Back

Poster Session B - Monday Morning
Category: Small Intestine
B0677 - Biopsy-Confirmed Celiac Disease After COVID-19 Infection
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
.jpg)
Mahmoud Aryan, MD
University of Alabama at Birmingham
Birmingham, AL
Presenting Author(s)
Mahmoud Aryan, MD1, Dane Johnson, MD1, Chirag Patel, MD2, Amanda Cartee, MD1
1University of Alabama at Birmingham, Birmingham, AL; 2University of Alabama Birmingham, Birmingham, AL
Introduction: Post-COVID gastrointestinal (GI) symptoms are increasingly common in clinical practice and can sometimes overlap with other common, treatable GI disorders, such as Celiac Disease (CeD). We present the case of post-COVID GI symptoms subsequently diagnosed with CeD.
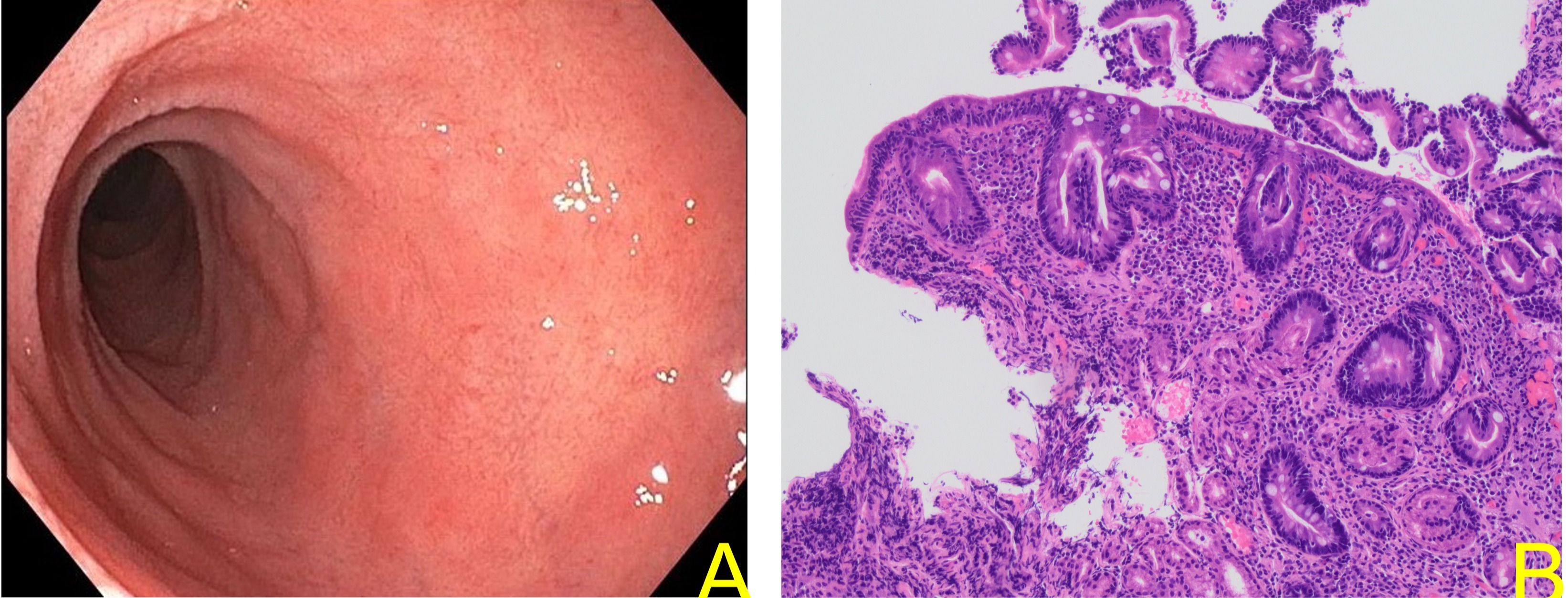
Case Description/Methods: A 28-year-old man with no prior medical history presented with nausea, vomiting, poor appetite, and weight loss after recovery from PCR-confirmed COVID-19 infection. Family history is remarkable for a sibling with type 1 diabetes mellitus. He endorsed an unintentional 40-pound weight loss with fatigue over the past 4 months, but he denied any constipation or loose stools. Family history is remarkable for a sibling with type 1 diabetes mellitus. He sought emergent care twice prior to being referred to gastroenterology clinic at which time abdominal imaging was unremarkable. Symptoms did not improve with a trial of proton pump inhibitors. Physical exam at time of consultation was remarkable for obesity. Laboratory work revealed elevated tissue transglutaminase IgA 57 U/mL (normal < 19 U/mL). He was also found to be deficient in vitamin D, vitamin B12, and folate. Upper endoscopy revealed duodenal scalloping and atrophy (figure 1A) where biopsies confirmed CeD, Marsh 3B (figure 1B). He was started on a gluten free diet and his symptoms resolved. Tissue transglutaminase IgA normalized (9 U/mL) within 6 months of making dietary changes.
