Back

Poster Session A - Sunday Afternoon
Category: General Endoscopy
A0270 - Biopsy Results Follow-Up After Outpatient Endoscopy: A Survey of Patient Preferences
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio
Kwabena O. Adu-Gyamfi, MBChB
Medical College of Georgia - Augusta University
Augusta, GA
Presenting Author(s)
Kwabena O. Adu-Gyamfi, MBChB1, Dariush Shahsavari, MD1, Jennifer Rooks, BSN2, Kenneth J. Vega, MD, FACG3, Viveksandeep Chandrasekar, MBBS3, Zain A. Sobani, MD4, John Erikson L. Yap, MD3
1Medical College of Georgia - Augusta University, Augusta, GA; 2Augusta University Medical Center, Augusta, GA; 3Augusta University Medical College of Georiga, Augusta, GA; 4Augusta University/Medical College of Georgia, Augusta, GA
Introduction: Effective communication is the cornerstone of healthcare delivery and patient satisfaction. Good communication between patient and physician has been demonstrated to increase adherence to treatment along with follow-up plans. Open access endoscopy, while achieving the goal of increasing screening rates poses a challenge in providing patients with pathology results from specimens obtained during the procedure. Institutions have implemented a variety of strategies to communicate such results to patients. We conducted a survey of patients undergoing outpatient endoscopy at our center to assess their preferences for obtaining pathology results.
Methods: All outpatients presenting to our institution for endoscopy for 30 consecutive days were approached for participation in this quality improvement (QI) project. A one-question survey assessed the patient’s preferred communication method of pathology results.
The options included phone visit, letter, email, telehealth and in person clinic visit. Demographics assessed included age, gender, race and educational level.
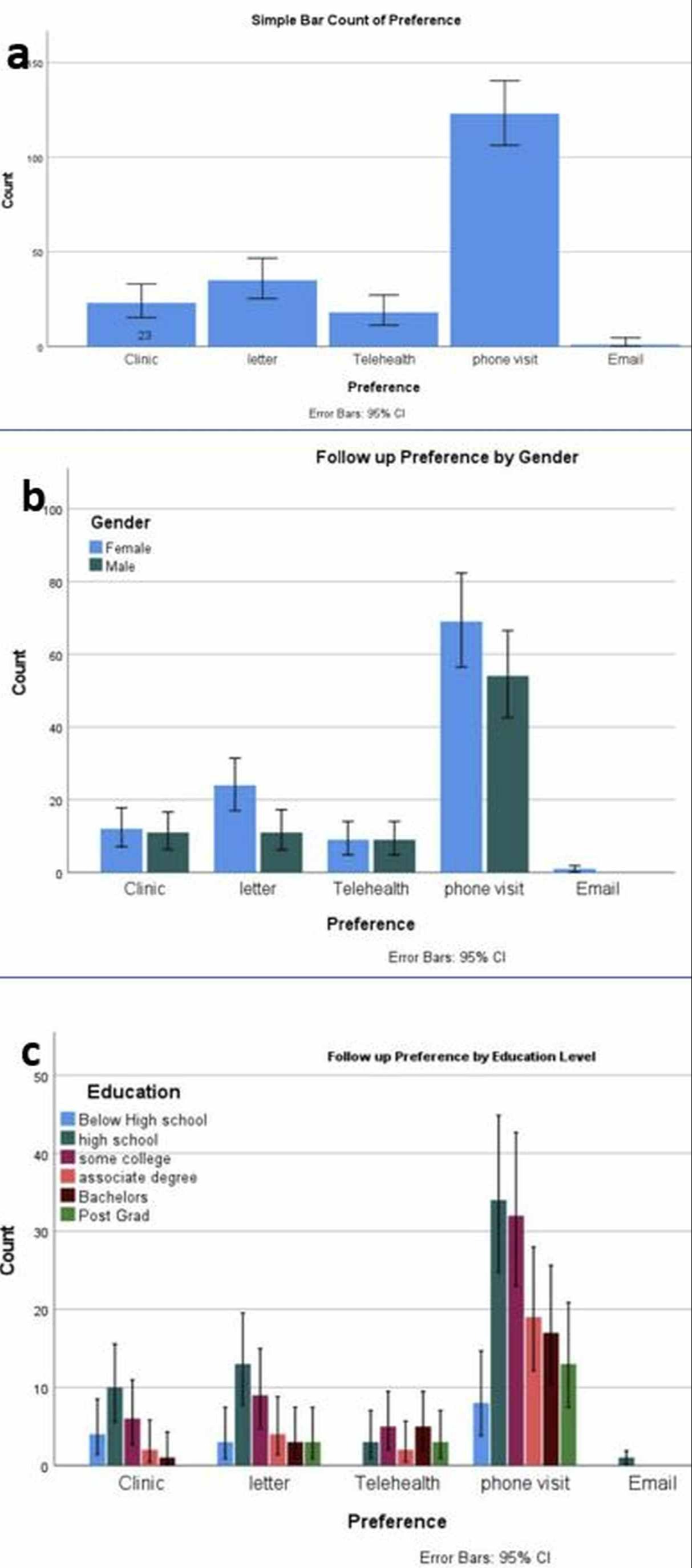
Results: A total of 200 patients presenting to our outpatient endoscopy suite during the period of interest completed the QI survey instrument and comprise the study group. Demographics were as follows: female 57.5%, male 42.5%; Age ranges in years - 18-40 (11.5%), 41-60 (44.5%) & >60 (44%); race - African American 51%, Caucasian 44%, Asian 2.5%, Hispanic 1% & Other 1.5%; Educational level - below high school 7.5%, high school 30.5%, some college 26%, Associates degree 13.5%, Bachelor’s degree 13% & Pos- graduate 9.5%. The preferred follow up method was phone visit (61.5%) followed by letter, in person clinic visit, telehealth & email (figure 1a). This was not influenced by age, gender (Fig 1b), race or educational level (Fig 1c) on univariate/multivariate regression models.
Discussion: The current QI study indicates patients preferred telephone follow up to other post-procedure communication methods. We believe this is due to direct discussion with a provider, enabling better understanding of results along with time-related flexibility from a phone visit. However, implementation
may increase physician workload. In addition, communication using a patient preferred intervention may yield significant increases in patient practice satisfaction. These preliminary results should be confirmed using larger patient cohorts and assess the role of GI advanced practice providers in this process.
