Back
Poster Session B - Monday Morning
Category: Liver
B0588 - A Case of Pyogenic Liver Abscesses and Pylephlebitis With Sigmoidal Diverticulitis
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Aaron Fein, DO
University of Kentucky
Lexington, KY
Presenting Author(s)
Aaron Fein, DO1, Fatai Akemokwe, MD1, Mansi Parekh, MD1, Donald R. Campbell, MD2, Kristen E. Fletcher, MD3
1University of Kentucky, Lexington, KY; 2The University of Kentucky, Lexington, KY; 3Lexington VA Health Care & University of Kentucky College of Medicine, Lexington, KY
Introduction: Pyogenic liver abscesses (PLA) are suppurative infections in the hepatic parenchyma with high mortality. Risk factors include diabetes mellitus, underlying hepatic/biliary disease, and gastrointestinal malignancy. It is hypothesized that diverticular disease leads to disruption of the colonic mucosa, facilitating bacterial translocation into the portal venous system. We present a patient with acute sigmoidal diverticulitis complicated by pyogenic liver abscesses and septic portal vein thrombosis.
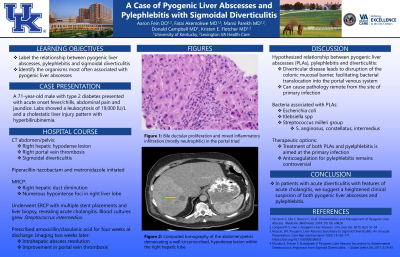
Case Description/Methods: A 71-year-old male with type 2 diabetes presented with acute onset fevers/chills, abdominal pain, and jaundice. Labs showed a leukocytosis of 19,000 IU/L and a cholestatic liver injury pattern with hyperbilirubinemia. CT abdomen and pelvis revealed right portal vein thrombosis, a right hepatic hypodense lesion, and concurrent sigmoidal diverticulitis. He was started empirically on piperacillin-tazobactam and metronidazole. E. histolytica serology and AFP were negative. MRCP demonstrated right hepatic duct diminution and numerous hyperintense foci in the right liver lobe. He underwent ECRP with multiple stent placements and liver biopsy, revealing acute cholangitis. Blood cultures grew Streptococcus intermedius. At discharge, he was prescribed amoxicillin/clavulanic acid for four weeks. At follow up two weeks later, imaging showed intrahepatic abscess resolution and interval improvement in portal vein thrombosis.
Discussion: Many case reports illustrate a relationship between pyogenic liver abscesses and sigmoidal diverticulitis. Although Escherichia coli and Klebsiella spp. are the predominate pathogens in PLA, the Streptococcus milleri group (including S. intermedius) are well documented as culprits. As seen in our patient, pylephlebitis is a known consequence of diverticulitis and treatment is aimed at the primary infection; anticoagulation remains controversial. In patients with acute diverticulitis with features of acute cholangitis, we suggest a heightened consideration of both pyogenic liver abscess and pylephlebitis.
1. Serraino C, Elia C, Bracco C, et al. Characteristics and Management of Pyogenic Liver Abscess. Medicine (Baltimore). 2018; 97(19): e0628
2. Muscat, E. Pyogenic Liver Abscess Secondary to Sigmoid Diverticulitis: An Unusual Presentation. Case Rep Gastroenterol. 2020; 14: 165-171
3. Wu, M, Schuster, M, Tadros, M. Update on Management of Portal Vein Thrombosis and the Role of Novel Anticoagulants. J Clin Transl Hepatol. 2019; 7(2): 154-164
Disclosures:
Aaron Fein, DO1, Fatai Akemokwe, MD1, Mansi Parekh, MD1, Donald R. Campbell, MD2, Kristen E. Fletcher, MD3. B0588 - A Case of Pyogenic Liver Abscesses and Pylephlebitis With Sigmoidal Diverticulitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Kentucky, Lexington, KY; 2The University of Kentucky, Lexington, KY; 3Lexington VA Health Care & University of Kentucky College of Medicine, Lexington, KY
Introduction: Pyogenic liver abscesses (PLA) are suppurative infections in the hepatic parenchyma with high mortality. Risk factors include diabetes mellitus, underlying hepatic/biliary disease, and gastrointestinal malignancy. It is hypothesized that diverticular disease leads to disruption of the colonic mucosa, facilitating bacterial translocation into the portal venous system. We present a patient with acute sigmoidal diverticulitis complicated by pyogenic liver abscesses and septic portal vein thrombosis.
Case Description/Methods: A 71-year-old male with type 2 diabetes presented with acute onset fevers/chills, abdominal pain, and jaundice. Labs showed a leukocytosis of 19,000 IU/L and a cholestatic liver injury pattern with hyperbilirubinemia. CT abdomen and pelvis revealed right portal vein thrombosis, a right hepatic hypodense lesion, and concurrent sigmoidal diverticulitis. He was started empirically on piperacillin-tazobactam and metronidazole. E. histolytica serology and AFP were negative. MRCP demonstrated right hepatic duct diminution and numerous hyperintense foci in the right liver lobe. He underwent ECRP with multiple stent placements and liver biopsy, revealing acute cholangitis. Blood cultures grew Streptococcus intermedius. At discharge, he was prescribed amoxicillin/clavulanic acid for four weeks. At follow up two weeks later, imaging showed intrahepatic abscess resolution and interval improvement in portal vein thrombosis.
Discussion: Many case reports illustrate a relationship between pyogenic liver abscesses and sigmoidal diverticulitis. Although Escherichia coli and Klebsiella spp. are the predominate pathogens in PLA, the Streptococcus milleri group (including S. intermedius) are well documented as culprits. As seen in our patient, pylephlebitis is a known consequence of diverticulitis and treatment is aimed at the primary infection; anticoagulation remains controversial. In patients with acute diverticulitis with features of acute cholangitis, we suggest a heightened consideration of both pyogenic liver abscess and pylephlebitis.
1. Serraino C, Elia C, Bracco C, et al. Characteristics and Management of Pyogenic Liver Abscess. Medicine (Baltimore). 2018; 97(19): e0628
2. Muscat, E. Pyogenic Liver Abscess Secondary to Sigmoid Diverticulitis: An Unusual Presentation. Case Rep Gastroenterol. 2020; 14: 165-171
3. Wu, M, Schuster, M, Tadros, M. Update on Management of Portal Vein Thrombosis and the Role of Novel Anticoagulants. J Clin Transl Hepatol. 2019; 7(2): 154-164
Disclosures:
Aaron Fein indicated no relevant financial relationships.
Fatai Akemokwe indicated no relevant financial relationships.
Mansi Parekh indicated no relevant financial relationships.
Donald Campbell indicated no relevant financial relationships.
Kristen Fletcher indicated no relevant financial relationships.
Aaron Fein, DO1, Fatai Akemokwe, MD1, Mansi Parekh, MD1, Donald R. Campbell, MD2, Kristen E. Fletcher, MD3. B0588 - A Case of Pyogenic Liver Abscesses and Pylephlebitis With Sigmoidal Diverticulitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