Discussion: Post-COVID symptoms are overall varied and non-specific with potential to overlap with other GI conditions. There has been a reported increased prevalence of CeD in all age groups during the SARS-CoV-2 pandemic1. SARS-CoV2 enters mucosal membranes via angiotensin-converting enzyme 2, which is present in the small bowel mucosa2. Our case highlights that weight loss, and other “red flag” symptoms should prompt further evaluation despite being a common post-COVID symptom. We contemplate what role, SARS-CoV-2 could have had in disrupting small bowel mucosa integrity, potentially leading to CeD in genetically susceptible individuals.
1. Trovato CM et al. COVID‐19 and celiac disease: A pathogenetic hypothesis for a celiac outbreak. International Journal of Clinical Practice. 2021;75(9).
2. Hoffman M et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181(2):271-280.
Disclosures:
Mahmoud Aryan, MD1, Dane Johnson, MD1, Chirag Patel, MD2, Amanda Cartee, MD1. B0677 - Biopsy-Confirmed Celiac Disease After COVID-19 Infection, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Alabama at Birmingham, Birmingham, AL; 2University of Alabama Birmingham, Birmingham, AL
Introduction: Post-COVID gastrointestinal (GI) symptoms are increasingly common in clinical practice and can sometimes overlap with other common, treatable GI disorders, such as Celiac Disease (CeD). We present the case of post-COVID GI symptoms subsequently diagnosed with CeD.
Case Description/Methods: A 28-year-old man with no prior medical history presented with nausea, vomiting, poor appetite, and weight loss after recovery from PCR-confirmed COVID-19 infection. Family history is remarkable for a sibling with type 1 diabetes mellitus. He endorsed an unintentional 40-pound weight loss with fatigue over the past 4 months, but he denied any constipation or loose stools. Family history is remarkable for a sibling with type 1 diabetes mellitus. He sought emergent care twice prior to being referred to gastroenterology clinic at which time abdominal imaging was unremarkable. Symptoms did not improve with a trial of proton pump inhibitors. Physical exam at time of consultation was remarkable for obesity. Laboratory work revealed elevated tissue transglutaminase IgA 57 U/mL (normal < 19 U/mL). He was also found to be deficient in vitamin D, vitamin B12, and folate. Upper endoscopy revealed duodenal scalloping and atrophy (figure 1A) where biopsies confirmed CeD, Marsh 3B (figure 1B). He was started on a gluten free diet and his symptoms resolved. Tissue transglutaminase IgA normalized (9 U/mL) within 6 months of making dietary changes.
Discussion: Post-COVID symptoms are overall varied and non-specific with potential to overlap with other GI conditions. There has been a reported increased prevalence of CeD in all age groups during the SARS-CoV-2 pandemic1. SARS-CoV2 enters mucosal membranes via angiotensin-converting enzyme 2, which is present in the small bowel mucosa2. Our case highlights that weight loss, and other “red flag” symptoms should prompt further evaluation despite being a common post-COVID symptom. We contemplate what role, SARS-CoV-2 could have had in disrupting small bowel mucosa integrity, potentially leading to CeD in genetically susceptible individuals.
