was present in 1.9% cases overall with an increasing rising proportion from 0.9% to 3.6% (p-trend< 0.001). Regression analysis showed ventilator use (OR 10.6, 95% CI 8.9 – 12.6), severe sepsis/septic shock (OR 6.1, 95% CI 5.1 – 7.3), age >50 (OR 3.4, 95% CI 3.0 – 4.3), intestinal perforation (OR 2.1, 95% CI 1.6 – 2.8) and female sex (OR1.5, 95% CI 1.3 – 1.7) were significant predictors of inpatient mortality.
Discussion: SBO remains a known complication of Crohn’s disease. The proportion of CD patients with SBO seem to be decreasing but among these patients, inpatient mortality seems to be increasing which needs further investigation
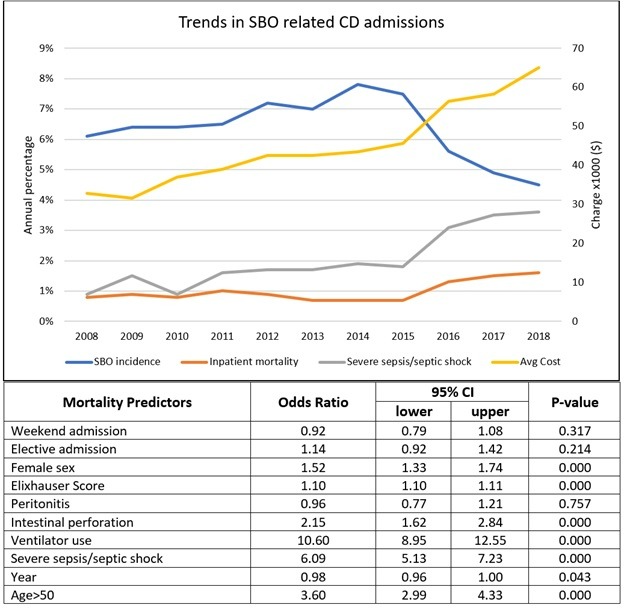
Figure: Figure 1. Top half shows trend lines for incidence of SBO in CD patients, their inpatient mortality, rate of severe sepsis/septic shock and cost of hospitalization (adjusted for inflation). Bottom half depicting predictors of inpatient mortality using regression analysis.
Disclosures:
Muhammad Waqas Tahir indicated no relevant financial relationships.
Raseen Tariq indicated no relevant financial relationships.
Zoya Tahir indicated no relevant financial relationships.
Sahil Khanna: Ferring Pharmaceuticals – Grant/Research Support. Finch – Grant/Research Support. Niche – Consultant. Pfizer – Grant/Research Support. Probiotech – Consultant. Seres Therapeutics – Grant/Research Support. Takeda/Shire – Consultant. Vedanta – Grant/Research Support.
Muhammad Waqas Tahir, MD1, Raseen Tariq, MD2, Zoya Tahir, MD3, Sahil Khanna, MBBS, MS, FACG2. B0356 - Trends in Hospitalization for Small Bowel Obstruction in Crohn’s Disease Patients: A Nationwide Analysis From 2008 to 2018, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