Disclosures:
Kwabena O. Adu-Gyamfi, MBChB1, Dariush Shahsavari, MD1, Jennifer Rooks, BSN2, Kenneth J. Vega, MD, FACG3, Viveksandeep Chandrasekar, MBBS3, Zain A. Sobani, MD4, John Erikson L. Yap, MD3. A0270 - Biopsy Results Follow-Up After Outpatient Endoscopy: A Survey of Patient Preferences, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Medical College of Georgia - Augusta University, Augusta, GA; 2Augusta University Medical Center, Augusta, GA; 3Augusta University Medical College of Georiga, Augusta, GA; 4Augusta University/Medical College of Georgia, Augusta, GA
Introduction: Effective communication is the cornerstone of healthcare delivery and patient satisfaction. Good communication between patient and physician has been demonstrated to increase adherence to treatment along with follow-up plans. Open access endoscopy, while achieving the goal of increasing screening rates poses a challenge in providing patients with pathology results from specimens obtained during the procedure. Institutions have implemented a variety of strategies to communicate such results to patients. We conducted a survey of patients undergoing outpatient endoscopy at our center to assess their preferences for obtaining pathology results.
Methods: All outpatients presenting to our institution for endoscopy for 30 consecutive days were approached for participation in this quality improvement (QI) project. A one-question survey assessed the patient’s preferred communication method of pathology results.
The options included phone visit, letter, email, telehealth and in person clinic visit. Demographics assessed included age, gender, race and educational level.
Results: A total of 200 patients presenting to our outpatient endoscopy suite during the period of interest completed the QI survey instrument and comprise the study group. Demographics were as follows: female 57.5%, male 42.5%; Age ranges in years - 18-40 (11.5%), 41-60 (44.5%) & >60 (44%); race - African American 51%, Caucasian 44%, Asian 2.5%, Hispanic 1% & Other 1.5%; Educational level - below high school 7.5%, high school 30.5%, some college 26%, Associates degree 13.5%, Bachelor’s degree 13% & Pos- graduate 9.5%. The preferred follow up method was phone visit (61.5%) followed by letter, in person clinic visit, telehealth & email (figure 1a). This was not influenced by age, gender (Fig 1b), race or educational level (Fig 1c) on univariate/multivariate regression models.
Discussion: The current QI study indicates patients preferred telephone follow up to other post-procedure communication methods. We believe this is due to direct discussion with a provider, enabling better understanding of results along with time-related flexibility from a phone visit. However, implementation
may increase physician workload. In addition, communication using a patient preferred intervention may yield significant increases in patient practice satisfaction. These preliminary results should be confirmed using larger patient cohorts and assess the role of GI advanced practice providers in this process.