1. Trovato CM et al. COVID‐19 and celiac disease: A pathogenetic hypothesis for a celiac outbreak. International Journal of Clinical Practice. 2021;75(9).
2. Hoffman M et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181(2):271-280.
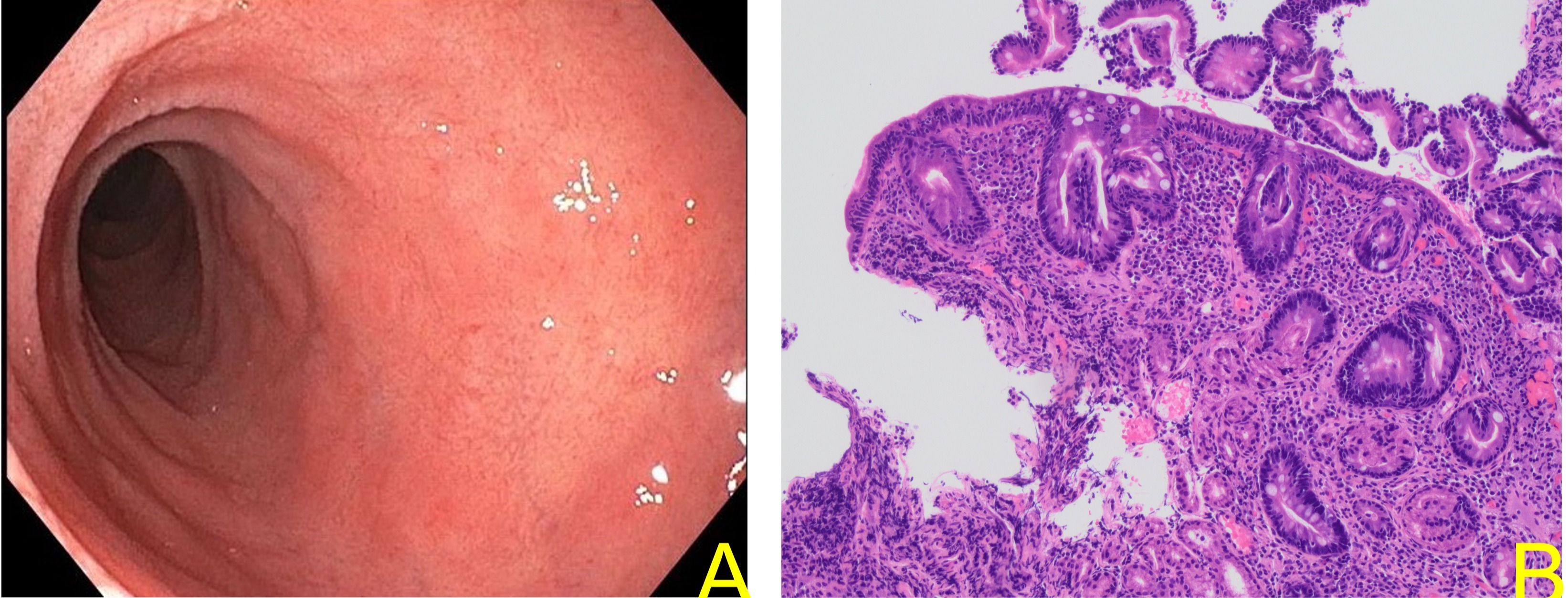
Figure: A: Duodenal scalloping and atrophy on upper endoscopy B: Subtotal villous atrophy, Marsh 3B
Disclosures:
Mahmoud Aryan indicated no relevant financial relationships.
Dane Johnson indicated no relevant financial relationships.
Chirag Patel indicated no relevant financial relationships.
Amanda Cartee: Alimentiv, Inc – Advisory Committee/Board Member. Equillium, Inc – Consultant.
Mahmoud Aryan, MD1, Dane Johnson, MD1, Chirag Patel, MD2, Amanda Cartee, MD1. B0677 - Biopsy-Confirmed Celiac Disease After COVID-19 Infection, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