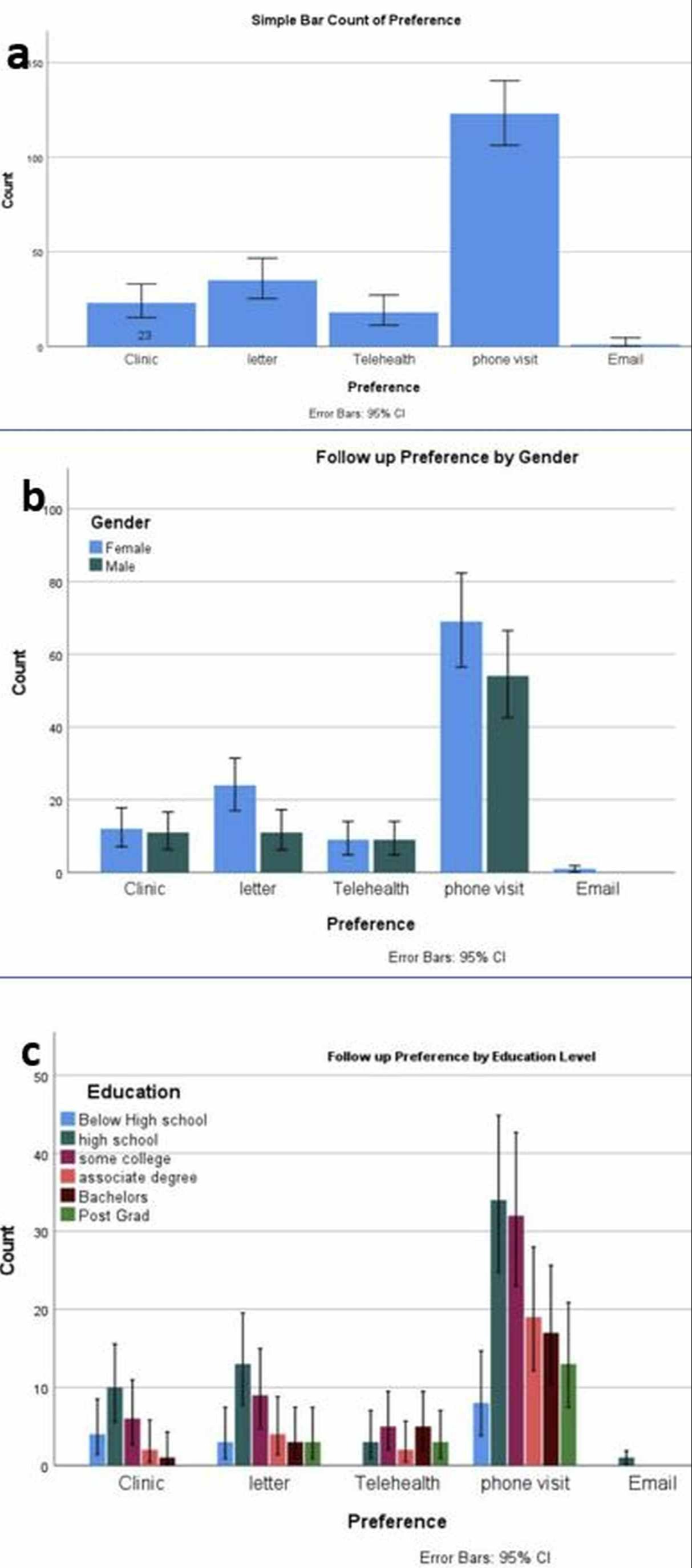
Figure: Fig 1. Patient preferences for post-endoscopy biopsy results follow-up (Fig 1a). Patient preference by gender (Fig 1b). Patient preference by educational level (Fig 1c).
Disclosures:
Kwabena Adu-Gyamfi indicated no relevant financial relationships.
Dariush Shahsavari indicated no relevant financial relationships.
Jennifer Rooks indicated no relevant financial relationships.
Kenneth Vega indicated no relevant financial relationships.
Viveksandeep Chandrasekar indicated no relevant financial relationships.
Zain Sobani indicated no relevant financial relationships.
John Erikson Yap indicated no relevant financial relationships.
Kwabena O. Adu-Gyamfi, MBChB1, Dariush Shahsavari, MD1, Jennifer Rooks, BSN2, Kenneth J. Vega, MD, FACG3, Viveksandeep Chandrasekar, MBBS3, Zain A. Sobani, MD4, John Erikson L. Yap, MD3. A0270 - Biopsy Results Follow-Up After Outpatient Endoscopy: A Survey of Patient Preferences, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

